Abstract
Radiolabelled aerosols provide a versatile means of studying the pathophysiology of lung disease. If aerosols consisting of small particles are used, a qualitative image of the distribution of ventilation is obtained. Larger particles are deposited by inertial impaction, mainly in larger airways. This mechanism is related to changes in the direction and velocity of airflow rather than to ventilation and is therefore very sensitive to airway narrowing. Measurements of aerosol deposition can therefore identify very early changes in the airways in chronic obstructive pulmonary disease (COPD) and asthma. Aerosols of solid particles can, when deposited on the ciliated mucosa, be used for assessment of mucociliary clearance and are useful for evaluation of therapeutic measures in COPD and asthma. Soluble tracers delivered as aerosols may be absorbed from the lungs into the bloodstream and provide a measure of the permeability of the alveolar–capillary barrier. Finally, radioactive aerosols are extensively used in the development of devices and formulations for inhaled pharmaceuticals.
Similar content being viewed by others
The first application of radiolabelled aerosols for functional imaging of the lungs was as a means of ventilation scintigraphy, used as a complement to lung perfusion scintigraphy for the diagnosis of pulmonary embolism [1]. Although this is still their major clinical application, radiolabelled aerosols have also been used for a number of other purposes, e.g. basic studies of airway pathophysiology, assessment of the deposition of pharmaceutical aerosols, measurement of mucociliary clearance, and assessment of the permeability of the alveolar–capillary barrier. This review provides a brief account of the use of radiolabelled aerosols in chronic obstructive pulmonary disease (COPD) and asthma.
Mechanisms of aerosol deposition in the lungs
Solid and liquid particles are inhaled with every breath, and a variable fraction of these particles is deposited in the lungs. There are three main mechanisms of deposition of non-fibrous particles: inertial impaction, gravitational sedimentation and Brownian diffusion. The mechanism of deposition depends largely on particle size. Considering particles with a density of approximately 1 g/mL, few particles with a diameter >10 μm will reach the lungs; such particles will instead be deposited mainly in the upper airways. Particles with a diameter greater than a few micrometres that reach the lungs are deposited mainly by inertial impaction. This is due to the inability of the particle to follow changes in the direction of airflow that occur, e.g. at airway bifurcations. The probability of impaction increases with particle size and with airflow velocity. Impaction, therefore, occurs to a great extent in the larger airways, where airflow velocity is high (Fig. 1). Impaction also occurs to a greater extent in diseased airways, where there may be sudden changes in both the direction and the velocity of airflow owing to variations in airway calibre.
Regional deposition, imaged in the anterior view, of inhaled particles in a normal subject. The image in the left panel was acquired after inhalation of particles with a diameter of 1.7 μm inhaled at a flow rate of approximately 0.5 L/s. The right panel shows an image acquired after inhalation of particles with a diameter of 2.9 μm inhaled at approximately 0.8 L/s in the same subject. Small particle size and low flow result in fairly uniform deposition in the periphery of the lungs. After inhalation of larger particles at higher flow rate, heavy deposition is seen in the trachea and main bronchi. The activity in the ventricle represents particles initially deposited in the mouth and then swallowed. Approximately, 7 MBq of 99mTc-DTPA was deposited on each occasion. Adapted from Bondesson et al. [2] (colour figure online)
Sedimentation is the major mechanism of deposition of particles ranging from approximately one to a few micrometres in diameter. While such particles reside in the lungs, they are affected by gravitation and may settle on the airway wall. The probability of sedimentation increases with particle size and longer residence time in the lungs. As settling velocity is rather low, sedimentation occurs mainly in the periphery of the lung, where distances are short.
Particles smaller than approximately 1 μm in diameter undergo Brownian diffusion as a result of collision with gas molecules. This results in random movements, which may result in deposition of the particle on the airway wall. Diffusion occurs mainly in the most distal air spaces, where flow velocity is low and the distance to the airway wall is short. The probability of deposition by diffusion increases with residence time in the lungs but is inversely related to particle size.
The deposited fraction of inhaled particles varies dramatically according to particle size [3, Fig. 2]. Particles in the range of 5–10 micrometres, which are deposited by impaction in the larger airways, are retained to a great extent. The retention of very small particles, deposited by diffusion in the periphery of the lung, is also very high. The total deposition of inhaled particles in the micrometre range is increased in subjects with asthma as well as in subjects with COPD [4, 5]. One of the more prominent factors explaining this phenomenon is likely to be increased deposition by impaction in narrowed airways.
Deposition of inhaled particles as a function of particle size. Adapted from Heyder et al. [3]
Measurement of deposition of radiolabelled aerosols
A very wide range of aerosol particles, both solid and liquid, has been labelled with gamma-emitting isotopes. Solid particles are preferred if static conditions are required, e.g. if a long imaging time is needed. A disadvantage of labelling solid particles is that the procedure is often laborious and time consuming. If the labelling is sufficiently stable, solid particles can be suspended in a water solution and administered with a conventional nebuliser. If, on the other hand, the labelling is not stable or the particle itself is water soluble, the aerosol has to be administered as a dry powder, which may introduce difficulties. When pharmaceutical preparations are labelled, the label is often associated with, rather than chemically bound to, the particles. As a result, the label may leach from the particles after they have been deposited in the lungs. The label can then be absorbed from the lungs, which will obviously affect the measurement of deposition. Liquid particles can easily be generated by nebulisation of a solution of a suitable tracer molecule. In this case, the rate of absorption of the tracer from the lungs is a very important consideration. 99mTcO4 − is a very commonly used radiolabel. As it is very rapidly absorbed from the lungs, reliable measurements of deposition can be obtained only during the first few minutes after inhalation of the aerosol [6].
Most previous studies of aerosol deposition (both physiological studies and studies assessing inhaled pharmaceuticals) have been carried out using static imaging. In studies restricted to deposition, static images of the chest and often the upper airways and stomach are obtained at least in the anterior and posterior views. If total deposition is measured, attenuation and a number of other factors need to be accounted for [6]. Regional deposition of the aerosol in the lungs is often of interest. As airway disease often results in higher deposition in central airways, deposition is often compared between the central and peripheral lung fields. This is conventionally done by selecting a region of interest covering the hilar region of the lung and a peripheral region and calculating a “penetration index” as the ratio of activity in the peripheral and hilar regions. The outline of the lungs is obtained by separate imaging using a radioactive gas or transmission imaging with a flood source. Imaging procedures as well as image analysis have been standardised for pharmaceutical applications [7]. In addition to particle penetration to peripheral airways, various indices of inhomogeneity have been used to describe aerosol deposition and examine its relation to lung function [8–10].
Single-photon emission tomography (SPECT) is increasingly used for aerosol deposition studies. The technique is particularly useful if combined with X-ray computed tomography (CT), whereby aerosol deposition can be related to morphology. The major advantage of SPECT is the improved separation between the bronchial and alveolar regions of the lungs. The CT scan serves several purposes, providing outlines of the lungs as well as anatomical information and data used for attenuation correction. If high-resolution CT is performed, the lobes of the lungs as well as several generations of bronchi can be identified. This comes, however, at the cost of a substantial radiation burden to the subject. Analysis of regional deposition in SPECT studies is often done by relating the activity in the peripheral parts of the lungs to that in the hilar region. Volumes of interest in the form of concentric shells are delineated starting from the hilum [11] and a ratio between outer and inner shells is calculated. As static imaging, SPECT has been standardised for pharmaceutical applications [12]. Combined with a mathematical model of the airways [13], deposition in the different shells can be partitioned between airway generations [14]. As for planar imaging several other methods for assessment of homogeneity of deposition have been described [15, 16].
Radiolabelled aerosols for ventilation scintigraphy
Radioactive aerosols are commonly used for ventilation scintigraphy in association with lung perfusion scintigraphy for the diagnosis of pulmonary embolism. A prerequisite for using aerosols for ventilation scintigraphy is that the particles are deposited mainly by diffusion or sedimentation. Deposition by impaction is related to local changes in the direction of airflow rather than to regional ventilation and will produce artefacts in the form of hot spots in the ventilation image. The aerosol can be generated by nebulisation of a water solution containing, for example, diethylene-triamine penta-acetate labelled with 99mTc (99mTc-DTPA). Several nebulisers are available that will produce aerosols with a median particle diameter of approximately 2 μm [17]. Technegas is an alternative technique, based on generation of solid particles [18]. A solution of 99mTcO4 − is evaporated in a crucible made of graphite. The crucible is then heated to 2,750 °C for a few seconds. This leads to the formation of an aerosol of 99mTc-labelled carbon particles with a median diameter of approximately 0.2 μm [19]. There are two important differences between the two methods. One is that 99mTc-DTPA is absorbed from the lungs. The half-life of the tracer in the lungs is approximately 60 min in healthy non-smokers, but considerably shorter in smokers and in subjects with interstitial lung diseases [20, 21]. In these categories of subjects, the activity in the lungs will therefore change during image acquisition. Technegas, by contrast, remains in the lung for more than 24 h [22]. The other important difference is the particle size of the aerosols. The Technegas particles are considerably smaller than those resulting from nebulisation of solutes. In subjects with airflow obstruction, there is an increased tendency to impaction of particles in the central airways, resulting in hot spots in the ventilation image and difficulties in interpretation. Since nebulisation produces larger particles than Technegas, greater problems are encountered with 99mTc-DTPA [23]. Even Technegas, however, gives rise to hot spots in the ventilation image in subjects with airflow obstruction [23–25; Fig. 3]. Aerosol scintigrams should therefore always be regarded as qualitative, rather than quantitative, images of the distribution of ventilation. Consequently, parametric images representing ventilation/perfusion ratios are of questionable value if based on aerosol scintigrams.
Aerosol ventilation scintigrams obtained in two patients undergoing ventilation/perfusion scintigraphy because of suspicion of pulmonary embolism. Single-photon emission tomography (SPECT) was performed after inhalation of approximately 20 MBq of Technegas. Upper panels show transverse planes and lower panels frontal planes. Horizontal green and blue lines indicate the position of the tomographic sections with respect to each other. The subject in the left panels has normal lung function, whereas the subject in the right panels suffers from moderate chronic obstructive pulmonary disease (forced expiratory volume in one second: 67 % of predicted value). There is increased deposition in large airways in the patient with airflow obstruction. R right, L left, A anterior, P posterior, H head, F feet (colour figure online)
Aerosol deposition in COPD and asthma
Pathological changes in the lungs in COPD include chronic inflammation and fibrosis of airway walls, mucus gland hyperplasia with mucus hypersecretion and emphysema. There is also a substantial reduction in the number of respiratory bronchioles. These structural changes lead to abnormal distribution of ventilation, characterised by multiple regions with reduced ventilation. These regions are generally widespread and diffuse and do not correspond to lung segments [26]. SPECT provides a better assessment of the distribution of ventilation defects than planar imaging does [27]. Given a particle size of less than about 2 μm, an aerosol scintigram can be used to estimate qualitatively the distribution of ventilation [24, 28–33].
Hot spots, reflecting increased aerosol deposition in central airways, are a common finding in subjects with COPD. Figure 4 shows aerosol scintigrams from a subject with moderate COPD (forced expiratory volume in one second [FEV1] 67 % of predicted). An aerosol with particle size 4.9 μm has been inhaled at a flow rate of 1.8 L/s. The upper panel is a static image in the anterior view showing heavy deposition in the central airways. Below is a SPECT/CT registration in a frontal plane at the level of the hilum. The left panel shows a low-dose CT that allows only the large airways to be identified. The right panel shows the aerosol image in colour fused with the CT. The hot spots can clearly be localised to the larger bronchi. The presence of hot spots is a function of aerosol particle size, the prevalence increasing for larger particles [34, 35]. The increased deposition in large airways is probably partly explained by airway narrowing, leading to higher flow velocity. Increased proximal deposition has thus been shown in normal volunteers in response to methacholine provocation [36, 37]. Furthermore, changes in airflow direction can be expected to occur to a greater extent in the airways of subjects with COPD. High flow velocity and changes in the direction of airflow would tend to increase particle deposition by impaction. Penetration of aerosol to the periphery of the lungs as well as other indices of heterogeneous deposition are well known to correlate with the degree of airflow obstruction in subjects with COPD [15, 29, 30, 38]. Even subjects with normal overall lung function tests may have abnormal aerosol deposition, showing the high sensitivity of the regional imaging technique [31].
Aerosol deposition studied by static imaging (top panel) and single-photon emission tomography and computed tomography (SPECT/CT; lower panels) in a subject with moderate chronic obstructive pulmonary disease. The study was approved by the Ethics Committee of Malmö University (HS60-10/953/11) and written, informed consent was obtained. See text for details
Some subjects, often ones with severe COPD, show a different pattern of aerosol distribution. Figure 5 shows a subject with severe COPD (FEV1 27 % of predicted value) who inhaled aerosol as described above. The left panel is a static image in the anterior view showing very uneven distribution with a large number of hot spots. The right panel is a fused image from a SPECT/CT examination showing that the hot spots, in this case, do not correspond primarily to the proximal airways, but to a large extent also occur in the periphery of the lungs. This pattern is difficult to explain on the basis of airway narrowing alone, as flow velocity in small airways is normally very low. A putative mechanism is that there is severe reduction in the number of patent peripheral airways, resulting in high flow through a limited number of airways. Aerosol scintigraphy in combination with high-resolution CT may provide more information concerning this pattern of deposition.
The pathology of asthma entails mucosal inflammation, bronchial hyperresponsiveness and hypersecretion with mucus plugging. With longstanding disease, there may be permanent remodelling of the airway walls with deposition of collagen and smooth muscle hypertrophy. In mild disease, lung function is often normal between symptomatic episodes, whereas in chronic disease there may be airflow obstruction already in the basal state. During an asthma attack, there is smooth muscle contraction with reduced airway calibre. Bronchoconstriction gives rise to multiple regions with reduced ventilation [39, 40]. These may normalise after bronchodilatation, but ventilation defects can be present even if pulmonary function tests are normal.
Aerosol scintigrams in acute asthma show multiple defects, often corresponding to lung segments, and focal deposition of aerosol in the larger bronchi [25, 41]. Such focal deposition has been shown to represent flow-limiting segments [25], whereas the peripheral defects reflect the reduced ventilation of the corresponding lung regions. In chronic asthma, there may be widespread abnormalities in the aerosol scintigram.
Asthma attacks often result in closure of peripheral airways [42]. King and co-workers [43] have described a technique whereby this phenomenon can be studied using Technegas. The aerosol is inhaled as a small bolus from residual volume, followed by room air. With this procedure the volume distal to the closed airways does not receive any aerosol and appears as a defect. The volume thus measured correlates with closing volume and closing capacity as measured by nitrogen washout. In addition to determining the volume of closed-off lung, the method provides information about the localisation of airway closure [44]. The volume of closed-off lung tends to increase with increasing bronchial hyperresponsiveness in asthmatic subjects [45].
Deposition of pharmaceutical aerosols
Radionuclide imaging is a well-established means of determining the dose of an inhaled pharmaceutical aerosol reaching the lungs as well as its regional deposition within the lungs [46]. A wealth of information about the properties of different inhalers has been obtained with radiolabelled aerosols. A detailed account of this field is beyond the scope of this review. Labelling of pharmaceutical aerosols with radionuclides requires extensive validation of the stability of the formulation and the distribution of the radiolabel and the active compound relative to particle size. Guidelines for this validation, as well as for imaging, have been established [7, 12, 47].
While the effects of device design, particle size and inhalation parameters on total and regional deposition have been extensively studied (Fig. 6), less information is available about the relationship between the site of deposition and the therapeutic effect [48–50]. In studies investigating this aspect, inspiratory flow and particle size are often varied to change the pattern of deposition. It is then important to measure the dose delivered to the lungs as well as indicators of regional distribution, as the particle losses in the device and upper airways may not be the same.
Distribution of a radiolabelled powder aerosol inhaled from a commercial inhaler (Diskhaler). The lactose particles in the ordered mixture of the drug were labelled with 99mTcO4 −. A normal subject inhaled a metered dose of 70 MBq, resulting in a total deposition of approximately 50 MBq. The images were obtained by scanning from the head to the waist with a double-headed gamma camera immediately after the inhalation. Approximately, 26 % of the metered dose is deposited in the lungs. There is heavy deposition in the large bronchi, but also penetration of particles to the periphery of the lungs. A substantial fraction of the inhaled dose is deposited in the mouth and subsequently partly swallowed. There is also considerable deposition in the larynx. Adapted from Bondesson et al. [6] (colour figure online)
The vast majority of studies of radiolabelled pharmaceutical aerosols have been performed with gamma-emitting tracers. However, positron-emitting tracers offer better possibilities for labelling the active compound rather than the preparation [51]. With better standardisation of procedures and increasing use of positron emission tomography, the importance of radionuclide imaging in the development of inhaled pharmaceuticals can be expected to increase.
Mucociliary clearance
Mucociliary clearance is fundamentally important for the removal of secretions and foreign particles that have been deposited in the airways. The overall principle of the system is simple: the ciliated cells in the epithelium transport the mucus with deposited particles in a proximal direction and eventually the mucus is expectorated or swallowed. Mucus may also be eliminated by coughing, a mechanism that is effective only in the proximal airways.
Mucociliary clearance can be measured using insoluble, radiolabelled aerosol particles. The aerosol should be administered so that the particles are deposited preferentially on the ciliated mucosa. A number of different inhalation patterns can be used, some of which entail bolus administration and breath-hold [52]. With this mode of administration, the particles do not penetrate to the periphery of the lungs, and a separate image is needed to define the borders of the lungs. This can be achieved by breathing radioactive gas or using a flood source for a transmission scintigram. Activity is monitored over the lungs for a variable time, usually up to 24 h. Regions of interest are drawn over the lungs and retention curves generated. If clearance is analysed over both peripheral and central regions, correction for transport from the peripheral to the central regions needs to be performed. As the rate of mucociliary clearance is considerably slower in peripheral than in central airways, the pattern of deposition of the inhaled aerosol is very important in determining the result [53]. The initial distribution is therefore characterised by, e.g. determining a penetration index for the aerosol. Agnew and Hasani [54] have described how the initial deposition can be taken into account in the analysis of mucociliary clearance. Coughing can account for a substantial part of mucus clearance in subjects with airway disease and therefore needs to be controlled. If activity is monitored continuously and coughing recorded, the retention curve can be corrected for the effect of coughing [55]. Another approach is to measure cough clearance separately in response to voluntary coughing.
The rate of mucociliary clearance is reduced in subjects with COPD and the fraction of mucus cleared by coughing is increased [56]. Measurements with targeting of peripheral airways, conducted over an extended period of time, suggest that mucociliary clearance may be reduced in small airways in COPD [57]. In asthmatic subjects, mucociliary clearance is severely reduced during acute exacerbations but improves in remission [58].
In addition to basic studies of pathophysiology, measurement of mucociliary clearance has been used extensively for evaluation of pharmacological as well as non-pharmacological approaches to improve mucus clearance in subjects with airway diseases [59, 60]. If the rate of mucociliary clearance can be shown to correlate with clinical endpoints, e.g. rate of lung function decline, exacerbation frequency or survival, the method may also become more clinically useful.
Permeability of the alveolar–capillary barrier
Substances that are deposited in the lungs may be absorbed into the bloodstream. For water-soluble substances, the rate of absorption is inversely related to the size of the molecule [61]. Radioactive aerosols have been applied extensively for studying the absorption of solutes from the lungs. The most frequently used tracer is 99mTc-DTPA. This is very hydrophilic compound with a molecular weight of 490 dalton. Most often, the alveolar epithelium is targeted. An aerosol with small particles is, therefore, inhaled at a low flow rate to promote deposition in the periphery of the lung. Activity is then continuously measured over the chest and a retention curve generated over the lungs. Correction for circulating tracer is performed by i.v. injection of a small amount of tracer at the end of the acquisition. The rate of absorption is expressed as the slope of the retention curve.
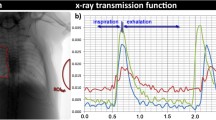
In normal non-smokers, the retention curve follows a mono-exponential course with a half-life of approximately 1 h [20]. The rate of absorption of 99mTc-DTPA is dramatically increased in smokers [20, 62; Fig. 7]. The retention of 99mTc-DTPA in the lungs is extremely sensitive to smoking, thus even symptom-free subjects exposed to passive smoking have an increased rate of absorption [63]. The abnormality is reversible after stopping smoking [64].
Retention curves of 99mTc-DTPA over the lungs from a healthy non-smoker (left panel) and a healthy smoker (right panel). The aerosol (particle diameter 1.7 μm, approximately 10 MBq) was inhaled by tidal breathing from an air jet nebuliser. Interrupted lines are exponential fits. The retention curve of the non-smoker follows a mono-exponential course with a half-life of about 70 min. In the smoker, the curve follows a bi-exponential course with half-lives of the slow and fast components of 80 and 13 min, respectively. Adapted from Wollmer and Evander [20]
The mechanisms underlying increased permeability of the blood–gas barrier are not entirely clear, but the pulmonary surfactant system appears to be an important part of the barrier. In animal models of surfactant dysfunction, absorption of 99mTc-DTPA increases dramatically [65, 66]. Conversely, if the amount of alveolar surfactant is increased experimentally, the rate of absorption is reduced, both in normal animals and in animals with surfactant dysfunction [67, 68]. In smokers, the recovery of phosphatidyl choline, a major component of alveolar surfactant, at lung lavage is correlated with the half-life of 99mTc-DTPA in the lungs [69]. There are, however, also other limiting factors. The rate of absorption depends on ventilation pattern, increasing with lung volume and tidal excursions and thus during exercise [70, 71].
In smokers with COPD, it appears to be the smoke exposure rather than the bronchial disease that causes increased absorption of 99mTc-DTPA [72]. A number of studies of the absorption of 99mTc-DTPA have been performed in asthmatics. In subjects with stable disease, there is no difference in the rate of absorption relative to normal subjects, and the absorption is not related to airway hyperresponsiveness [73–75]. During an acute asthma attack, an increased rate of absorption has, however, been reported [76].
Even though the rapid improvement in pulmonary absorption of 99mTc-DTPA has been suggested as a means of encouraging subjects in smoking-cessation programmes, by providing an indication of improvement in lung function after stopping smoking, the practical utility of this technique is limited in airway diseases. The technique is more useful in interstitial lung diseases, even though the effect of smoking is a confounder [77]. Measurements of the absorption of inhaled 99mTc-DTPA have been very useful in the development of inhaled pharmaceuticals, as the findings predict the kinetics of inhaled, water-soluble drugs [78–81].
Conclusion
Radioactive aerosols provide a versatile means of studying pulmonary pathophysiology and pharmacology. Combinations of aerosol deposition studies and other functional or morphological methods such as high-resolution CT or magnetic resonance imaging will most likely provide new information about the properties of the airways in obstructive lung diseases. Radioactive aerosols have an established role in clinical ventilation–perfusion imaging. Further development of inhaled pharmaceuticals would be virtually impossible without the use of radioactive aerosols.
References
Taplin GV, Poe ND (1965) A dual lung-scanning technic for evaluation of pulmonary function. Radiology 85:365–368
Bondesson E, Bengtsson T, Nilsson LE, Wollmer P (2007) Site of deposition and absorption of an inhaled hydrophilic solute. Br J Clin Pharmacol 63:722–731
Heyder J, Gebhart J, Rudolf G, Schiller CF, Stahlhofen W (1986) Deposition of particles in the human respiratory tract in the size range 0.005–15 μm. J Aerosol Sci 17:811–825
Kim CS, Kang TC (1997) Comparative measurement of lung deposition of inhaled fine particles in normal subjects and patients with obstructive airway disease. Am J Respir Crit Care Med 155:899–905
Brown JS, Zeman KL, Bennett WD (2002) Ultrafine particle deposition and clearance in the healthy and obstructed lung. Am J Respir Crit Care Med 166:1240–1247
Bondesson E, Bengtsson T, Borgström L, Nilsson LE, Norrgren K, Trofast E, Wollmer P (2003) Planar gamma scintigraphy–points to consider when quantifying pulmonary dry powder aerosol deposition. Int J Pharm 258:227–240
Newman S, Bennett WD, Biddiscombe M, Devadason SG, Dolovich MB, Fleming J, Haeussermann S, Kietzig C, Kuehl PJ, Laube BL, Sommerer K, Taylor G, Usmani OS, Zeman KL (2012) Standardization of techniques for using planar (2D) imaging for aerosol deposition assessment of orally inhaled products. J Aerosol Med Pulm Drug Deliv 25(Suppl 1):S10–S28
Olséni L, Palmer J, Wollmer P (1994) Quantitative evaluation of aerosol deposition pattern in the lung in patients with chronic bronchitis. Physiol Meas 15:41–48
Lloyd JJ, Taylor CJ, James JM, Lawson RS, Shields RA, Testa HJ (1995) Texture analysis of technegas lung ventilation images. Med Biol Eng Comput 33:52–57
Xu JH, Moonen M, Johansson A, Bake B (1998) Inhomogeneity in planar ventilation scintigraphy of emphysematous patients. Clin Physiol 18:435–440
Fleming JS, Hashish AH, Conway JH, Nassim MA, Holgate ST, Halson P, Moore E, Bailey AG, Martonen TB (1996) Assessment of deposition of inhaled aerosol in the respiratory tract of man using three-dimensional multimodality imaging and mathematical modeling. J Aerosol Med 9:317–327
Fleming J, Bailey DL, Chan HK, Conway J, Kuehl PJ, Laube BL, Newman S (2012) Standardization of techniques for using single-photon emission computed tomography (SPECT) for aerosol deposition assessment of orally inhaled products. J Aerosol Med Pulm Drug Deliv 25(Suppl 1):S29–S51
Montesantos S, Fleming JS, Tossici-Bolt L (2010) A spatial model of the human airway tree: the hybrid conceptual model. J Aerosol Med Pulm Drug Deliv 23:59–68
Majoral C, Fleming J, Conway J, Katz I, Tossici-Bolt L, Pichelin M, Montesantos S, Caillibotte G (2014) Controlled, parametric, individualized, 2D and 3D imaging measurements of aerosol deposition in the respiratory tract of healthy human volunteers: in vivo data analysis. J Aerosol Med Pulm Drug Deliv Epub ahead of print. PMID: 24400875
Xu J, Moonen M, Johansson A, Gustafsson A, Bake B (2001) Quantitative analysis of inhomogeneity in ventilation SPET. Eur J Nucl Med 28:1795–1800
Chung HW, Huang YH (2000) Fractal analysis of nuclear medicine images for the diagnosis of pulmonary emphysema: interpretations, implications, and limitations. AJR Am J Roentgenol 174:1055–1059
Chinet T, Collignon MA, Dusser D, Barritault L, Huchon GJ (1986) Effectiveness of micronic aerosol generators and their aerosol characteristics. Eur J Respir Dis 69:153–159
Burch WM, Tetley IJ, Gras JL (1984) Technetium-99 m ‘pseudogas’ for diagnostic studies in the lung. Clin Phys Physiol Meas 5:79–85
Lloyd JJ, Shields RA, Taylor CJ, Lawson RS, James JM, Testra HJ (1995) Technegas and Pertechnegas particle size distribution. Eur J Nucl Med 22:473–476
Wollmer P, Evander E (1994) Biphasic pulmonary clearance of 99mTc-DTPA in smokers. Clin Physiol 14:547–559
Brådvik I, Wollmer P, Evander E, Lárusdóttir H, Blom-Bülow B, Jonson B (1994) Different kinetics of lung clearance of technetium-99m labelled diethylene triamine penta-acetic acid in patients with sarcoidosis and smokers. Eur J Nucl Med 21:1218–1222
Wiebert P, Sanchez-Crespo A, Falk R, Philipson K, Lundin A, Larsson S, Möller W, Kreyling WG, Svartengren M (2006) No significant translocation of inhaled 35-nm carbon particles to the circulation in humans. Inhal Toxicol 18:741–747
Jögi J, Jonson B, Ekberg M, Bajc M (2010) Ventilation-perfusion SPECT with 99mTc-DTPA versus Technegas: a head-to-head study in obstructive and nonobstructive disease. J Nucl Med 51:735–741
James JM, Lloyd JJ, Leahy BC, Church S, Hardy CC, Shields RA, Prescott MC, Testa HJ (1992) 99Tcm-Technegas and krypton-81 m ventilation scintigraphy: a comparison in known respiratory disease. Br J Radiol 65:1075–1082
Pellegrino R, Biggi A, Papaleo A, Camuzzini G, Rodarte JR, Brusasco V (2001) Regional expiratory flow limitation studied with Technegas in asthma. J Appl Physiol 91:2190–2198
Cunningham DA, Lavender JP (1981) Krypton 81 m ventilation scanning in chronic obstructive airways disease. Br J Radiol 54:110–116
Stavngaard T, Mortensen J (2005) Assessment of ventilation inhomogenity with Krypton SPECT and planar imaging. Clin Physiol Funct Imaging 25:106–112
Short MD, Dowsett DJ, Heaf PJ, Pavia D, Thomson ML (1979) A comparison between monodisperse Tc-99 m-labeled aerosol particles and Kr-81 m for the assessment of lung function. J Nucl Med 20:194–200
Fazio F, Wollmer P, Lavender JP, Barr MM (1982) Clinical ventilation imaging with 113mIn aerosol: a comparison with 81mKr. J Nucl Med 23:306–314
Wollmer P, Eriksson L, Andersson AC (1985) Clinical assessment of a commercial delivery system for aerosol ventilation scanning by comparison with Krypton-81 m. J Nucl Med Technol 13:63–67
Agnew JE, Francis RA, Pavia D, Clarke SW (1982) Quantitative comparison of 99Tcm-aerosol and 81Krm ventilation images. Clin Phys Physiol Meas 3:21–30
Cook G, Clarke SE (1992) An evaluation of Technegas as a ventilation agent compared with krypton-81 m in the scintigraphic diagnosis of pulmonary embolism. Eur J Nucl Med 19:770–774
Hartmann IJ, Hagen PJ, Stokkel MP, Hoekstra OS, Prins MH (2001) Technegas versus (81m)Kr ventilation-perfusion scintigraphy: a comparative study in patients with suspected acute pulmonary embolism. J Nucl Med 42:393–400
Glover W, Chan HK, Eberl S, Daviskas E, Verschuer J (2008) Effect of particle size of dry powder mannitol on the lung deposition in healthy volunteers. Int J Pharm 349:314–322
Fazzi P, Borsò E, Albertelli R, Mariani G, Giuntini C (2009) Comparative performance of two inhaler systems to assess distribution of convective ventilation by 99mTc-labeled aerosol scintigraphy in patients with airway obstruction. Q J Nucl Med Mol Imaging 53:428–436
Richards R, Haas A, Simpson S, Britten A, Renwick A, Holgate S (1988) Effect of methacholine induced bronchoconstriction on the pulmonary distribution and plasma pharmacokinetics of inhaled sodium cromoglycate in subjects with normal and hyperreactive airways. Thorax 43:611–616
O’Riordan TG, Walser L, Smaldone GC (1993) Changing patterns of aerosol deposition during methacholine bronchoprovocation. Chest 103:1385–1389
Jögi J, Ekberg M, Jonson B, Bozovic G, Bajc M (2011) Ventilation/perfusion SPECT in chronic obstructive pulmonary disease: an evaluation by reference to symptoms, spirometric lung function and emphysema, as assessed with HRCT. Eur J Nucl Med Mol Imaging 38:1344–1352
Agnew JE, Bateman JR, Pavia D, Clarke SW (1984) Radionuclide demonstration of ventilatory abnormalities in mild asthma. Clin Sci (Lond) 66:525–531
Altes TA, Powers PL, Knight-Scott J, Rakes G, Platts-Mills TA, de Lange EE, Alford BA, Mugler JP 3rd, Brookeman JR (2001) Hyperpolarized 3He MR lung ventilation imaging in asthmatics: preliminary findings. J Magn Reson Imaging 13:378–384
Chung KF, Jeyasingh K, Snashall PD (1988) Influence of airway calibre on the intrapulmonary dose and distribution of inhaled aerosol in normal and asthmatic subjects. Eur Respir J 1:890–895
Kaminsky DA (2011) Peripheral lung mechanics in asthma: exploring the outer limits. Pulm Pharmacol Ther 24:199–202
King GG, Eberl S, Salome CM, Meikle SR, Woolcock AJ (1997) Airway closure measured by a technegas bolus and SPECT. Am J Respir Crit Care Med 155:682–688
King GG, Eberl S, Salome CM, Young IH, Woolcock AJ (1998) Differences in airway closure between normal and asthmatic subjects measured with single-photon emission computed tomography and technegas. Am J Respir Crit Care Med 158:1900–1906
Farrow CE, Salome CM, Harris BE, Bailey DL, Bailey E, Berend N, Young IH, King GG (1985) Airway closure on imaging relates to airway hyperresponsiveness and peripheral airway disease in asthma. J Appl Physiol 113:958–966
Corcoran TE, Devadason SG, Kuehl PJ (2012) Introduction: aerosol delivery of orally inhaled agents. J Aerosol Med Pulm Drug Deliv 25(Suppl 1):S3–S5
Devadason SG, Chan HK, Haeussermann S, Kietzig C, Kuehl PJ, Newman S, Sommerer K, Taylor G (2012) Validation of radiolabeling of drug formulations for aerosol deposition assessment of orally inhaled products. J Aerosol Med Pulm Drug Deliv 25(Suppl 1):S6–S9
Hultquist C, Wollmer P, Eklundh G, Jonson B (1992) Effect of inhaled terbutaline sulphate in relation to its deposition in the lungs. Pulmon Pharmacol 5:127–132
Laube BL, Edwards AM, Dalby RN, Creticos PS, Norman PS (1998) The efficacy of slow versus faster inhalation of cromolyn sodium in protecting against allergen challenge in patients with asthma. J Allergy Clin Immunol 101:475–783
Usmani OS, Biddiscombe MF, Barnes PJ (2005) Regional lung deposition and bronchodilator response as a function of beta2-agonist particle size. Am J Respir Crit Care Med 172:1497–1504
Venegas J, Winkler T, Harris RS (2013) Lung physiology and aerosol deposition imaged with positron emission tomography. J Aerosol Med Pulm Drug Deliv 26:1–8
Bennett WD, Daviskas E, Hasani A, Mortensen J, Fleming J, Scheuch G (2010) Mucociliary and cough clearance as a biomarker for therapeutic development. J Aerosol Med Pulm Drug Deliv 23:261–272
Ilowite JS, Smaldone GC, Perry RJ, Bennett WD, Foster WM (1989) Relationship between tracheobronchial particle clearance rates and sites of initial deposition in man. Arch Environ Health 44:267–273
Agnew JE, Hasani A (2008) Deposition-dependent normal ranges for radioaerosol assessment of lung mucus clearance. J Aerosol Med Pulm Drug Deliv 21:371–380
Lafortuna CL, Fazio F (1984) Acute effect of inhaled salbutamol on mucociliary clearance in health and chronic bronchitis. Respiration 45:111–123
Puchelle E, Zahm JM, Girard F, Bertrand A, Polu JM, Aug F, Sadoul P (1980) Mucociliary transport in vivo and in vitro. Relations to sputum properties in chronic bronchitis. Eur J Respir Dis 61:254–264
Svartengren M, Svartengren K, Europe E, Falk R, Hofmann W, Sturm R, Philipson K, Camner P (2004) Long-term clearance from small airways in patients with chronic bronchitis: experimental and theoretical data. Exp Lung Res 30:333–353
Messina MS, O’Riordan TG, Smaldone GC (1991) Changes in mucociliary clearance during acute exacerbations of asthma. Am Rev Respir Dis 143:993–997
Rogers DF (2005) Mucociliary dysfunction in COPD: effect of current pharmacotherapeutic options. Pulm Pharmacol Ther 18:1–8
Bhowmik A, Chahal K, Austin G, Chakravorty I (2009) Improving mucociliary clearance in chronic obstructive pulmonary disease. Respir Med 103:496–502
Folkesson HG, Matthay MA, Weström BR, Kim KJ, Karlsson BW, Hastings RH (1995) Alveolar epithelial clearance of protein. J Appl Physiol 80:1431–1445
Jones JG, Minty BD, Lawler P, Hulands G, Crawley JC, Veall N (1980) Increased alveolar epithelial permeability in cigarette smokers. Lancet 1:66–68
Beadsmoore C, Cheow HK, Szczepura K, Ruparelia P, Peters AM (2007) Healthy passive cigarette smokers have increased pulmonary alveolar permeability. Nucl Med Commun 28:75–77
Minty BD, Jordan C, Jones JG (1981) Rapid improvement in abnormal pulmonary epithelial permeability after stopping cigarettes. Br Med J (Clin Res Ed) 282:1183–1186
Evander E, Wollmer P, Jonson B, Lachmann B (1987) Pulmonary clearance of inhaled 99mTc-DTPA: effects of surfactant depletion by lung lavage. J Appl Physiol 62:1611–1614
Evander E, Wollmer P, Valind S, Sörnmo L, John J, Jonson B (1994) Biexponential pulmonary clearance of 99mTc-DTPA induced by detergent aerosol. J Appl Physiol 77:190–196
Bos JA, Wollmer P, Bakker W, Hannappel E, Lachmann B (1992) Clearance of 99mTc-DTPA and experimentally increased alveolar surfactant content. J Appl Physiol 72:1413–1417
Nilsson K, John J, Lachmann B, Robertson B, Wollmer P (1997) Pulmonary clearance of 99mTc-DTPA in experimental surfactant dysfunction treated with surfactant instillation. Acta Anaesthesiol Scand 41:297–303
Schmekel B, Bos JA, Khan AR, Wohlfart B, Lachmann B, Wollmer P (1992) Integrity of the alveolar-capillary barrier and alveolar surfactant system in smokers. Thorax 47:603–608
Evander E, Wollmer P, Jonson B (1990) Pulmonary clearance of inhaled [99Tcm]DTPA: effects of ventilation pattern. Clin Physiol 10:189–199
Meignan M, Rosso J, Leveau J, Katz A, Cinotti L, Madelaine G, Galle P (1986) Exercise increases the lung clearance of inhaled technetium-99m DTPA. J Nucl Med 27:274–280
Huchon GJ, Russell JA, Barritault LG, Lipavsky A, Murray JF (1984) Chronic air-flow limitation does not increase respiratory epithelial permeability assessed by aerosolized solute, but smoking does. Am Rev Respir Dis 130:457–460
O’Byrne PM, Dolovich M, Dirks R, Roberts RS, Newhouse MT (1984) Lung epithelial permeability: relation to nonspecific airway responsiveness. J Appl Physiol Respir Environ Exerc Physiol 57:77–84
Elwood RK, Kennedy S, Belzberg A, Hogg JC, Paré PD (1983) Respiratory mucosal permeability in asthma. Am Rev Respir Dis 128:523–527
Del Donno M, Chetta A, Foresi A, Gavaruzzi G, Ugolotti G, Olivieri D (1997) Lung epithelial permeability and bronchial responsiveness in subjects with stable asthma. Chest 111:1160–1255
Lemarchand P, Chinet T, Collignon MA, Urzua G, Barritault L, Huchon GJ (1992) Bronchial clearance of DTPA is increased in acute asthma but not in chronic asthma. Am Rev Respir Dis 145:147–152
O’Doherty MJ, Peters AM (1997) Pulmonary technetium-99m diethylene triamine penta-acetic acid aerosol clearance as an index of lung injury. Eur J Nucl Med 24:81–87
Schmekel B, Borgström L, Wollmer P (1991) Difference in pulmonary absorption of inhaled terbutaline in healthy smokers and non-smokers. Thorax 46:225–228
Schmekel B, Borgström L, Wollmer P (1992) Exercise increases the rate of pulmonary absorption of inhaled terbutaline. Chest 101:742–745
Himmelmann A, Jendle J, Mellén A, Petersen AH, Dahl UL, Wollmer P (2003) The impact of smoking on inhaled insulin. Diabetes Care 26:677–682
Petersen AH, Köhler G, Korsatko S, Wutte A, Wonisch M, Mautner A, Rønn BB, Clauson P, Laursen T, Wollmer P, Pieber TR (2008) The effect of exercise on the absorption of inhaled human insulin in healthy volunteers. Br J Clin Pharmacol 65:165–171
Acknowledgments
This work was supported by the Swedish Heart and Lung Foundation.
Conflict of interest
The author has no conflict of interest.
Human and Animal Studies
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Author information
Authors and Affiliations
Corresponding author
Additional information
Color figures online at http://link.springer.com/article/10.1007/s40336-014-0080-0
Rights and permissions
About this article
Cite this article
Wollmer, P. Aerosolised radionuclides for functional imaging in COPD/asthma. Clin Transl Imaging 2, 403–413 (2014). https://doi.org/10.1007/s40336-014-0080-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-014-0080-0