Abstract
Background
Cardiorespiratory fitness (CRF) among people with severe mental illness (SMI) (i.e., schizophrenia, bipolar disorder, and major depressive disorder) is a critical clinical risk factor given its relationship to cardiovascular disease and premature mortality.
Objectives
This study aimed to: (1) investigate the mean CRF in people with SMI versus healthy controls; (2) explore moderators of CRF; and (3) investigate whether CRF improved with exercise interventions and establish if fitness improves more than body mass index following exercise interventions.
Methods
Major electronic databases were searched systematically. A meta-analysis calculating Hedges’ g statistic was undertaken.
Results
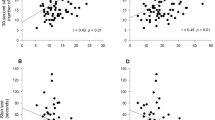
Across 23 eligible studies, pooled mean CRF was 28.7 mL/kg/min [95 % confidence interval (CI) 27.3 to 30.0 mL/kg/min, p < 0.001, n = 980]. People with SMI had significantly lower CRF compared with controls (n = 310) (Hedges’ g = −1.01, 95 % CI −1.18 to −0.85, p < 0.001). There were no differences between diagnostic subgroups. In a multivariate regression, first-episode (β = 6.6, 95 % CI 0.6–12.6) and inpatient (β = 5.3, 95 % CI 1.6–9.0) status were significant predictors of higher CRF. Exercise improved CRF (Hedges’ g = 0.33, 95 % CI = 0.21–0.45, p = 0.001), but did not reduce body mass index. Higher CRF improvements were observed following interventions at high intensity, with higher frequency (at least three times per week) and supervised by qualified personnel (i.e., physiotherapists and exercise physiologists).
Conclusion
The multidisciplinary treatment of people with SMI should include a focus on improving fitness to reduce all-cause mortality. Qualified healthcare professionals supporting people with SMI in maintaining an active lifestyle should be included as part of multidisciplinary teams in mental health treatment.



Similar content being viewed by others
References
Reininghaus U, Dutta R, Dazzan P, et al. Mortality in schizophrenia and other psychoses: a 10-year follow-up of the ÆSOP first-episode cohort. Schizophr Bull. 2015;41(3):664–73.
Osborn DP, Levy G, Nazareth I, et al. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s General Practice Research Database. Arch Gen Psychiatry. 2007;64(2):242–9.
Lawrence D. Excess mortality, mental illness and global burden of disease. Epidemiol Psychiatr Sci. 2015;24(2):141–3.
Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–31.
Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–41.
Ellingrod VL, Taylor SF, Dalack G, et al. Risk factors associated with metabolic syndrome in bipolar and schizophrenia subjects treated with antipsychotics: the role of folate pharmacogenetics. J Clin Psychopharmacol. 2012;32(2):261.
Manu P, Correll CU, Wampers M, et al. Markers of inflammation in schizophrenia: association vs. causation. World Psychiatry. 2014;13(2):189–92.
Vancampfort D, Stubbs B, Mitchell AJ, et al. Risk of metabolic syndrome and its components in people with schizophrenia, bipolar and major depressive disorders: a large scale meta-analysis of 198 studies. World Psychiatry. 2015;14(3):339–47.
Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301(19):2024–35.
Barry VW, Baruth M, Beets MW, et al. Fitness vs. fatness on all-cause mortality: a meta-analysis. Progr Cardiovasc Dis. 2014;56(4):382–90.
Lee DC, Artero EG, Sui X, et al. Review: mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol. 2010;24(4 Suppl):27–35.
Kimhy D, Vakhrusheva J, Bartels MN, et al. Aerobic fitness and body mass index in individuals with schizophrenia: implications for neurocognition and daily functioning. Psychiatry Res. 2014;220(3):784–91.
Rosenbaum S, Tiedemann A, Sherrington C, et al. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry. 2014;75(9):964–74.
Bartels SJ, Pratt SI, Aschbrenner KA, et al. Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. Am J Psychiatry. 2014;172(4):344–52.
Chwastiak L. Making evidence-based lifestyle modification programs available in community mental health centers: why so slow? J Clin Psychiatry. 2015;76(4):519–20.
Vancampfort D, Rosenbaum S, Probst M, et al. Promotion of cardiorespiratory fitness in schizophrenia: a clinical overview and meta-analysis. Acta Psychiatr Scand. 2015;132(2):131–43.
Ward MC, White DT, Druss BG. A meta-review of lifestyle interventions for cardiovascular risk factors in the general medical population: lessons for individuals with serious mental illness. J Clin Psychiatry. 2015;76(4):477–86.
Firth J, Cotter J, Elliott R, et al. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med. 2015;45(7):1343–61.
Vancampfort D, Rosenbaum S, Ward PB, et al. Exercise improves cardiorespiratory fitness in people with schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2015;169(1–3):453–7.
Stubbs B, Rosenbaum S, Vancampfort D, et al. Exercise improves cardiorespiratory fitness in people with depression: a meta-analysis of randomized control trials. J Affect Disord. 2016;190:249–53.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–12.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 2009;6(7):e1000097.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM 5). Washington, DC: American Psychiatric Association; 2013.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV). Washington, DC: American Psychiatric Association; 1994.
World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993.
Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Publ Health Rep. 1985;100(2):126.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Knubben K, Reischies FM, Adli M, et al. A randomised, controlled study on the effects of a short-term endurance training programme in patients with major depression. Br J Sports Med. 2007;41(1):29–33.
Krogh J, Saltin B, Gluud C, et al. The DEMO trial: a randomized, parallel-group, observer-blinded clinical trial of strength versus aerobic versus relaxation training for patients with mild to moderate depression. J Clin Psychiatry. 2009;70(6):790–800.
Pajonk FG, Wobrock T, Gruber O, et al. Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry. 2010;67(2):133–43.
Heggelund J, Nilsberg GE, Hoff J, et al. Effects of high aerobic intensity training in patients with schizophrenia: a controlled trial. Nord J Psychiatry. 2011;65(4):269–75.
Strassnig M, Brar JS, Ganguli R. Low cardiorespiratory fitness and physical functional capacity in obese patients with schizophrenia. Schizophr Res. 2011;126(1):103–9.
Krogh J, Videbech P, Thomsen C, et al. DEMO-II trial. Aerobic exercise versus stretching exercise in patients with major depression: a randomised clinical trial. PLoS One. 2012;7(10):e48316.
Nilsson BM, Olsson RM, Öman A, et al. Physical capacity, respiratory quotient and energy expenditure during exercise in male patients with schizophrenia compared with healthy controls. Eur Psychiatry. 2012;27(3):206–12.
Scheewe TW, Takken T, Kahn RS, et al. Effects of exercise therapy on cardiorespiratory fitness in patients with schizophrenia. Med Sci Sports Exerc. 2012;44(10):1834–42.
Strassnig MT, Newcomer JW, Harvey PD. Exercise improves physical capacity in obese patients with schizophrenia: pilot study. Schizophr Res. 2012;141(2):284–5.
Ostermann S, Herbsleb M, Schulz S, et al. Exercise reveals the interrelation of physical fitness, inflammatory response, psychopathology, and autonomic function in patients with schizophrenia. Schizophr Bull. 2012;39(5):1139.
Abdel-Baki A, Brazzini-Poisson V, Marois F, et al. Effects of aerobic interval training on metabolic complications and cardiorespiratory fitness in young adults with psychotic disorders: a pilot study. Schizophr Res. 2013;149(1–3):112–5.
Bredin SS, Warburton DE, Lang DJ. The health benefits and challenges of exercise training in persons living with schizophrenia: a pilot study. Brain Sci. 2013;3(2):821–48.
Ozbulut O, Genc A, Bagcioglu E, et al. Evaluation of physical fitness parameters in patients with schizophrenia. Psychiatry Res. 2013;210(3):806–11.
Kimhy D, Vakhrusheva J, Bartels MN, et al. Aerobic fitness and body mass index in individuals with schizophrenia: implications for neurocognition and daily functioning. Psychiatry Res. 2014;220(3):784–91.
Kimhy D, Vakhrusheva J, Bartels MN, et al. The impact of aerobic exercise on brain-derived neurotrophic factor and neurocognition in individuals with schizophrenia: a single-blind, randomized clinical trial. Schizophr Bull. 2015;41(4):859–68.
Leone M, Lalande D, Thériault L, et al. Impact of an exercise program on the physiologic, biologic and psychologic profiles in patients with schizophrenia. Schizophr Res. 2015;164(1–3):270.
Nyboe L, Vestergaard CH, Lund H, et al. Metabolic syndrome in first-time hospitalized patients with depression: a 1-year follow-up study. Acta Psychiatr Scand. 2016;133(3):241–8.
Rosenbaum S, Lagopoulos J, Curtis J, et al. Aerobic exercise intervention in young people with schizophrenia spectrum disorders; improved fitness with no change in hippocampal volume. Psychiatry Res Neuroimaging. 2015;232(2):200–1.
Schuch FB, Vasconcelos-Moreno MP, Borowsky C, et al. Exercise and severe major depression: effect on symptom severity and quality of life at discharge in an inpatient cohort. J Psychiatr Res. 2015;61:25–32.
Schuch FB, da Silveira LE, de Zeni TC, et al. Effects of a single bout of maximal aerobic exercise on BDNF in bipolar disorder: a gender-based response. Psychiatry Res. 2015;229(1):57–62.
Vancampfort D, Guelinkcx H, Probst M, et al. Associations between metabolic and aerobic fitness parameters in patients with schizophrenia. J Nerv Ment Dis. 2015;203(1):23–7.
Vancampfort D, Buys R, Sienaert P, et al. Validity of the 6 min walk test in outpatients with bipolar disorder. Psychiatry Res. 2015;230(2):664–7.
Kerling A, Tegtbur U, Gützlaff E, et al. Effects of adjunctive exercise on physiological and psychological parameters in depression: a randomized pilot trial. J Affect Disord. 2015;177:1–6.
Daumit GL, Dickerson FB, Wang NY, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med. 2013;368(17):1594–602.
Green CA, Yarborough BJH, Leo MC, et al. Weight maintenance following the STRIDE lifestyle intervention for individuals taking antipsychotic medications. Obesity. 2015;23(10):1995–2001.
Church TS, LaMonte MJ, Barlow CE, et al. Cardiorespiratory fitness and body mass index as predictors of cardiovascular disease mortality among men with diabetes. Arch Intern Med. 2005;165(18):2114–20.
Hainer V, Toplak H, Stich V. Fat or fit: what is more important? Diabetes Care. 2009;32(Suppl 2):S392–7.
Parker BA, Kalasky MJ, Proctor DN. Evidence for sex differences in cardiovascular aging and adaptive responses to physical activity. Eur J Appl Physiol. 2010;110(2):235–46.
Swift DL, Staiano AE, Johannsen NM, et al. Low cardiorespiratory fitness in African Americans: a health disparity risk factor? Sports Med. 2013;43(12):1301–13.
Richardson LD, Norris M. Access to health and health care: how race and ethnicity matter. Mt Sinai J Med. 2010;77(2):166–77.
Curtis J, Watkins A, Rosenbaum S, et al. Evaluating an individualized lifestyle and life skills intervention to prevent antipsychotic-induced weight gain in first-episode psychosis. Early Interv Psychiatry. 2016;10(3):267–76.
Soundy A, Freeman P, Stubbs B, et al. The transcending benefits of physical activity for individuals with schizophrenia: a systematic review and meta-ethnography. Psychiatry Res. 2014;220(1):11–9.
Gross J, Vancampfort D, Stubbs B, et al. A narrative synthesis investigating the use and value of social support to promote physical activity among individuals with schizophrenia. Disabil Rehabil. 2016;38(2):123–50.
Vancampfort D, Rosenbaum S, Probst M, et al. What are the top 10 physical activity research questions in schizophrenia? Disabil Rehabil. 2016;1–9.
Vancampfort D, Stubbs B, Ward P, et al. Integrating physical activity as medicine in the care of people with severe mental illness. Aust N Z J Psychiatry. 2015;49(8):681–2.
Vancampfort D, Stubbs B, Ward PB, et al. Why moving more should be promoted for severe mental illness. Lancet Psychiatry. 2015;2(4):295.
Weston KS, Wisløff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med. 2014;48(16):1227–34.
Vancampfort D, Stubbs B, Venigalla SK, et al. Adopting and maintaining physical activity behaviours in people with severe mental illness: the importance of autonomous motivation. Prev Med. 2015;81:216–20.
Beauchamp MK, Nonoyama M, Goldstein RS, et al. Interval versus continuous training in individuals with chronic obstructive pulmonary disease—a systematic review. Thorax. 2010;65(2):157–64.
Vancampfort D, Probst M, Sweers K, et al. Relationships between obesity, functional exercise capacity, physical activity participation and physical self-perception in people with schizophrenia. Acta Psychiatr Scand. 2011;123(6):423–30.
Biddle SJ, Batterham AM. High-intensity interval exercise training for public health: a big HIT or shall we HIT it on the head? Int J Behav Nutr Phys Act. 2015;12(1):95.
Mitchell A, De Hert M. Promotion of physical health in persons with schizophrenia: can we prevent cardiometabolic problems before they begin? Acta Psychiatr Scand. 2015;132(2):83–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Davy Vancampfort has support from the Research Foundation-Flanders (FWOVlaanderen). Brendon Stubbs was supported by the Collaboration for Leadership in Applied Health Research and Care South London for this article. No other sources of funding were used to assist in the preparation of this article.
Conflict of interest
Davy Vancampfort, Simon Rosenbaum, Felipe Schuch, Philip Ward, Justin Richards, James Mugisha, Michel Probst, and Brendon Stubbs declare that they have no conflicts of interest relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vancampfort, D., Rosenbaum, S., Schuch, F. et al. Cardiorespiratory Fitness in Severe Mental Illness: A Systematic Review and Meta-analysis. Sports Med 47, 343–352 (2017). https://doi.org/10.1007/s40279-016-0574-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-016-0574-1