Abstract
Objective
To provide a framework for addressing payers’ criteria during the development of pharmaceuticals.
Methods
A conceptual framework was presented to an international health economic expert panel for discussion. A structured literature search (from 2010 to May 2015), using the following databases in Ovid: Medline® and Medline® In-Process (PubMed), Embase (Ovid), EconLit (EBSCOhost) and the National Health Service Economic Evaluation Database (NHS EED), and a ‘grey literature’ search, were conducted to identify existing criteria from the payer perspective. The criteria assessed by existing frameworks and guidelines were collated; the most commonly reported criteria were considered for inclusion in the framework. A mnemonic was conceived as a memory aide to summarise these criteria.
Results
Overall, 41 publications were identified as potentially relevant to the objective. Following further screening, 26 were excluded upon full-text review on the basis of no framework presented (n = 13), redundancy (n = 11) or abstract only (n = 2). Frameworks that captured criteria developed for or utilised by the pharmaceutical industry (n = 5) and reimbursement guidance (n = 10) were reviewed. The most commonly identified criteria—unmet need/patient burden, safety, efficacy, quality-of-life outcomes, environment, evidence quality, budget impact and comparator—were incorporated into the summary framework. For ease of communication, the following mnemonic was developed: BEACON (Burden/target population, Environment, Affordability/value, Comparator, Outcomes, Number of studies/quality of evidence).
Conclusions
The BEACON framework aims to capture the ‘essence’ of payer requirements by addressing the most commonly described criteria requested by payers regarding the introduction of a new pharmaceutical.
Similar content being viewed by others
There are a variety of existing frameworks and guidelines that can be used by payers (budget holders) to assess new pharmaceutical therapies. However, these tools are not designed to inform internal decision making within a pharmaceutical company, involving multiple stakeholders throughout drug development. |
This review of existing frameworks and guidelines identified common criteria for decision making relating to new pharmaceuticals from the payer perspective: burden/unmet need, safety, efficacy and quality-of-life outcomes, environment, evidence quality, budget impact and comparator. |
We developed a new framework—BEACON—which could be used to guide the development of a new pharmaceutical from the payer perspective, to effectively communicate payer needs to different functions or stakeholders within pharmaceutical companies and to inform global decision making within a pharmaceutical company. |
1 Background
The traditional pharmaceutical development model focusses on building the evidence to meet registration requirements for regulatory approval (e.g. the US Food and Drug Administration [FDA] or European Medicines Agency [EMA]) [1, 2]. However, pharmaceutical companies are increasingly aware that regulatory approval is not the final hurdle and that payers’ (i.e. organisations that fund healthcare for patients, such as insurers or national health systems) needs must also be addressed [1–3]. Clinical societies such as the American Society of Clinical Oncology have also recognised the need to communicate more widely on therapy value (beyond solely clinical benefit) to aid treatment decision making, recently publishing a conceptual framework to assess the value of cancer treatment options [4].
Payers need to carefully consider the optimal allocation of limited healthcare resources to their patient population; these decisions are complex and must take practical and budgetary considerations into account [5]. In many countries, these multifaceted decisions are enabled through a comprehensive health technology assessment (HTA), which consolidates the medical, economic, social and ethical implications of a new healthcare intervention [4–9]. Although recent efforts from international bodies such as the European Network for Health Technology Assessment (EUnetHTA) aim to standardise data requirements across Europe, complete transferability or standardisation of decision making is not possible, because of intrinsic differences between countries in terms of public healthcare expenditure, healthcare system structures or treatment pathways [2, 7]. Additionally, it is acknowledged that payer requirements not only vary between countries, but can also vary within countries, at regional and local levels [2, 3].
Demonstration of value to payers globally is therefore a significant challenge, which is further complicated by the need to address the requirements of the multiple internal stakeholders involved in pharmaceutical development. For instance, during the initial stages of clinical development (e.g. phase I or II), the main focus is on the safety and efficacy of a healthcare product. However, payer requirements should also be taken into consideration even at this early stage, e.g. defining a specific target population with an unmet need and identifying the appropriate clinical outcomes. During the later stages of development (phase III onwards), the same principles apply from the payers’ perspectives; however, other requirements such as improved quality of life (QoL) and added clinical benefits over current therapies are also taken into consideration to determine how a healthcare product will provide incremental value in comparison with existing treatments. Given the time-consuming nature of clinical development and the resource use associated with it, it is imperative that the right decisions are made in order to pursue healthcare products that meet payers’ needs. However, within pharmaceutical companies, there is a broad array of functions integral to pharmaceutical development (medical, commercial, patent, manufacturing, drug safety, regulatory, etc.) that may have conflicting interests, which are not necessarily aligned with payer needs. It is widely acknowledged that barriers in communication can exist across these functions [10], which may impede the incorporation of the payer perspective throughout development.
This has been acknowledged by other bodies (e.g. HTA bodies); thus, initiatives such as the Shaping European Early Dialogues (SEED) project are currently ongoing in order to inform pharmaceutical companies of specific payer needs through early discussions. The project (sponsored by the European Commission) is a consortium of 14 HTA bodies from ten countries, led by Haute Autorité de Santé (HAS). The objective of this project is to improve collaboration and exchange of information between HTA bodies and pharmaceutical companies during initial phases of clinical development (e.g. phase I or II) in order to overcome any potential limitations of national reimbursement or to inform on specific requirements of HTA bodies for different types of data [11, 12]. While initiatives such as the SEED project are necessary, they also emphasise the importance of internal alignment of stakeholders within pharmaceutical companies in order to effectively cooperate to meet payers’ needs.
Aligning pharmaceutical development with the requirements of payers will increase the probability of success and ensure timely access for patients [2, 3]. Integrating the needs of the payer into pharmaceutical development requires consideration and understanding of the payer perspective across the entire organisation. However, within global pharmaceutical companies, there can be considerable confusion regarding the varying requirements of reimbursement agencies and payers across jurisdictions [2, 13]. Similarly, although frameworks have been developed that propose criteria to be used in the assessment and evaluation of new pharmaceuticals, the proposed criteria vary widely across these frameworks. We therefore sought to develop a summary framework that captures the ‘essence’ of international payer requirements, which could be used to guide the development of a new pharmaceutical from the payer perspective, to effectively communicate payer needs and to inform global decision making within a pharmaceutical company. To the best of our knowledge, no previous publication has aimed to summarise the criteria that capture payer requirements from an international perspective.
2 Methods
The primary objective of this research was to inform the development of a new framework through identification of existing criteria of tools, guidelines and frameworks (henceforth collectively referred to as frameworks) from the published literature. Although many frameworks consist of four core components—identification of criteria, measurement, valuation and aggregation—this manuscript explores only the identification of criteria from existing frameworks. The criteria assessed by existing frameworks were collated, and the most commonly reported criteria that were deemed to be of significance from the payer perspective were considered for inclusion in the summary framework. To aid in the recall and utilisation of the framework by pharmaceutical companies, a mnemonic was developed that captured the criteria summarised by the framework.
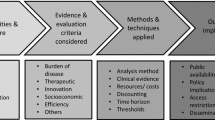
The overall development of the summary framework to date is outlined in Fig. 1.
2.1 Pilot Conceptual Framework
The first stage of the research involved developing a pilot framework. A pilot conceptual framework, termed ‘PICOP’ (Population, Intervention, Comparator, Outcomes and Price), was developed on the basis of the existing PICO (Population, Intervention, Comparator, Outcomes) framework commonly used in academia to guide the formulation of research questions [14]. This initial framework was developed on the basis of internal discussions within the market access team at Mundipharma International Limited. It was created to capture the main discussion points within the team following multiple reviews of therapies either from a business development perspective (i.e. licensing deals or partnerships with other pharmaceutical companies) or the clinical study design context. The pilot framework aimed to capture the key criteria considered by payers, and it can be summarised as follows:
-
Population: is the population well defined, and does it have a clear unmet need?
-
Intervention budget impact: what will payers perceive as the budget impact?
-
Comparator: will clinical data be available versus the relevant comparator/standard of care?
-
Outcome: are the clinical endpoints and outcomes appropriate and meaningful?
-
Price: is the price justifiable on the basis of these and other factors?
The pilot framework was presented and applied at an international advisory board meeting (in Vienna, December 2014). The members of the advisory board were all leaders in their respective fields, with the vast majority having more than 20 years of related experience. The advisory board focused on considerations in the development of new therapies, but clinical and regulatory experts were also invited to provide specialised input. The advisory board included a mix of health economic experts (n = 14), clinicians (n = 3) and regulatory personnel (n = 1) from Brazil, Canada, France, Germany, Italy, Mexico, the Netherlands, Spain, Sweden, the UK and the USA, all of whom were invited to participate as key opinion leaders in their respective fields. Of those in attendance, a panel of health economic and clinical experts, including three of the authors of this publication (CDM, OP and RG) [Canada: n = 1; France: n = 2; Germany: n = 1; Spain: n = 1; UK: n = 2; USA: n = 3] provided formal feedback via a post-meeting questionnaire (see “Appendix 1”). The overall response to the framework was positive, with the majority of participants indicating that the framework captured all (n = 2) or most (n = 8) of the key dimensions that would be considered by a payer during evaluation of a new pharmaceutical.
The pilot framework was also presented to and utilised by different functional teams within an international pharmaceutical company (Mundipharma International Limited; see the Acknowledgments section). The tool was used to engage with a number of different functions, including business development, regulatory, medical science, marketing and medical affairs. These findings indicated that the pilot conceptual framework may be applicable to the assessment of pharmaceuticals from the payer perspective and was a worthwhile endeavour; however, further validation of the criteria to be included was required.
2.2 Literature Review
To ensure that the tool captured the criteria that were of importance to payers globally, a review of the published literature was conducted to identify existing frameworks. The structured search was conducted electronically using the following databases in Ovid (Ovid Technologies, Inc.): Medline® and Medline® In-Process (PubMed), Embase (Ovid), EconLit (EBSCOhost) and the National Health Service Economic Evaluation Database (NHS EED). The search was limited to the English language only. The search was limited to a 5-year time horizon (from 2010 to May 2015) to identify the most up-to-date literature; it was assumed that more recent publications would refer back to existing tools (published prior to 2010). The search string is presented in “Appendix 2”. Additionally, the reference list of each publication was reviewed to identify any additional publications of interest, and grey literature was identified from a broad internet search using the following key terms: ‘framework’, ‘drug development’ and ‘decision making’.
Overall, 230 abstracts were screened from the structured literature review (Fig. 2); of these, 41 publications were identified as publications potentially of interest and were taken forward to full-text review. Publications of interest were required to fulfil the following inclusion criterion: publications reporting on frameworks that were developed to assess the value of a new pharmaceutical from a healthcare system, payer or pharmaceutical company perspective. A further 26 publications were excluded at full-text review. The majority of publications excluded at full-text review were conceptual papers (n = 13), which commented on the need for a framework to assess the value of a new pharmaceutical but presented no frameworks. An additional 11 publications were considered to be redundant at full-text review and were subsequently excluded, i.e. numerous publications presented risk–benefit assessments in early clinical development.
A review of HTA guidance was also conducted to understand the key criteria that national payers currently use to assess new pharmaceuticals. The review was limited to guidance from countries with well-established and publically available HTA guidelines, in order to provide an indication of the different perspectives taken in internationally influential HTA countries. This included guidance published by EUnetHTA [15], Canadian Agency for Drugs and Technologies in Health (CADTH) [16], HAS [17], Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) [8], Pharmaceutical Benefits Advisory Committee (PBAC) [9], National Institute for Health and Care Excellence (NICE) [6], Belgian Health Care Knowledge Centre (KCE) [18, 19] and Tandvårds- och läkemedels-förmånsverket (TLV) [20].
3 Results
3.1 Evaluation of Existing Tools and Frameworks
In total, five frameworks and ten HTA guidelines were reviewed. Although this list was not exhaustive, the frameworks considered in this paper represent a sample of those utilised by the pharmaceutical industry to align to payer requirements. Additionally, a number of decision-making approaches were identified, such as risk–benefit analyses and multicriteria decision analysis (MCDA); these approaches were captured, where possible, through the evaluation of representative tools, e.g. the Clinical Utility Index and the Evidence and Value: Impact on Decision Making (EVIDEM) framework, respectively [21, 22]. The following frameworks were included within this review:
-
Clinical Utility Index: a quantitative risk–benefit assessment of the value of a new medical intervention.
-
Evaluation of Pharmaceutical Innovations with Regard to Therapeutic Advantage (EVITA): a tool for early evaluation of the additional therapeutic value of a drug.
-
International Society for Pharmacoeconomics and Outcomes Research/Academy of Managed Care Pharmacy/National Pharmaceutical Council (ISPOR-AMCP-NPC) Good Practice Task Force questionnaire: to assess the relevance and credibility of observational studies.
-
EVIDEM framework: to assess healthcare interventions, using an MCDA core model and context-specific decision criteria.
-
Institute for Clinical and Economic Review value framework: an approach to assessing the value of a new healthcare intervention in the USA.
-
Cancer Drugs Fund (CDF) assessment: a budget allocation prioritisation tool.
-
Ontario Decision Determinants (DD) framework: a complementary framework to guide HTA in Ontario, Canada.
-
HTA guidance published by EUnetHTA, CADTH, HAS, IQWiG, PBAC, KCE, TLV and NICE.
These existing frameworks and guidance were reviewed and categorised on the basis of (1) their purpose or application; and (2) their perspective. Each framework was evaluated to identify any criteria that were of relevance from the payer perspective, to be incorporated into the new conceptual framework.
3.2 Categorisation of Frameworks
The frameworks were broadly classified as non-HTA or HTA frameworks:
-
1.
Non-HTA decision-making frameworks: evidence-based, academic or healthcare system perspective to assess the quality of evidence.
-
2.
HTA guidance: healthcare system payer perspective, assessing the clinical, economic, social and ethical implications of a new pharmaceutical to aid HTA decision making.
However, it was acknowledged the majority of the frameworks feed into the HTA process, and a degree of overlap exists.
3.3 Non-HTA Decision-Making Frameworks
A summary of the criteria considered in the ‘non-HTA decision-making’ frameworks is provided in Table 1. As can be seen in the table, there is a wide variety of different approaches taken. Some frameworks utilise a more clinical approach (such as the Clinical Utility Index), whereas others take an approach that is closer to the payer perspective.
Risk–benefit frameworks, such as the approach taken by the Clinical Utility Index, are commonly used by pharmaceutical companies and regulatory agencies in drug development and pre-approval. The Clinical Utility Index combines multiple attributes of a product profile with appropriate weighting to generate a single utility value, and it has previously been implemented in early exploratory development programmes or at the ‘proof of concept’ stage, i.e. to assess whether the available evidence suggests that success is ‘reasonably likely’ on the basis of the presence of key success attributes and lack of failure attributes [21, 27]. However, these risk–benefit tools, such as the Clinical Utility Index, may inform the likelihood of clinical efficacy or safety but do not necessarily link to the commercial viability of the intervention: estimates suggest that in 2005/2006, approximately 50 % of pharmaceuticals that achieved proof of concept proceeded to development. Of these, the registration rate varied from approximately 20 % for cardiovascular drugs to 8–12 % for oncology drugs, despite oncology drugs having the highest rate of successful ‘proof of concept’ [27].
It has also been acknowledged that appropriate comparative clinical evidence, demonstrating an additional therapeutic value of a pharmaceutical, may be lacking at the time of the launch because of the use of inadequate comparators, control groups or outcomes. The EVITA tool was developed as a simple, transparent tool for early evaluation of the additional therapeutic value of a pharmaceutical. The tool assesses clinical benefit, e.g. improved efficacy and reduced adverse events, and follows an algorithm that captures the relevance of outcomes and the strength of evidence [23].
Furthermore, the volumes of data required to demonstrate the incremental benefit of a new pharmaceutical are increasing. A number of tools have been developed to aid in the critical appraisal of evidence, such as an assessment tool for prospective observational studies developed by an ISPOR task force [24]. This tool consists of 33 questions to assess the relevance and credibility of a study, and it was developed to allow an individual to critically appraise an individual study to assess whether it is of sufficient quality to be included within a body of evidence for a new technology appraisal.
Two further approaches—MCDA and a US-based payer assessment framework—were identified, which were considered to be more closely aligned with the purpose of the pilot conceptual framework (i.e. to take into account budgetary factors that can influence decision makers in an ever-increasingly resource-constrained environment), rather than focusing on clinical data. Moreover, MCDA takes into consideration multiple criteria and scores each criterion on the basis of importance or relevance to generate an overall estimate [28]. An MCDA-based decision-making approach has already been piloted by the Office of Health Economics (OHE) for the assessment of orphan indications in the UK [29], and in the USA, there is an MCDA-based decision-making framework for prioritisation of vaccines [28]. However, it is important to note that this type of approach to assessments is not widely used by major HTA bodies such as HAS, IQWIG or NICE. The EVIDEM framework has been developed to assess healthcare interventions using an MCDA core model and context-specific decision criteria with the aim of bridging HTA and MCDA approaches [22]. EVIDEM assigns 15 decision-making determinants to form an MCDA value matrix (Table 1). Each criterion is scored, and a weight is allocated to generate a final score. However, there are some components that are not quantifiable, such as ethical factors (opportunity costs, population priority, access and fairness) and context (system capacity and appropriate use of an intervention). Furthermore, some methodological issues have also been identified that can arise when applying this method to HTA—in particular, choosing the criteria to include in the decision process, choosing an appropriate scoring or weighting method, or modelling scores and weights [30, 31]. Although interest in the MCDA approach has been expressed, there is a lack of guidance on the appropriate approach to conducting such an analysis, and the complexity and length of the analysis may impact upon its wider utilisation.
A US-based payer assessment framework is also being developed by the Institute for Clinical and Economic Review [26]. This value framework is a categorical, part quantitative, part qualitative approach to assessing the value of a pharmaceutical. The tool aims to improve the reliability and consistency of decisions by payers and to provide the basis for transparent discussions between the pharmaceutical company and decision makers when value is being considered [26].
3.4 HTA Guidance
Established HTA agencies (e.g. CADTH, HAS, IQWiG, PBAC, KCE, TLV and NICE) inform decisions on coverage and reimbursement for a new pharmaceutical. Both comparative effectiveness and cost effectiveness are considered within these assessment procedures, which are detailed in Table 2.
Some frameworks place a greater emphasis on certain criteria—for example, NICE in the UK, PBAC in Australia, KCE in Belgium and TLV in Sweden focus on the economic element of the review in cost–utility or cost-effectiveness analyses presented by pharmaceutical companies, alongside assessments of the comparative clinical benefit [6, 9, 18–20, 28]. All of the frameworks consider life-years gained or quality-adjusted life-years (QALYs) as appropriate measures of effect in economic analyses; however, it is worth pointing out that only NICE uses a specific threshold for each QALY gained (i.e. £20,000–£30,000) [6], and TLV uses an individual’s willingness to pay per QALY gained threshold rather than a set budgetary threshold, while PBAC and KCE do not use an explicit cost-effectiveness threshold when assessing new pharmaceuticals [9, 18, 32]. Despite that, it is important to note that within single countries, there may be different payer bodies, depending on the geography or the nature of the pharmaceutical. For example, the NICE assessment procedure is not applied to all new pharmaceuticals launched in the UK and, in addition, the CDF was established in 2010 to provide access to cancer therapies that are not approved or not reviewed by NICE [33]. The assessment criteria used by the CDF, in its current form, are slightly different from those used by NICE, mainly prioritising the magnitude of survival and toxicity, as well as unmet need and strength of evidence over costs and cost effectiveness (Table 2) [33, 34]. However, it is worth noting that a new assessment process led by NICE for the appraisal of cancer drugs is expected in 2016 [35].
In other established HTA countries in Europe, there is a different approach by payers to the assessment of new technologies. In Germany, there is a clear separation of the assessment of added clinical benefit from the assessment of cost effectiveness [8]. In particular, IQWiG is usually commissioned by the Gemeinsamer Bundesausschuss (G-BA) to conduct an early benefit assessment of a health technology to determine whether there is proof of added or comparable patient-relevant clinical benefit. Price negotiations are completed only following a decision on the added patient-relevant clinical benefit of a pharmaceutical. In exceptional cases, i.e. when pricing negotiations fail to reach an agreement between a pharmaceutical company and the national statutory health insurance association, a health economic analysis may be conducted [8]. On the other hand, in France, clinical assessments are carried out first during the HTA of a new pharmaceutical, followed by economic evaluations if an appropriate level of clinical benefit is achieved and if the new pharmaceutical is anticipated to have a significant budget impact on the healthcare system. However, their outputs are used to inform different decisions. For example, the added clinical benefit of a medical intervention is used as a criterion for reimbursement decisions, while cost-effectiveness results are used during pricing negotiations [36].
Because of the recognised differences in approaches across Europe, the European body EUnetHTA has also developed a core framework for the assessment of pharmaceuticals, which embodies all of the core criteria typically used across Europe (Table 2).
Furthermore, in addition to national HTA processes, extra guidance has been developed to complement the national HTA process. For example, in Canada, in addition to a national body review by the CADTH [16], there are regional drug assessments, such as those conducted by the Ontario Health Technology Advisory Committee (OHTAC). OHTAC has developed its own framework for assessment (the Ontario DD framework), which also encompasses many of the national-level assessment criteria but explicitly includes an assessment of the feasibility of implementation in the current healthcare system, which is important for regional or local-level decision making [37].
The identified frameworks assess a broad range of criteria, each of which has differing subcriteria or associated key questions, which vary depending on the perspective taken and the purpose of the tool or framework. The criteria assessed by each framework were categorised into 11 broader criteria: efficacy outcomes, safety outcomes, QoL outcomes, unmet need, environment, evidence quality, cost, comparator, ethics, indication and pharmaceuticals. All of the frameworks consider the clinical safety and efficacy outcomes (n = 15) as a key criterion, whereas fewer consider the dosing or formulation of a new pharmaceutical (n = 9) or ethics (n = 8); this is summarised in Fig. 3, which provides an overview of the criteria that are currently covered by the existing tools discussed in the preceding sections.
3.5 Development and Application of the BEACON Framework
The frameworks outlined in Tables 1 and 2 were reviewed, and all criteria that were relevant from the payer perspective were considered for inclusion within the new framework (Fig. 3). The selection of the criteria deemed relevant to payers was based on a consensus from all authors of the manuscript.
As the overall objective was to develop a simple communication tool, the overall number of discrete criteria included were limited by grouping similar criteria into broader single criterion. For instance, the most frequently identified criteria were efficacy (n = 15), safety (n = 15) and QoL (n = 13), all of which represent outcomes; therefore, these were combined as a single criterion. Other criteria such as comparator (n = 13), unmet need (n = 12), cost (n = 12) and evidence quality (n = 11) were also frequently assessed by the frameworks reviewed and thus were considered by the authors to be important and distinct enough to warrant separate categories. Indication (n = 10), environment (n = 10), pharmaceutics (n = 9) and ethics (n = 8) were the least frequently identified criteria. Indication, pharmaceutics and ethics were not regarded as unique drivers of decision making from the payer perspective. Consequently, these three criteria were grouped with other categories defined above. Key aspects for ‘indication’, which are required for regulatory licensing, were incorporated under the headings of common categories that were also likely to be of interest to the payer: ‘unmet need’ and ‘outcomes’. Pharmaceutics, which included dosing formulation and pharmacokinetics, were considered potential influencers on the appropriateness of comparators and outcomes, and thus were included under the ‘comparator’ and ‘outcomes’ categories. Ethical considerations were taken into account under the ‘environment’ heading. Environment—which takes into account aspects such as clinical guidelines, drug reimbursement and healthcare systems—which are of importance to payers in their decision making, was also included as a single criterion.
Therefore, overall, six broad categories to be included in the final communication framework were identified from the existing frameworks in descending order of frequency: outcomes, comparator, unmet need (or burden/target population), affordability/value and cost (to encompass the broad range of considerations relating to costs, cost effectiveness and budgetary implications, which are of importance to the payer), number of studies/evidence quality, and environment.
The proposed list of key criteria for inclusion in the framework and the key questions and sub-questions to be answered are detailed in Table 3.
For ease of communication of this framework, we propose the following mnemonic, based on the identified broad categories: BEACON (Burden/target population, Environment, Affordability/value, Comparator, Outcomes, Number of studies/quality of evidence). The BEACON mnemonic was perceived to be simple to remember and reflective of the purpose of the summary framework, as the term has connotations of ‘guiding’ stakeholders through complex payer requirements.
It is recognised that the proposed BEACON framework provides a broad set of criteria and that in practice, the sub-questions are likely to be adapted to the respective situation, e.g. the stage of the pharmaceutical life cycle, the country and local payer priorities.
As a payer’s perception of the value of a pharmaceutical may be influenced by a number of factors, we propose that all criteria are assessed within the context of an overarching value statement and target product profile, i.e. to differentiate between decisions on expensive pharmaceuticals that are associated with a significant clinical benefit and decisions on pharmaceuticals whose clinical efficacy and safety are equivalent to those of the standard of care but that are associated with a cost saving.
Figure 4 demonstrates how the BEACON framework could be applied when payer-focused decisions are being made regarding a biosimilar, orphan drug product or high-cost oncology product (all of which are hypothetical products). A colour-coding system is proposed to highlight key areas where focus is required in the development of the new pharmaceutical, in a simple manner. It is recognised that there will be differences between regions—therefore, this assessment would need to be undertaken from different perspectives—and also that, depending on the decision problem, greater complexity may be required than the example applications presented in Fig. 4.
On the basis of this description of the benefits of the new pharmaceuticals, pharmaceutical companies can then effectively communicate the potential value of a new in-development pharmaceutical to a range of stakeholders (both internally and externally) in order to shape the future development of the pharmaceutical.
4 Discussion
A variety of tools and guidelines are used by payers to assess new pharmaceutical therapies. Each of these is important within a certain context, whether this is to perform early evaluations of a pharmaceutical’s additional therapeutic benefits (e.g. EVITA) or to inform decisions on reimbursement (i.e. HTA guidance). However, these tools are not designed for the purposes of internal decision making involving multiple stakeholders throughout all stages of pharmaceutical drug development.
From the frameworks identified in this manuscript, several key themes and common criteria were identified. These included unmet need/patient burden, environment, budget impact or cost considerations, safety, efficacy, QoL outcomes, comparator and overall quality of evidence.
In contrast to the existing frameworks and tools, the proposed BEACON framework and mnemonic allow the identification of criteria to guide the development of a pharmaceutical from a payer perspective, to aid with communication and internal decision making within pharmaceutical companies. For instance, value frameworks developed by organisations such as the American College of Cardiology and American Heart Association (ACC and AHA), the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) all include clinical efficacy and safety criteria assessments, as well as cost effectiveness and budget impact, but they do not take into account disease burden, market access opportunities or QoL outcomes. Moreover, these approaches aim to include user preferences by assigning weights or scores to the various dimensions they assess, which in turn may produce inconsistent results [39]. On the other hand, the BEACON framework uses a colour-coding system, which can be used to highlight areas where potential market access challenges might arise and where more focus is required in the pharmaceutical development. The colour-coding system can also be used to communicate these challenges to other functional teams within a pharmaceutical company in a simplified manner and to ensure that a payer-led perspective is integrated throughout all stages of development at all team levels.
Given the many different criteria and the different emphasis of payers globally, a framework such as BEACON, which consolidates the different needs, will help multinational companies (who need to consider a global perspective) make informed decisions. In addition, communicating the value of a new pharmaceutical by using this framework will aid the different functions and stakeholders within pharmaceutical companies to understand the payer perspective and incorporate that into decision making for pharmaceutical development or in-licensing. Applying this framework when assessing the value of a pharmaceutical will also enable a consistent approach, to maximise the chance of successful development and patient access. It is anticipated that this framework could be used at multiple stages of the pharmaceutical life cycle, to take into account the changing external landscape and to ensure that the development strategy is refined on the basis of the latest payer needs. Additionally—although this was not explored within this manuscript—it is assumed that the framework may be broadly applicable to the assessment of other healthcare interventions, e.g. medical devices.
To inform decision making in practice, it is likely that the use of the BEACON framework will be based on research such as discussions with payers, reviews of similar drug case studies, development of health economic models and real-world evidence.
It is recognised that the proposed BEACON framework provides a broad set of criteria and that an adapted version of BEACON that incorporates specific local payer requirements may be required when decisions are being made for local application. Implementation of the framework should never be a substitute for other review processes and the use of more complex guidelines or tools. Given BEACON’s potential to facilitate internal alignment within a pharmaceutical organisation, the tool could also be used to improve early discussions between pharmaceutical companies and payers. For instance, the SEED project has been recently initiated with the aim of advising pharmaceutical companies how to optimise their development strategies in order to meet payers requirements. Some of the main topics covered by the SEED project are also covered by BEACON; these include the target population, comparators, clinical trial design (e.g. duration, drug dosage), clinical endpoints, subgroup analyses and economic analyses [11, 12]. This suggests that the broad nature of the criteria incorporated into the BEACON framework could potentially help pinpoint areas that should be discussed within the context of a more complex tool.
The framework presented here is based on a review of the literature and distillation of the key payer requirements into a core set of criteria. As the review of the published literature was limited to a 5-year time horizon and a focused review of established HTA guidance, it is acknowledged that the core set of criteria presented within this manuscript is not an exhaustive list of criteria that may be of consideration for payers. Therefore, additional research needs to be conducted to further validate the proposed framework, to assess its sensitivity and generalisability and how the framework performs in terms of identifying products that have a high probability of market access success. In addition, further consideration should be given to how the criteria within the tool are scored and whether weighting of the different categories is required in order to effectively communicate value and inform decision making. Finally, there is a potential need to further develop the framework to take into account internal company resources, long-term strategic goals, pipeline balance and spread across therapy areas and stages of clinical development, all of which can also influence internal decision making on pharmaceutical development.
5 Conclusions
Both pharmaceutical companies and payers are under increasing pressure to meet the growing healthcare needs of society. To ensure that innovative pharmaceuticals are reaching the market, and to ensure timely access for patients, pharmaceutical companies need to focus on intelligent innovation by instilling payer decision makers’ needs through the entire development process. The introduction of a framework such as BEACON, as proposed here, will provide a tool to guide pharmaceutical development from the payer perspective.
References
Grignolo A. Collaboration and convergence: bringing new medicines to global markets in the 21st century. Ther Innov Regul Sci. 2013;47(1):8–15.
Sansom L. Assessing the value of medicines. Pharm Med. 2010;24(2):89–92.
Epstein RS, Sidorov J, Lehner JP, Salimi T. Integrating scientific and real-world evidence within and beyond the drug development process. J Comp Eff Res. 2012;1(1 Suppl. 1):9–13.
Schnipper LE, Davidson NE, Wollins DS, Tyne C, Blayney DW, Blum D, Dicker AP, Ganz PA, Hoverman JR, Langdon R, Lyman GH, Meropol NJ, Mulvey T, Newcomer L, Peppercorn J, Polite B, Raghavan D, Rossi G, Saltz L, Schrag D, Smith TJ, Yu PP, Hudis CA, Schilsky RL, American Society of Clinical Oncology. American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33(23):2563–77. doi:10.1200/JCO.2015.61.6706.
Stafinski T, Menon D, Philippon DJ, McCabe C. Health technology funding decision-making processes around the world: the same, yet different. Pharmacoeconomics. 2011;29(6):475–95.
National Institute for Health and Care Excellence. Guide to methods of technology appraisal 2013. Published April 2013. http://www.nice.org.uk/article/pmg9/chapter/foreword. Accessed June 2015.
Hao Y, Thomas A. Health technology assessment and comparative effectiveness research: a pharmaceutical industry perspective. Expert Rev Pharmacoecon Outcomes Res. 2013;13(4):447–54.
Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen. General methods version 4.2. Published April 2015. https://www.iqwig.de/download/IQWiG_General_Methods_Version_%204-2.pdf. Accessed Mar 2016.
Australian Government Department of Health and Aging. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee. Published 2008. http://www.ispor.org/PEguidelines/source/Australia-Guidelines-for-preparing-submissions-to-the-Pharmaceutical-Benefits-Advisory-Committee-2008.pdf. Accessed Aug 2015.
Pinto MB, Pinto JK. Project team communication and cross-functional cooperation in new program development. J Prod Innov Manage. 1990;7(3):200–12.
Meyer F. Multi-HTA early dialogues: EUnetHTA, SEED, HTA Network. Presented at ISPOR 18th Annual European Congress, Milan, Italy, November, 2015. http://www.ispor.org/Event/GetReleasedPresentation/450. Accessed Mar 2016.
Harousseau J-L, Pavlovic M, Mouas H, Meyer F. PHP275 Shaping European early dialogues: the SEED project. Published at ISPOR 18th Annual European Congress, Milan, Italy, November, 2015. http://www.ispor.org/research_pdfs/51/pdffiles/PHP275.pdf. Accessed Mar 2016.
Gispen-De Wied CC, Leufkens HGM. From molecule to market access: drug regulatory science as an upcoming discipline. Eur J Pharmacol. 2013;719(1–3):9–15.
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14:579.
European Network for Health Technology Assessment. Methods for health economic evaluations. Published May 2015. http://www.eunethta.eu/sites/5026.fedimbo.belgium.be/files/2015-04-29-ECO-GL_Final%20version_0.pdf. Accessed June 2015.
Canadian Agency for Drugs and Technologies in Health. Guidelines for the economic evaluation of health technologies: Canada. Published 2006. http://www.ispor.org/PEguidelines/source/HTAGuidelinesfortheEconomicEvaluationofHealthTechnologies-Canada.pdf. Accessed Aug 2015.
Haute Autorité de Santé. Choices in methods for economic evaluations. Published Oct 2012. http://www.has-sante.fr/portail/upload/docs/application/pdf/2012-10/choices_in_methods_for_economic_evaluation.pdf. Accessed June 2015.
Belgian Health Care Knowledge Centre (KCE). Belgian guidelines for economic evaluations and budget impact analyses: second edition. Published Dec 2015. https://kce.fgov.be/sites/default/files/page_documents/KCE_183_economic_evaluations_second_edition_Report3.pdf. Accessed Mar 2016.
Belgian Health Care Knowledge Centre (KCE). Search for evidence and critical appraisal health technology assessment (HTA). Published Sept 2007. https://kce.fgov.be/sites/default/files/page_documents/kce_process_notes_hta.pdf. Accessed Mar 2016.
The Dental and Pharmaceutical Benefits Agency in Sweden (TLV). General guidelines for economic evaluations from the Pharmaceutical Benefits Board. Published May 2003. http://www.tlv.se/Upload/English/Guidelines-for-economic-evaluations-LFNAR-2003-2.pdf. Accessed Mar 2016.
Ouellet D. Benefit-risk assessment: the use of clinical utility index. Expert Opin Drug Saf. 2010;9(2):289–300.
Evidence and value: impact on decision making (EVIDEM). Conceptual background, definitions, design and instructions. Published Dec 2014. https://www.evidem.org/docs/2015/EVIDEM-v2-4-Decision-criteria-conceptual-background-definitions-and-instructions-Dec-2014.pdf. Accessed June 2015.
Püntmann I, Schmacke N, Melander A, Lindberg G, Mühlbauer B. EVITA: a tool for the early evaluation of pharmaceutical innovations with regard to therapeutic advantage. BMC Pharmacol Toxicol. 2010;10(1):5.
Berger M, Martin B, Husereau D, et al. A questionnaire to assess the relevance and credibility of observational studies to inform healthcare decision making: an ISPOR-AMCP-NPC Good Practice Task Force report. Value Health. 2014;17:143–56.
Carrothers TJ, Hodge FL, Korsan RJ, Poland WB, Dykstra KH. Decision-making in drug development: application of a clinical utility index. Clinical trial simulations—applications and trends. Heidelberg: Springer Verlag; 2011. p. 85–107.
Pearson SA, Institute for Clinical and Economic Review (ICER). (2015) Framework for payer assessment of the value of new technologies: a US approach. Seminar briefing 16. Office of Health Economics Research (OHE). Published Feb 2015.
Cartwright ME, Cohen S, Fleishaker JC, Madani S, McLeod JF, Musser B, et al. Proof of concept: a PhRMA position paper with recommendations for best practice. Clin Pharmacol Ther. 2010;87(3):278–85.
Marsh K, Lanitis T, Neasham D, Orfanos P, Caro J. Assessing the value of healthcare interventions using multi-criteria decision analysis: a review of the literature. Pharmacoeconomics. 2014;32(4):345–65.
Sussex J, Rollet P, Garau M, Schmitt C, Kent A, Hutchings A. A pilot study of multicriteria decision analysis for valuing orphan medicines. Value Health. 2013;16(8):1163–9.
Thokala P, Duenas A. Multiple criteria decision analysis for health technology assessment. Value Health. 2012;15(8):1172–81.
Thokala P, Marsh K. Choosing appropriate multi-criteria decision analysis technique(s) to support health care decisions: issues and considerations. 37th Annual Meeting of the Society for Medical Decision Making, Missouri, USA; 2015.
Paris V, Belloni A. Value in pharmaceutical pricing country profile: Australia. OECD Health Working Papers, No. 63, OECD Publishing. 2013. http://apps.who.int/medicinedocs/documents/s21368en/s21368en.pdf. Accessed June 2016.
NHS England. The Cancer Drug Fund. http://www.england.nhs.uk/ourwork/pe/cdf/. Accessed Aug 2015.
National Health Service Commissioning board. National Cancer Drugs Fund prioritisation tool. Appendix E. https://www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=0CCgQFjAA&url=http%3A%2F%2Fwww.blueteq.com%2Fcdf%2FForms%2FAppendix%2520E%2520National%2520Prioritisation%2520tool.docx&ei=v95mVem7D8jlsASzhoCQCg&usg=AFQjCNH_P1RnHUE2Spjm8cEwvPRqmH7CUQ&bvm=bv.93990622,d.ZGU. Accessed June 2015.
National Institute for Health and Care Excellence (NICE). Faster access to effective cancer treatments through new Cancer Drugs Fund. Published 16 Mar 2016. 2016. https://www.nice.org.uk/news/article/faster-access-to-effective-cancer-treatments-through-new-cancer-drugs-fund. Accessed Mar 2016.
Ghabri S, Hamers FF, Josselin JM. Exploring uncertainty in economic evaluations of drugs and medical devices: lessons from the first review of manufacturers’ submissions to the french national authority for health. PharmacoEconomics. 2016;34(6):617–24.
Ontario Health Technology Advisory Committee (OHTAC). Decision-making process for the development of evidence-based recommendations. Decision determinants guidance document. Revised Sept 2010. http://www.hqontario.ca/en/mas/tech/pdfs/2011/guide_decision.pdf. Accessed June 2015.
Haute Autorité de Santé. Pricing and reimbursement of drugs and HTA policies in France. Published Mar 2014. http://www.has-sante.fr/portail/upload/docs/application/pdf/2014-03/pricing_reimbursement_of_drugs_and_hta_policies_in_france.pdf. Accessed Aug 2015.
Neumann PJ, Cohen JT. Measuring the value of prescription drugs. N Engl J Med. 2015;373(27):2595–7.
Acknowledgments
The authors would like to acknowledge Matthew Hirst, Francois Bernard, Antonio Lervolino, James Kenworthy, Alexandra Staufer, Ashok Jha and Charlotte James (Mundipharma International Limited); Professor Ron Akehurst (BresMed, University of Sheffield); Jean-Gabriel Castaigne (Amgen); Jason Ward (IMS Consulting Group); and Georg Toufar (Kronberg Associates) for their contributions to the framework. They would also like to acknowledge Luke Skinner (Adelphi Values Limited) for medical writing assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
WCND is an employee of Mundipharma International Limited. AE and LH are employees of Adelphi Values Limited (Adelphi Values Limited received budgetary compensation for involvement in the manuscript development). OP, CDM, RG and MJP participated in the advisory board meeting (in Vienna in December 2014); they subsequently voluntarily participated in the work on this manuscript, did not receive any honoraria for this manuscript and declare no conflicts of interest. OP, CDM, RG and MJP have all previously received honoraria/fees from Mundipharma International Limited for other advisory services.
Author contributions
WCND was involved in the conceptualisation of the pilot framework and the advisory board meeting. WCND, LH and AE were involved in the design of the search strategy, the conduct of the literature review and development of the manuscript and the BEACON framework. CDM, OP, RG and MJP were part of the advisory board, reviewed the pilot framework, contributed to the search strategy and research strategy, and reviewed and provided input on all drafts of the manuscript and the BEACON framework.
Appendices
Appendix 1
Advisory board post-meeting questionnaire (Vienna, December 2014)
Q1. Does the PICOP tool capture the key dimensions that determine whether payers will approve a new therapy? | |
Answer: please place a cross in ONE box only | |
Captures all | □ |
Captures most | □ |
Captures some | □ |
Captures none | □ |
Q2. Are there any critical areas you feel have not been captured? If yes, what are they? | |
Q3. Would adding a dimension on the system improve the tool? The sixth dimension on the system could cover any unique aspects of a health system that might influence payer acceptance of a therapy, e.g. uptake of novel therapies or perverse incentives | |
Answer: please place a cross in ONE box only | |
Definitely | □ |
Likely | □ |
Unlikely | □ |
Never | □ |
Q4. In the PICOP scoring system guide are the descriptions for each dimension and the definitions for scoring 1 and 5 stars clear and appropriate? | |
Answer: please place a cross in ONE box only | |
Definitely | □ |
Likely | □ |
Unlikely | □ |
Never | □ |
Q5. If not, any suggestions? | |
Q6. Overall, how useful do you think the PICOP tool is as a therapy assessment and development tool from a payer perspective? | |
Answer: please place a cross in ONE box only | |
Very useful | □ |
Useful | □ |
Slightly useful | □ |
Not useful | □ |
Q7. Would you be interested in working with Mundipharma on refining and validating the PICOP tool? | |
Answer: please place a cross in ONE box only | |
Yes | □ |
Maybe | □ |
No | □ |
Q8. Any other comments? | |
Appendix 2
Structured literature review search string
1. (‘Decision making’ or ‘health economics’ or ‘health technology assessment’ or ‘outcome assessment’ or ‘evidence based medicine’ or ‘biomedical technology assessment’ or ‘payer assessment’ or ‘early evaluation’ or ‘healthcare cost’ or ‘early benefit assessment’ or ‘risk benefit analysis’ or ‘forecasting’ or ‘reimbursement’).mp. [mp = ti, ot, ab, sh, hw, kw, tn, dm, mf, dv, nm, kf, px, rx, an, ui, tc, id, tm, ct, tx] |
2. ‘Drug development’.mp. [mp = ti, ot, ab, sh, hw, kw, tn, dm, mf, dv, nm, kf, px, rx, an, ui, tc, id, tm, ct, tx] |
3. (‘Framework’ or ‘tool’ or ‘guidelines’).mp. [mp = ti, ot, ab, sh, hw, kw, tn, dm, mf, dv, nm, kf, px, rx, an, ui, tc, id, tm, ct, tx] |
4. 1 and 2 and 3 |
5. Limit 4 to English language |
6. Limit 5 to yr = ‘2009–current’ |
7. Remove duplicates from 6 |
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Dunlop, W.C.N., Mullins, C.D., Pirk, O. et al. BEACON: A Summary Framework to Overcome Potential Reimbursement Hurdles. PharmacoEconomics 34, 1051–1065 (2016). https://doi.org/10.1007/s40273-016-0427-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-016-0427-7