Abstract
Background
Generalized anxiety disorder (GAD) is one of the most prevalent anxiety disorders, with important implications for patients and healthcare resources. However, few economic evaluations of pharmacological treatments for GAD have been published to date, and those available have assessed only a limited number of drugs.
Objective
To assess the cost effectiveness of pharmacological interventions for patients with GAD in the UK.
Methods
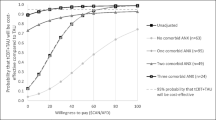
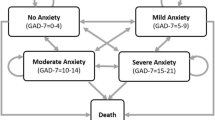
A decision-analytic model in the form of a decision tree was constructed to compare the costs and QALYs of six drugs used as first-line pharmacological treatments in people with GAD (duloxetine, escitalopram, paroxetine, pregabalin, sertraline and venlafaxine extended release [XL]) and ‘no pharmacological treatment’. The analysis adopted the perspective of the NHS and Personal Social Services (PSS) in the UK. Efficacy data were derived from a systematic literature review of double-blind, randomized controlled trials and were synthesized using network meta-analytic techniques. Two network meta-analyses were undertaken to assess the comparative efficacy (expressed by response rates) and tolerability (expressed by rates of discontinuation due to intolerable side effects) of the six drugs and no treatment in the study population. Cost data were derived from published literature and national sources, supplemented by expert opinion. The price year was 2011. Probabilistic sensitivity analysis was conducted to evaluate the underlying uncertainty of the model input parameters.
Results
Sertraline was the best drug in limiting discontinuation due to side effects and the second best drug in achieving response in patients not discontinuing treatment due to side effects. It also resulted in the lowest costs and highest number of QALYs among all treatment options assessed. Its probability of being the most cost-effective drug reached 75 % at a willingness-to-pay threshold of £20,000 per extra QALY gained.
Conclusion
Sertraline appears to be the most cost-effective drug in the treatment of patients with GAD. However, this finding is based on limited evidence for sertraline (two published trials). Sertraline is not licensed for the treatment of GAD in the UK, but is commonly used by primary care practitioners for the treatment of depression and mixed depression and anxiety.





Similar content being viewed by others
References
Lieb R, Becker E, Altamura C. The epidemiology of generalized anxiety disorder in Europe. Eur Neuropsychopharmacol. 2005;15(4):445–52.
Kessler RC, Brandenburg N, Lane M, et al. Rethinking the duration requirement for generalized anxiety disorder: evidence from the National Comorbidity Survey Replication. Psychol Med. 2005;35(7):1073–82.
Grant BF, Hasin DS, Stinson FS, et al. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2005;35(12):1747–59.
Gelder M, Harrison P, Cowen P. Shorter Oxford textbook of psychiatry. London: Oxford University Press; 2006.
Carter RM, Wittchen HU, Pfister H, et al. One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample. Depress Anxiety. 2001;13(2):78–88.
Hunt C, Issakidis C, Andrews G. DSM-IV generalized anxiety disorder in the Australian National Survey of Mental Health and Well-Being. Psychol Med. 2002;32(4):649–59.
Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depress Anxiety. 2002;16(4):162–71.
Hoffman DL, Dukes EM, Wittchen HU. Human and economic burden of generalized anxiety disorder. Depress Anxiety. 2008;25(1):72–90.
Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999;60(7):427–35.
Andlin-Sobocki P, Jonsson B, Wittchen HU, et al. Cost of disorders of the brain in Europe. Eur J Neurol. 2005;12(1 Suppl.):1–27.
Gorman JM. Treatment of generalized anxiety disorder. J Clin Psychiatry. 2002;63(8 Suppl.):17–23.
British Medical Association and The Royal Pharmaceutical Society of Great Britain. British National Formulary (BNF) 63. London: Pharmaceutical Press; 2012.
Heuzenroeder L, Donnelly M, Haby MM, et al. Cost-effectiveness of psychological and pharmacological interventions for generalized anxiety disorder and panic disorder. Aust N Z J Psychiatry. 2004;38(8):602–12.
Iskedjian M, Walker JH, Bereza BG, et al. Cost-effectiveness of escitalopram for generalized anxiety disorder in Canada. Curr Med Res Opin. 2008;24(5):1539–48.
Jorgensen TR, Stein DJ, Despiegel N, et al. Cost-effectiveness analysis of escitalopram compared with paroxetine in treatment of generalized anxiety disorder in the United Kingdom. Ann Pharmacother. 2006;40(10):1752–8.
Guest JF, Russ J, Lenox-Smith A. Cost-effectiveness of venlafaxine XL compared with diazepam in the treatment of generalised anxiety disorder in the United Kingdom. Eur J Health Econ. 2005;6(2):136–45.
Vera-Llonch M, Dukes E, Rejas J, et al. Cost-effectiveness of pregabalin versus venlafaxine in the treatment of generalized anxiety disorder: findings from a Spanish perspective. Eur J Health Econ. 2010;11(1):35–44.
The NHS Information Centre, Prescribing Support Unit. Prescription cost analysis England 2010. London: The NHS Health and Social Care Information Centre; 2011.
National Collaborating Centre for Mental Health. Generalised anxiety disorder in adults: management in primary, secondary and community care. London: The British Psychological Society and The Royal College of Psychiatrists; 2011.
Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;331(7521):897–900.
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23(20):3105–24.
McManus S, Meltzer H, Brugha T, et al. Adult psychiatric morbidity in England, 2007: results of a household survey. Leeds: The NHS Health and Social Care Information Centre; 2009.
Lunn DJ, Thomas A, Best N, et al. WinBUGS—Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput. 2000;10:325–37.
Spiegelhalter DJ, Thomas A, Best NG, Lunn D. WinBUGS user manual: version 1.4. Cambridge: MRC Biostatistics Unit; 2003.
Ades AE, Mavranezouli I, Dias S, et al. Network meta-analysis with competing risk outcomes. Value Health. 2010;13(8):976–83.
Allgulander C, Hackett D, Salinas E. Venlafaxine extended release (ER) in the treatment of generalised anxiety disorder: twenty-four-week placebo-controlled dose-ranging study. Br J Psychiatry. 2001;179:15–22.
Gelenberg AJ, Lydiard RB, Rudolph RL, et al. Efficacy of venlafaxine extended-release capsules in nondepressed outpatients with generalized anxiety disorder: a 6-month randomized controlled trial. JAMA. 2000;283(23):3082–8.
Rickels K, Pollack MH, Sheehan DV, et al. Efficacy of extended-release venlafaxine in nondepressed outpatients with generalized anxiety disorder. Am J Psychiatry. 2000;157(6):968–74.
Kasper S, Herman B, Nivoli G, et al. Efficacy of pregabalin and venlafaxine-XR in generalized anxiety disorder: results of a double-blind, placebo-controlled 8-week trial. Int Clin Psychopharmacol. 2009;24(2):87–96.
Montgomery SA, Tobias K, Zornberg GL, et al. Efficacy and safety of pregabalin in the treatment of generalized anxiety disorder: a 6-week, multicenter, randomized, double-blind, placebo-controlled comparison of pregabalin and venlafaxine. J Clin Psychiatry. 2006;67(5):771–82.
Hartford J, Kornstein S, Liebowitz M, et al. Duloxetine as an SNRI treatment for generalized anxiety disorder: results from a placebo and active-controlled trial. Int Clin Psychopharmacol. 2007;22(3):167–74.
Nicolini H, Bakish D, Duenas H, et al. Improvement of psychic and somatic symptoms in adult patients with generalized anxiety disorder: examination from a duloxetine, venlafaxine extended-release and placebo-controlled trial. Psychol Med. 2009;39(2):267–76.
Bose A, Korotzer A, Gommoll C, et al. Randomized placebo-controlled trial of escitalopram and venlafaxine XR in the treatment of generalized anxiety disorder. Depress Anxiety. 2008;25(10):854–61.
Hackett D, Haudiquet V, Salinas E. A method for controlling for a high placebo response rate in a comparison of venlafaxine XR and diazepam in the short-term treatment of patients with generalised anxiety disorder. Eur Psychiatry. 2003;18(4):182–7.
Davidson JR, DuPont RL, Hedges D, et al. Efficacy, safety, and tolerability of venlafaxine extended release and buspirone in outpatients with generalized anxiety disorder. J Clin Psychiatry. 1999;60(8):528–35.
Montgomery S, Chatamra K, Pauer L, et al. Efficacy and safety of pregabalin in elderly people with generalised anxiety disorder. Br J Psychiatry. 2008;193(5):389–94.
Rickels K, Pollack MH, Feltner DE, et al. Pregabalin for treatment of generalized anxiety disorder: a 4-week, multicenter, double-blind, placebo-controlled trial of pregabalin and alprazolam. Arch Gen Psychiatry. 2005;62(9):1022–30.
Pohl RB, Feltner DE, Fieve RR, et al. Efficacy of pregabalin in the treatment of generalized anxiety disorder: double-blind, placebo-controlled comparison of BID versus TID dosing. J Clin Psychopharmacol. 2005;25(2):151–8.
Pande AC, Crockatt JG, Feltner DE, et al. Pregabalin in generalized anxiety disorder: a placebo-controlled trial. Am J Psychiatry. 2003;160(3):533–40.
European Medicines Agency. European assessment report: LYRICA. London: EMEA; 2006. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Scientific_Discussion_-_Variation/human/000546/WC500046605.pdf. Accessed 27 Oct 2011.
Feltner DE, Crockatt JG, Dubovsky SJ, et al. A randomized, double-blind, placebo-controlled, fixed-dose, multicenter study of pregabalin in patients with generalized anxiety disorder. J Clin Psychopharmacol. 2003;23(3):240–9.
Koponen H, Allgulander C, Erickson J, et al. Efficacy of duloxetine for the treatment of generalized anxiety disorder: implications for primary care physicians. Prim Care Companion J Clin Psychiatry. 2007;9(2):100–7.
Rynn M, Russell J, Erickson J, et al. Efficacy and safety of duloxetine in the treatment of generalized anxiety disorder: a flexible-dose, progressive-titration, placebo-controlled trial. Depress Anxiety. 2008;25(3):182–9.
Wu WY, Wang G, Ball SG, et al. Duloxetine versus placebo in the treatment of patients with generalized anxiety disorder in China. Chin Med J (Engl). 2011;124(20):3260–8.
Davidson JR, Bose A, Korotzer A, et al. Escitalopram in the treatment of generalized anxiety disorder: double-blind, placebo controlled, flexible-dose study. Depress Anxiety. 2004;19(4):234–40.
Lenze EJ, Rollman BL, Shear MK, et al. Escitalopram for older adults with generalized anxiety disorder: a randomized controlled trial. JAMA. 2009;301(3):295–303.
Baldwin DS, Huusom AK, Maehlum E. Escitalopram and paroxetine in the treatment of generalised anxiety disorder: randomised, placebo-controlled, double-blind study. Br J Psychiatry. 2006;189:264–72.
Merideth C, Cutler AJ, She F, et al. Efficacy and tolerability of extended release quetiapine fumarate monotherapy in the acute treatment of generalized anxiety disorder: a randomized, placebo controlled and active-controlled study. Int Clin Psychopharmacol. 2012;27(1):40–54.
Ansseau M, Olie JP, von Frenckel R, et al. Controlled comparison of the efficacy and safety of four doses of suriclone, diazepam, and placebo in generalized anxiety disorder. Psychopharmacology (Berl). 1991;104(4):439–43.
Rickels K, DeMartinis N, Aufdembrinke B. A double-blind, placebo-controlled trial of abecarnil and diazepam in the treatment of patients with generalized anxiety disorder. J Clin Psychopharmacol. 2000;20(1):12–8.
Andreatini R, Sartori VA, Seabra ML, et al. Effect of valepotriates (valerian extract) in generalized anxiety disorder: a randomized placebo-controlled pilot study. Phytother Res. 2002;16(7):650–4.
Sramek JJ, Tansman M, Suri A, et al. Efficacy of buspirone in generalized anxiety disorder with coexisting mild depressive symptoms. J Clin Psychiatry. 1996;57(7):287–91.
Pollack MH, Worthington JJ, Manfro GG, et al. Abecarnil for the treatment of generalized anxiety disorder: a placebo-controlled comparison of two dosage ranges of abecarnil and buspirone. J Clin Psychiatry. 1997;58(11 Suppl.):19–23.
Feltner DE, Harness J, Brock J, et al. Clinical evaluation of the Daily Assessment of Symptoms-Anxiety (DAS-A): a new instrument to assess the onset of symptomatic improvement in generalized anxiety disorder. CNS Neurosci Ther. 2009;15(1):12–8.
GSK. Clinical evaluation of BRL29060A (paroxetine hydrochloride hydrate) in generalized anxiety disorder (GAD): a double-blind, placebo-controlled, comparative study. India: GSK; 2005. http://www.gsk-clinicalstudyregister.com/result_detail.jsp?protocolId=BRL29060A%2f856&studyId=573BB223-06D2-4684-A2C3-D76E7488CC42&compound=Anxiety+Disorders&type=Medical+Condition&letterrange=A-F. Accessed 27 Oct 2011.
Pollack MH, Zaninelli R, Goddard A, et al. Paroxetine in the treatment of generalized anxiety disorder: results of a placebo-controlled, flexible-dosage trial. J Clin Psychiatry. 2001;62(5):350–7.
Rickels K, Zaninelli R, McCafferty J, et al. Paroxetine treatment of generalized anxiety disorder: a double-blind, placebo-controlled study. Am J Psychiatry. 2003;160(4):749–56.
GSK. A randomized, double-blind, placebo-controlled, flexible dosage trial to evaluate the efficacy and tolerability of paroxetine CR in patients with generalised anxiety disorder (GAD). India: GSK; 2002. http://www.gsk-clinicalstudyregister.com/result_detail.jsp?protocolId=29060%2f791&studyId=A32F4E7C-163F-4838-9658-B607CF41EC88&compound=Anxiety+Disorders&type=Medical+Condition&letterrange=A-F. Accessed 27 Oct 2011.
Hewett K, et al. Generalized anxiety disorder: efficacy of paroxetine. World J Biol Psychiatry. 2001;2(1 Suppl.):358e.
Bandelow B, Chouinard G, Bobes J, et al. Extended-release quetiapine fumarate (quetiapine XR): a once-daily monotherapy effective in generalized anxiety disorder. Data from a randomized, double-blind, placebo- and active-controlled study. Int J Neuropsychopharmacol. 2010;13(3):305–20.
Khan A, Joyce M, Atkinson S, et al. A randomized, double-blind study of once-daily extended release quetiapine fumarate (quetiapine XR) monotherapy in patients with generalized anxiety disorder. J Clin Psychopharmacol. 2011;31(4):418–28.
Allgulander C, Dahl AA, Austin C, et al. Efficacy of sertraline in a 12-week trial for generalized anxiety disorder. Am J Psychiatry. 2004;161(9):1642–9.
Brawman-Mintzer O, Knapp RG, Rynn M, et al. Sertraline treatment for generalized anxiety disorder: a randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2006;67(6):874–81.
Bielski RJ, Bose A, Chang CC. A double-blind comparison of escitalopram and paroxetine in the long-term treatment of generalized anxiety disorder. Ann Clin Psychiatry. 2005;17(2):65–9.
AstraZeneca Clinical Trials. A multi-center, double-blind, randomized, parallel-group, placebo-controlled phase III study of the efficacy and safety of quetiapine fumarate extended-release (Seroquel XR) as monotherapy in the treatment of elderly patients with generalized anxiety disorder (CHROMIUM study). AstraZeneca; 2008. http://www.astrazenecaclinicaltrials.com/search/?itemId=8543681. Accessed 27 Oct 2011.
Darcis T, Ferreri M, Natens J, et al. A multicentre double-blind placebo-controlled study investigating the anxiolytic efficacy of hydroxyzine in patients with generalized anxiety. Hum Psychopharmacol. 1995;10(3):181–7.
Llorca PM, Spadone C, Sol O, et al. Efficacy and safety of hydroxyzine in the treatment of generalized anxiety disorder: a 3-month double-blind study. J Clin Psychiatry. 2002;63(11):1020–7.
Allgulander C, Florea I, Huusom AK. Prevention of relapse in generalized anxiety disorder by escitalopram treatment. Int J Neuropsychopharmacol. 2006;9(5):495–505.
Davidson JR, Wittchen HU, Llorca PM, et al. Duloxetine treatment for relapse prevention in adults with generalized anxiety disorder: a double-blind placebo-controlled trial. Eur Neuropsychopharmacol. 2008;18(9):673–81.
Stocchi F, Nordera G, Jokinen RH, et al. Efficacy and tolerability of paroxetine for the long-term treatment of generalized anxiety disorder. J Clin Psychiatry. 2003;64(3):250–8.
Rickels K, Etemad B, Khalid-Khan S, et al. Time to relapse after 6 and 12 months’ treatment of generalized anxiety disorder with venlafaxine extended release. Arch Gen Psychiatry. 2010;67(12):1274–81.
Feltner D, Wittchen HU, Kavoussi R, et al. Long-term efficacy of pregabalin in generalized anxiety disorder. Int Clin Psychopharmacol. 2008;23(1):18–28.
Katzman MA, Brawman-Mintzer O, Reyes EB, et al. Extended release quetiapine fumarate (quetiapine XR) monotherapy as maintenance treatment for generalized anxiety disorder: a long-term, randomized, placebo-controlled trial. Int Clin Psychopharmacol. 2011;26(1):11–24.
Allgulander C, Jorgensen T, Wade A, et al. Health-related quality of life (HRQOL) among patients with generalised anxiety disorder: evaluation conducted alongside an escitalopram relapse prevention trial. Curr Med Res Opin. 2007;23(10):2543–9.
Revicki DA, Brandenburg N, Matza L, et al. Health-related quality of life and utilities in primary-care patients with generalized anxiety disorder. Qual Life Res. 2008;17(10):1285–94.
Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21(2):271–92.
Brambilla P, Cipriani A, Hotopf M, et al. Side-effect profile of fluoxetine in comparison with other SSRIs, tricyclic and newer antidepressants: a meta-analysis of clinical trial data. Pharmacopsychiatry. 2005;38(2):69–77.
Werneke U, Northey S, Bhugra D. Antidepressants and sexual dysfunction. Acta Psychiatr Scand. 2006;114(6):384–97.
Tassone DM, Boyce E, Guyer J, et al. Pregabalin: a novel gamma-aminobutyric acid analogue in the treatment of neuropathic pain, partial-onset seizures, and anxiety disorders. Clin Ther. 2007;29(1):26–48.
Taylor D. Antidepressant drugs and cardiovascular pathology: a clinical overview of effectiveness and safety. Acta Psychiatr Scand. 2008;118(6):434–42.
Wernicke J, Lledo A, Raskin J, et al. An evaluation of the cardiovascular safety profile of duloxetine: findings from 42 placebo-controlled studies. Drug Saf. 2007;30(5):437–55.
Stone M, Laughren T, Jones ML, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009;11(339):b2880.
Fergusson D, Doucette S, Glass KC, et al. Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials. BMJ. 2005;330(7488):396.
Yuan Y, Tsoi K, Hunt RH. Selective serotonin reuptake inhibitors and risk of upper GI bleeding: confusion or confounding? Am J Med. 2006;119(9):719–27.
Revicki DA, Wood M. Patient-assigned health state utilities for depression-related outcomes: differences by depression severity and antidepressant medications. J Affect Disord. 1998;48(1):25–36.
National Institute for Health and Clinical Excellence. The guidelines manual. London: NICE; 2009.
Curtis L. Unit costs of health and social care 2011. Canterbury: Personal Social Services Research Unit, University of Kent; 2011.
The NHS Information Centre. Hospital episode statistics 2010–11. London: The NHS Health and Social Care Information Centre; 2011.
Department of Health. NHS Reference costs 2010–11. London: Department of Health; 2011.
Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. New York: Oxford University Press; 2006.
Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ. 2001;10(8):779–87.
National Institute for Health and Clinical Excellence. Social Value Judgements. Principles for the development of NICE guidance. 2008. 2nd ed. London: National Institute for Health and Clinical Excellence; 2008.
Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6.
Baldwin D, Woods R, Lawson R, et al. Efficacy of drug treatments for generalised anxiety disorder: systematic review and meta-analysis. BMJ. 2011;342:d1199.
Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746–58.
Soares-Weiser K, Bravo VY, Beynon S, et al. A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder. Health Technol Assess 2007;11(39):iii–iv, ix–206.
Cipriani A, Barbui C, Salanti G, et al. Comparative efficacy and acceptability of antimanic drugs in acute mania: a multiple-treatments meta-analysis. Lancet. 2011;378(9799):1306–15.
Edwards SJ, Smith CJ. Tolerability of atypical antipsychotics in the treatment of adults with schizophrenia or bipolar disorder: a mixed treatment comparison of randomized controlled trials. Clin Ther. 2009;31(Pt 1):1345–59.
Silverstone PH, Salinas E. Efficacy of venlafaxine extended release in patients with major depressive disorder and comorbid generalized anxiety disorder. J Clin Psychiatry. 2001;62(7):523–9.
Barbui C, Cipriani A. Fluoxetine top of the ranking for GAD: garbage in, garbage out? [rapid response to Baldwin D, Woods R, Lawson R, et al. Efficacy of drug treatments for generalised anxiety disorder: systematic review and meta-analysis. BMJ 2011 Mar; 342: d1199]. BMJ 16; 2011. http://www.bmj.com/content/342/bmj.d1199?tab=responses. Accessed 27 Oct 2011.
Whittington CJ, Kendall T, Fonagy P, et al. Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data. Lancet. 2004;363(9418):1341–5.
Turner EH, Matthews AM, Linardatos E, et al. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008;358(3):252–60.
Acknowledgments
The economic analysis presented in this paper was undertaken to inform a clinical practice guideline on anxiety (partial update) developed by the National Collaborating Centre for Mental Health (NCCMH), commissioned and funded by NICE in the UK [19]. The authors’ work was independent of the funding body. All authors have no conflicts of interest to declare. The authors would like to thank the GDG of the anxiety guideline (partial update) for useful comments on the development of the economic model and the interpretation of the results. Special thanks to Philip Cowen (University of Oxford, UK) for expert advice on the development of the economic model and the interpretation of findings, as well as for useful comments on previous drafts of the manuscript. We also acknowledge Sarah Stockton (NCCMH) for creating the search strategies and conducting the database searches used for the anxiety guideline as well as the updated searches used in this study.
Author contributions
IM, NM and TK were paid by the NCCMH to undertake the development of the partial update of the anxiety guideline. JC was chair of the GDG. IM conceived and developed the economic model, undertook the network meta-analyses and drafted the manuscript. NM conducted the systematic review of clinical literature. JC and TK served as clinical experts for the development of the economic model. All authors contributed to the interpretation of the results. NM, JC and TK critically reviewed the manuscript. All authors approved the final version submitted for publication. IM is the guarantor of the study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mavranezouli, I., Meader, N., Cape, J. et al. The Cost Effectiveness of Pharmacological Treatments for Generalized Anxiety Disorder. PharmacoEconomics 31, 317–333 (2013). https://doi.org/10.1007/s40273-013-0031-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-013-0031-z