Abstract
Introduction
Pilonidal disease is a benign anorectal inflammatory disease that involves the subcutaneous adipose tissue overlying the sacrococcygeal region.
The aim of the work
The current study aimed to assess the value of preoperative evaluation of pilonidal disease and the exclusion of perianal sepsis using superficial parts ultrasonography and endoanal ultrasound.
Methodology
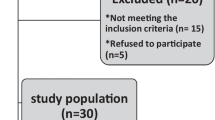
Referred 30 patients were clinically diagnosed as pilonidal disease, all were examined with superficial parts ultrasonography and if the disease was extending to the perianal region further endoanal US was performed to exclude perianal sepsis.
Results
7 patients showed subcutaneous abscesses and 23 patients showed pilonidal sinus tracts. Among patients with pilonidal sinus tracts, six tracts (26 %) seen as superficially situated, short narrow tracts with straight course, no side branches and with a blind end situated away from the anal canal wall. 2 (9 %) tracts showed vertical orientation and three tracts (13 %) were wide and deeply situated reaching the presacral fascia. 7 cases (30 %) showed branching pilonidal sinus tracts, two cases of them showed more than one external opening. 5 patients (22 %) showed abnormally long tracts seen reaching the perianal region.
Conclusion
Ultrasonography is an available, inexpensive, safe imaging modality that yields a high degree of accuracy in evaluating pilonidal disease and in exclusion of perianal sepsis.
Riassunto
Introduzione
La malattia pilonidale (PND) è una patologia infiammatoria ano-rettale benigna che coinvolge il tessuto adiposo sottocutaneo sovrastante la regione sacro-coccigea.
Scopo
scopo dello studio è stato evidenziare il ruolo dell’ecografia delle parti molli ed endorettale nella valutazione preoperatoria della malattia pilonidale e nell’escludere la sepsi perianale.
Materiali e Metodi
sono stati presi in esame 30 pazienti ai quali era stata diagnosticata clinicamente la malattia pilonidale, tutti sono stati sottoposti ad esame ecografico delle parti molli, se la malattia si era diffusa anche alla regione perianale, sono stati ulteriormente sottoposti ad esame ecografico endorettale per escludere sepsi perianale.
Risultati
7 pazienti mostravano ascessi sottocutanei e 23 cisti pilonidali. Tra questi ultimi, 6 (26 %) presentavano cisti con localizzazione superficiale, a decorso stretto e lineare, senza ramificazioni laterali e con un fondo cieco situato lontano dalla parete del canale anale. 2 pazienti (9 %) mostravano cisti ad orientamento verticale e 3 (13 %) sito ampio e profondo fino a raggiungere la fascia presacrale. 7 casi (30 %) mostravano ramificazione delle fistole pilonidali, di cui 2 con più di un’apertura esterna. 5 casi (22 %) cisti estremamente lunghe fino a raggiungere la regione perianale.
Conclusione
L’ecografia è una modalità d’indagine economica e sicura con un alto grado di precisione nella valutazione della malattia pilonidale e nell’esclusione la sepsi perianale.











Similar content being viewed by others
References
Bendewald FP, Cima RR (2007) Pilonidal disease. Clin Colon Rectal Surg 20(2):86–95
Richard A, Raffman A (1959) Re-evaluation of the pathogenesis of pilonidal sinus. Ann Surg 150(5):895–903
Can MF, Sevinc MM, Yilmaz M (2009) Comparison of Karydakis flap reconstruction versus primary midline closure in sacrococcygeal pilonidal disease: results of 200 military service members. Surg Today 39(7):580–586
Onder A, Girgin S, Kapan M, Toker M, Arikanoglu Z, Palanci Y, Bac B (2012) Pilonidal sinus disease: risk factors for postoperative complications and recurrence. Int Surg 97(3):224–229
Karydakis GE (1992) Easy and successful treatment of pilonidal sinus after explanation of its causative process. ANZ J Surg 62:385–389
da Silva JH (2000) Pilonidal cyst. Causes and treatment. Dis Colon Rectum 43:1146–1156
Kronberg I, Christensen KI, Zimmerman-Nielson O (1986) Chronic pilonidal disease: a randomised trial with complete three year follow up. Br J Surg 72:303–304
Sondenaa K, Diab R, Nesvik I et al (2002) Influence of failure of primary wound healing on subsequent recurrence of pilonidal sinus. Eur J Surg 168(11):614–618
Lee HC, Ho YH, Seow CF, Eu KW, Nyam D (2000) Pilonidal disease in Singapore: clinical features and management. Aust N Z J Surg 70(3):196–198
Mentes BB, Leventoglu S, Cihan A, Tatlicioglu E, Akin M, Oguz M (2004) Modified Limberg transposition flap for sacrococcygeal pilonidal sinus. Surg Today 34(5):419–423
Cihan A, Mentes BB, Tatlicioglu E, Ozmen S, Leventoglu S, Ucan BH (2004) Modified Limberg flap reconstruction compares favorably with primary repair for pilonidal sinus surgery. ANZ J Surg 74(4):238–242
Sozen S, Ozturk V, Das K, Erdem H, Cetinkunar S, Bal I (2012) Day-care surgery for pilonidal sinus using sinotomy technique and fibrin glue injection. Arch Clin Exp Surg 1(3):138–141
Mentes O, Oysul A, Harlak A, Zeybek N, Kozak O, Tufan T (2009) Ultrasonography accurately evaluates the dimension and shape of the pilonidal sinus. Clinics 64(3):189–192
Taylo SA, Halligan S, Bartram CI (2003) Pilonidal sinus disease: MR imaging distinction from fistula in ano. Radiology 226(3):662–667
McCallum IJD, King PM, Bruce J (2008) Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ 336:868–871
Mahdy T (2008) Surgical treatment of the pilonidal disease: primary closure or flap reconstruction after excision. Dis Colon Rectum 51(12):1816–1822
Ziech M, Felt-Bersma R, Stoker J (2009) Imaging of perianal fistulas. Clin Gastroenterol Hepatol 7:1037–1045
Kulacoglu H, Dener C, Tumer H, Aktimur R (2006) Total subcutaneous fistulectomy combined with Karydakis flap for sacrococcygeal pilonidal disease with secondary perianal opening. Colorectal Dis 8:120–123
Akinci OF, Coskun A, Ozgonul A, Terzi A (2006) Surgical treatment of complicated pilonidal disease: limited separate elliptical excision with primary closure. Colorectal Dis 8:704–749
Conflict of interest
The author declares that he has no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). All patients provided written informed consent to enrolment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Human and animal studies
The study was conducted in accordance with all institutional and national guidelines for the care and use of laboratory animals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Youssef, A.T. The value of superficial parts and endoanal ultrasonography in evaluating pilonidal disease and exclusion of perianal sepsis. J Ultrasound 18, 237–243 (2015). https://doi.org/10.1007/s40477-015-0156-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-015-0156-3