Abstract
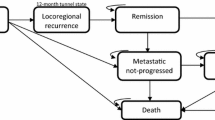
The National Institute for Health and Care Excellence (NICE) invited the manufacturer of pertuzumab (Roche) to submit evidence for the clinical and cost effectiveness of pertuzumab + trastuzumab + docetaxel for the treatment of human epidermal growth factor receptor 2-positive (HER2+) metastatic or locally recurrent unresectable breast cancer in accordance with the Institute’s Single Technology Appraisal (STA) process. The Liverpool Reviews and Implementation Group (LRiG) at the University of Liverpool was commissioned to act as the Evidence Review Group (ERG). This article summarises the ERG’s review of the evidence submitted by the manufacturer and provides a summary of the Appraisal Committee’s (AC) initial decision. At the time of writing, final guidance had not been published by NICE. The clinical evidence was mainly derived from an ongoing phase III randomised double-blind placebo-controlled international multicentre clinical trial (CLEOPATRA), designed to evaluate efficacy and safety in 808 patients, which compared pertuzumab + trastuzumab + docetaxel (pertuzumab arm) with placebo + trastuzumab + docetaxel (control arm). Both progression-free survival (PFS) and overall survival (OS) were analysed at two data cut-off points—May 2011 (median follow-up of 18 months) and May 2012 (median follow-up of 30 months). At both time points, PFS was significantly longer in the pertuzumab arm (18.5 months compared with 12.4 months in the control arm at the first data cut-off point and 18.7 versus 12.4 months at the second data cut-off point). Assessment of OS benefit suggested an improvement for patients in the pertuzumab arm with a strong trend towards an OS benefit at the second data cut-off point; however, due to the immaturity of the OS data, the magnitude of the OS benefit was uncertain. Importantly, cardiotoxicity was not increased in patients treated with a combination of pertuzumab + trastuzumab + docetaxel. The ERG’s main concern with the clinical effectiveness data was the lack of mature OS data. An additional concern of the AC was that the majority of patients in the randomised controlled trial were trastuzumab naïve, which does not reflect current clinical practice. The incremental cost-effectiveness ratios (ICERs) generated by the manufacturer’s model are considered to be commercial in confidence data and therefore cannot be published. Nevertheless, the results of the manufacturer’s probabilistic sensitivity analyses suggest that pertuzumab + trastuzumab + docetaxel has a 0 % probability of being cost effective at a willingness-to-pay of £30,000 per quality-adjusted life-year gained when compared with trastuzumab + docetaxel. The ERG believes that more realistic estimates of the ICERs are considerably higher, almost double those presented by the manufacturer. This is because the ERG believes that due to the manner in which the economic model is constructed, the additional survival benefit following disease progression that is generated for patients treated with pemetrexed + trastuzumab + docetaxel is unrealistic. At the time of writing, NICE had not made a final decision regarding this technology but had instead referred the issue of the assessment of technologies that are not effective at a zero price to their Decision Support Unit for advice.
Similar content being viewed by others
References
National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. 2008. http://www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdatedJune2008.pdf. Accessed 11 Dec 2013.
National Institute for Health and Care Excellence. Breast cancer (HER2 positive, metastatic)—pertuzumab (with trastuzumab and docetaxel) [ID523] London: NICE; 2013. http://guidance.nice.org.uk/index.jsp?action=byId&o=13815. Accessed 11 Jun 2014.
Cancer Research UK. Breast cancer incidence statistics 2010. [updated 7 November 2012]. http://www.cancerresearchuk.org/cancer-info/cancerstats/types/breast/incidence/. Accessed 24 Apr 2013.
National Institute for Health and Care Excellence. Breast cancer (HER2 positive, metastatic)—pertuzumab (with trastuzumab and docetaxel): evaluation report. http://guidance.nice.org.uk/TAG/322/Consultation/EvaluationReport/pdf/English. Accessed 11 Dec 2013.
Breast Cancer Care. Secondary Breast Cancer Taskforce. Stand up and be counted: the need for the collection of data on incidence of secondary breast cancer and survival. 2007. http://www.breastcancercare.org.uk/upload/pdf/statistics_briefing_final_0.pdf. Accessed 11 Dec 2013.
Chen L, Yalamanchi S, Waynick C, et al. Characteristics of de novo stage IV breast cancer presentation and comparison with stage IV disease relapse after adjuvant therapy. Cancer Res. 2011;71(24 Suppl 3):P1-08–23.
Dawood S, Broglio K, Ensor J, Hortobagyi GN, Giordano SH. Survival differences among women with de novo stage IV and relapsed breast cancer. Ann Oncol. 2010;21(11):2169–74.
F Foot C, Harrison T. How to improve cancer survival: explaining England’s relatively poor rates. London: The King’s Fund 2011. http://www.kingsfund.org.uk/sites/files/kf/How-to-improve-cancer-survival-Explaining-England-poor-rates-Kings-Fund-June-2011.pdf. Accessed 11 Dec 2013.
Pritchard C, Hickish T. Changes in cancer incidence and mortality in England and Wales and a comparison of cancer deaths in the major developed countries by age and sex 1979–2002 in context of GDP expenditure on health. Ecancermedicalscience. 2008;2:80.
Allemani C, Minicozzi P, Berrino F, Bastiaannet E, Gavin A, Galceran J, et al. Predictions of survival up to 10 years after diagnosis for European women with breast cancer in 2000–2002. Int J Cancer. 2013;132(10):2404–12.
Ross JS, Fletcher JA. The HER-2/neu oncogene in breast cancer: prognostic factor, predictive factor, and target for therapy. Stem Cells. 1998;16(6):413–28.
Pauletti G, Dandekar S, Rong H, et al. Assessment of methods for tissue-based detection of the HER-2/neu alteration in human breast cancer: a direct comparison of fluorescence in situ hybridization and immunohistochemistry. J Clin Oncol. 2000;18(21):3651–64.
Menard S, Fortis S, Castiglioni F, Agresti R, Balsari A. HER2 as a prognostic factor in breast cancer. Oncology. 2001;61(Suppl 2):67–72.
Curigliano G, Viale G, Bagnardi V, et al. Clinical relevance of HER2 overexpression/amplification in patients with small tumor size and node-negative breast cancer. J Clin Oncol. 2009;27(34):5693–9.
Brown M, Tsodikov A, Bauer KR, Parise CA, Caggiano V. The role of human epidermal growth factor receptor 2 in the survival of women with estrogen and progesterone receptor-negative, invasive breast cancer: the California Cancer Registry, 1999–2004. Cancer. 2008;112(4):737–47.
Borg A, Tandon AK, Sigurdsson H, et al. HER-2/neu amplification predicts poor survival in node-positive breast cancer. Cancer Res. 1990;50(14):4332–7.
Ross JS, Slodkowska EA, Symmans WF, Pusztai L, Ravdin PM, Hortobagyi GN. The HER-2 receptor and breast cancer: ten years of targeted anti-HER-2 therapy and personalized medicine. Oncologist. 2009;14(4):320–68.
National Institute for Health and Clinical Excellence (NICE). Guidance on the use of trastuzumab for the treatment of advanced breast cancer. NICE Technology Appraisal Guidance. No. 34. 2002. http://www.nice.org.uk/nicemedia/pdf/advancedbreastcancerno34pdf.pdf. Accessed 11 Dec 2013.
National Institute for Health and Care Excellence). Advanced breast cancer: diagnosis and treatment: NICE clinical guideline 81. 2009. http://www.nice.org.uk/Guidance/CG81. Accessed 14 May 2013.
Marty M, Cognetti F, Maraninchi D, et al. Randomized phase II trial of the efficacy and safety of trastuzumab combined with docetaxel in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer administered as first-line treatment: the M77001 study group. J Clin Oncol. 2005;23(19):4265–74.
European Medicines Agency. Perjeta (Pertuzumab). http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002547/human_med_001628.jsp&mid=WC0b01ac058001d124. Accessed 6 Sept 2013.
Fleeman N, Bagust A, Beale S, et al. Pertuzumab in combination with trastuzumab and docetaxel for the treatment of HER2 positive metastatic or locally recurrent unresectable breast cancer: a single technology appraisal. Liverpool: LRiG; 2013. http://www.nets.nihr.ac.uk/__data/assets/pdf_file/0007/82636/ERGReport-11-139-01.pdf. Accessed 11 Dec 2013.
Baselga J, Cortes J, Kim SB, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366(2):109–19.
Swain SM, Kim S-B, Cortés J, et al. Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA study): overall survival results from a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 2013;14(6):461–71.
F. Hoffman-La Roche. Clinical study report—WO20698C/TOC4129g—A phase III, randomized, double-blind, placebo-controlled clinical trial to evaluate the efficacy and safety of pertuzumab + trastuzumab + docetaxel vs. placebo + trastuzumab + docetaxel in previously untreated HER2-positive metastatic breast cancer—Report No. 1046288: F. Hoffman-La Roche 2011.
F. Hoffman-La Roche. Update clinical study report—WO20698C/TOC4129g—A phase III, randomized, double-blind, placebo-controlled clinical trial to evaluate the efficacy and safety of pertuzumab + trastuzumab + docetaxel vs. placebo + trastuzumab + docetaxel in previously untreated HER2-positive metastatic breast cancer—Report No. 1053649: F. Hoffman-La Roche 2012.
European Medicines Agency Committee for Medicinal Products for Human Use. Assessment Report for Perjeta (pertuzumab). Procedure No.EMEA/H/C/002547/0000. 2012; Available from: http://www.emea.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002547/WC500141004.pdf. Accessed 29 Apr 2013.
Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
Sparano JA, Wang M, Martino S, et al. Weekly paclitaxel in the adjuvant treatment of breast cancer. N Engl J Med. 2008;358(16):1663–71.
Baselga J, Gelmon KA, Verma S, et al. Phase II trial of pertuzumab and trastuzumab in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer that progressed during prior trastuzumab therapy. J Clin Oncol. 2010;28(7):1138–44.
Glenny AM, Altman DG, Song F, et al. Indirect comparisons of competing interventions. Health Technol Assess. 2005;9(26):1–134 (iii–iv).
Munich Cancer Registry. Tumorregister Müechen. 2012. http://translate.google.co.uk/translate?hl=en&sl=de&u=http://www.tumorregister-muenchen.de/facts/specific_analysis.php&prev=/search%3Fq%3DTumorregiste-Muenchen,%2B2012%26biw%3D1920%26bih%3D1054. Accessed 7 June 2013.
Joint Formulary Committee. British National Formulary (BNF) March 2012. London: British Medical Association and Royal Pharmaceutical Society of Great Britain; 2012.
Department of Health. NHS Reference costs: financial year 2011 to 2012. London: Department of Health; 2012. https://www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012. Accessed 7 June 2013.
Millar D, Corrie P, Hill M, Pulfer A. PCN74 A service evaluation to compare secondary care resource use between Xelox and Folfox-6 regimens in the treatment of metastatic colorectal cancer (MCRC) from a UK National Health Service (NHS) perspective. Value Health. 2008;11:A483.
Personal Social Services Research Unit (PSSRU). Unit costs of health and social care 2012. Canterbury, Kent; 2012. http://www.pssru.ac.uk/project-pages/unit-costs/2012/. Accessed 7 June 2013.
Guest J, Ruiz F, Greener M, Trotman I. Palliative care treatment patterns and associated costs of healthcare resource use for specific advanced cancer patients in the UK. Eur J Cancer Care. 2006;15(1):65–73.
National Institute for Health and Clinical Excellence. Bevacizumab in combination with capecitabine for the first-line treatment of metastatic breast cancer (TA263). London 2012. http://guidance.nice.org.uk/TA263. Accessed 7 June 2013.
Lloyd A, Nafees B, Narewska J, Dewilde S, Watkins J. Health state utilities for metastatic breast cancer. Br J Cancer. 2006;95(6):683–90.
Kaufman B, Mackey JR, Clemens MR, et al. Trastuzumab plus anastrozole versus anastrozole alone for the treatment of postmenopausal women with human epidermal growth factor receptor 2-positive, hormone receptor-positive metastatic breast cancer: results from the randomized phase III TAnDEM study. J Clin Oncol. 2009;27(33):5529–37.
Acknowledgments
This project was funded by the National Institute for Health Research Health Technology Assessment Programme (project number 11/139/01). See the Health Technology Assessment programme website for further project information. http://www.hta.ac.uk.
The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the National Institute for Health and Care Excellence or the Department of Health.
The authors have no competing interests.
Contributions of authors
Nigel Fleeman: Project lead, drafted clinical results section and supervised the final report. Adrian Bagust: Critical appraisal of the economic model. Sophie Beale: Critical appraisal of the economic evidence. Kerry Dwan: Critical appraisal of clinical statistical approach. Rumona Dickson: Summary and critical appraisal of the clinical evidence. Chris Proudlove: Critical appraisal of the manufacturer’s submission. Yenal Dundar: Cross-checking of manufacturer’s search strategies.
Author information
Authors and Affiliations
Corresponding author
Additional information
A NICE Single Technology Appraisal.
Rights and permissions
About this article
Cite this article
Fleeman, N., Bagust, A., Beale, S. et al. Pertuzumab in Combination with Trastuzumab and Docetaxel for the Treatment of HER2-Positive Metastatic or Locally Recurrent Unresectable Breast Cancer. PharmacoEconomics 33, 13–23 (2015). https://doi.org/10.1007/s40273-014-0206-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-014-0206-2