Abstract
Introduction
The etiology of the end-stage renal disease (ESRD) and the hydration status may be involved in the arterial stiffening process observed in hemodialyzed patients. The ratio between carotid-femoral and carotid-radial pulse wave velocity (PWV ratio) was recently proposed to characterize the patient-specific stiffening process. Aims: to analyze: (1) the PWV-ratio in healthy and hemodialyzed subjects, analyzing potential changes associated to etiologies of the ESRD, (2) the PWV-ratio and hydration status using multiple-frequency bioimpedance and, (3) the effects of hemodialysis on PWV-ratio in a 5-year follow-up.
Methods
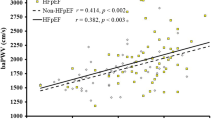
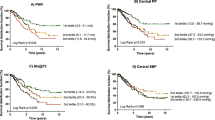
PWV-ratio was evaluated in 151 patients differentiated by the pathology determining their ESRD. Total body fluid (TBF), intra and extra cellular fluid (ICF, ECF) were measured in 65 of these patients using bioelectrical-impedance. The association between arterial, hemodynamic or fluid parameters was analyzed. PWV-ratio was evaluated in a group of patients (n = 25) 5 years later (follow-up study).
Results
PWV-ratio increased in the ESRD cohort with respect to the control group (1.03 ± 0.23 vs. 1.31 ± 0.37; p < 0.001). PWV-ratio in the diabetic nephropathy group was higher than in all other etiological groups (1.61 ± 0.33; p < 0.05). PWV-ratio was associated with TBF (r = −0.238; p < 0.05), ICF (r = −0.323; p < 0.01), ECF/ICF (r = 0.400; p < 0.001) and ECF/TBF (r = 0.403; p < 0.001). PWV-ratio calculated in ESRD patients in 2007 increased 5 years later (1.14 ± 0.32 vs. 1.43 ± 0.44; p < 0.005).
Conclusions
PWV-ratio increased the most in patients with diabetic nephropathy. PWV ratio was significantly associated with age and body hydration status, but not with the blood pressure. PWV-ratio could be considered a blood pressure-independent parameter, associated with the age and hydration status of the patient.



Similar content being viewed by others
References
Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999;99(18):2434–9.
Fortier C, Mac-Way F, Desmeules S, Marquis K, De Serres SA, Lebel M, Boutouyrie P, Agharazii M. Aortic–brachial stiffness mismatch and mortality in dialysis population. Hypertension. 2015;65(2):378–84.
Fortier C, Sidibé A, Desjardins MP, Marquis K, De Serres SA, Mac-Way F, Agharazii M. Aortic–brachial pulse wave velocity ratio: a blood pressure-independent index of vascular aging. Hypertension. 2017;69(1):96–101.
Covic A, Siriopol D. Pulse wave velocity ratio. The new “gold standard” for measuring arterial stiffness. Hypertension. 2015;65(2):289–90.
Bia D, Valtuille R, Galli C, Wray S, Armentano R, Zócalo Y, Cabrera-Fiscer E. Hemodialysis decreases the etiologically-related early vascular aging observed in end-stage renal disease: a 5-year follow-up study. Blood Purif. 2016;43(1–3):18–30.
Wizemann V, Wabel P, Chamney P, Zaluska W, Moissl U, Rode C, Malecka-Masalska T, Marcelli D. The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant. 2009;24(5):1574–9.
Lin Y, Yu W, Hsu T, Ding P, Yang W, Chen C. The extracellular fluid-to-intracellular fluid volume ratio is associated with large-artery structure and function in hemodialysis patients. Am J Kidney Dis. 2003;42:990–9.
Zheng D, Cheng L, Zhuang Z, Gu Y, Tang L, Wang T. Correlation between pulse wave velocity and fluid distribution in hemodialysis patients. Blood Purif. 2009;27:248–52.
Di Iorio B, Nazzaro P, Cucciniello E, Bellizzi V. Influence of haemodialysis on variability of pulse wave velocity in chronic haemodialysis patients. Nephrol Dial Transplant. 2010;25(5):1579–83.
Keith DS, Nichols GA, Gullion CM, Brown JB, Smith DH. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med. 2004;164:659–63.
Fischer E, Zócalo Y, Galli C, Wray S, Bia D: Arterial stiffness and renal replacement therapy: a controversial topic. Int J Nephrol. 2015;2015:7. doi:10.1155/2015/729609.
Santana DB, Zócalo YA, Armentano RL. Integrated e-Health approach based on vascular ultrasound and pulse wave analysis for asymptomatic atherosclerosis detection and cardiovascular risk stratification in the community. IEEE Trans Inf Technol Biomed. 2012;16(2):287–94.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Thoemmes F, Kim ES. A systematic review of propensity score methods in the social sciences. Multivar Behav Res. 2011;46:90–118.
Payne R. Risk calculator based on Joint British Societies risk prediction charts, 2010. http://cvrisk.mvm.ed.ac.uk/calculator/excelcalc.htm; Cardiovascular Risk Calculator. The University of Edinburgh.
Chamney PW, Wabel P, Moissl UM, Müller MJ, Bosy-Westphal A, Korth O, Fuller NJ. A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr. 2007;85(1):80–9.
Bia D, Galli C, Valtuille R, Zócalo Y, Wray S, Armentano RL. Hydration status Is associated with aortic stiffness, but not with peripheral arterial stiffness, in chronically hemodialysed patients. Int J Nephrol. 2015;2015:11. doi:10.1155/2015/628654.
Imai E, Matsuo S, Makino H, Watanabe T, Akizawa T, Nitta K, Iimuro S, Ohashi Y, Hishida A. Chronic kidney disease Japan cohort study: baseline characteristics and factors associated with causative diseases and renal function. Clin Exp Nephrol. 2010;14(6):558–70.
Késoi I, Sági B, Tóth OI, Vas T, Fasekas A, Kovács T, Pintér T, Wittmann I, Nagy J. Different effect of IgA nephropathy and polycystic kidney disease on arterial stiffness. Kidney Blood Press Res. 2011;34(3):158–66.
Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol. 2005;25(5):932–43.
Wabel P, Moissl U, Chamney P, Jirka T, Machek P, Ponce P, Taborsky P, Tetta C, Velasco N, Vlasak J, Zaluska W, Wizemann V. Towards improved cardiovascular management: the necessity of combining blood pressure and fluid overload. Nephrol Dial Transplant. 2008;23(9):2965–71.
Viazzi F, Leoncini G, Ratto E, Storace G, Gonnella A, Garneri D, Bonino B, Cappadona F, Parodi EL, Verzola D, Garibotto G, Pontremoli R. Peripheral artery disease and blood pressure profile abnormalities in hemodialysis patients. J Nephrol. 2016 [Epub ahead of print] (PubMed PMID 27250350).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the René Favaloro University Foundation and funds of “PICT 2008 OC AR 0340” (Argentina) and Agencia Nacional de Investigación e Innovación (ANII; PRSCT-008-020).
Conflict of Interest
Author Dr. Daniel Bia declares that he has no conflict of interest. Dr. Rodolfo Valtuille declares that he has no conflict of interest. Dr. Cintia Galli declares that she has no conflict of interest. M.Sc. Sandra Wray declares that she has no conflict of interest. Dr. Ricardo Armentano declares that he has no conflict of interest. Dr. Yanina Zócalo declares that she has no conflict of interest. Dr. Edmundo Cabrera-Fischer declares that he has no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Bia, D., Valtuille, R., Galli, C. et al. Aortic–Radial Pulse Wave Velocity Ratio in End-stage Renal Disease Patients: Association with Age, Body Tissue Hydration Status, Renal Failure Etiology and Five Years of Hemodialysis. High Blood Press Cardiovasc Prev 24, 37–48 (2017). https://doi.org/10.1007/s40292-017-0178-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-017-0178-3