Abstract
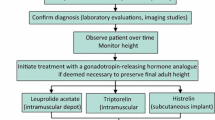
Central precocious puberty (CPP) is characterized by the same biochemical and physical features as normally timed puberty but occurs at an abnormally early age. Most cases of CPP are seen in girls, in whom it is usually idiopathic. In contrast, ~50 % of boys with CPP have an identifiable cause. The diagnosis of CPP relies on clinical, biochemical, and radiographic features. Untreated, CPP has the potential to result in early epiphyseal fusion and a significant compromise in adult height. Thus, the main goal of therapy is preservation of height potential. The gold-standard treatment for CPP is gonadotropin-releasing hormone (GnRH) analogs (GnRHa). Numerous preparations with a range of delivery systems and durations of action are commercially available. While the outcomes of patients treated for CPP have generally been favorable, more research about the psychological aspects, optimal monitoring, and long-term effects of all forms of GnRHa treatment is needed. Several potential therapeutic alternatives to GnRHa exist and await additional investigation.
Similar content being viewed by others
References
Nebesio TD, Eugster EA. Current concepts in normal and abnormal puberty. Curr Probl Pediatr Adolesc Health Care. 2007;37(2):50–72. doi:10.1016/j.cppeds.2006.10.005.
Fuqua JS. Treatment and outcomes of precocious puberty: an update. J Clin Endocrinol Metab. 2013;98(6):2198–207. doi:10.1210/jc.2013-1024.
Tanner JM, Davies PSW. Clinical longitudinal standards for height and height velocity for North American children. J Pediatr. 1985;107(3):317–29. doi:10.1016/s0022-3476(85)80501-1.
Soriano-Guillen L, Corripio R, Labarta JI, Canete R, Castro-Feijoo L, Espino R, et al. Central precocious puberty in children living in Spain: incidence, prevalence, and influence of adoption and immigration. J Clin Endocrinol Metab. 2010;95(9):4305–13. doi:10.1210/jc.2010-1025.
Lee PA, Neely EK, Fuqua J, Yang D, Larsen LM, Mattia-Goldberg C, et al. Efficacy of leuprolide acetate 1-month depot for central precocious puberty (CPP): growth outcomes during a prospective, longitudinal study. Int J Pediatr Endocrinol. 2011;2011(1):7. doi:10.1186/1687-9856-2011-7.
Choi KH, Chung SJ, Kang MJ, Yoon JY, Lee JE, Lee YA, et al. Boys with precocious or early puberty: incidence of pathological brain magnetic resonance imaging findings and factors related to newly developed brain lesions. Ann Pediatr Endocrinol Metab. 2013;18(4):183–90. doi:10.6065/apem.2013.18.4.183.
de Vries L, Kauschansky A, Shohat M, Phillip M. Familial central precocious puberty suggests autosomal dominant inheritance. J Clin Endocrinol Metab. 2004;89(4):1794–800. doi:10.1210/jc.2003-030361.
Rohn R, Rousonelos G. Familial sexual precocity. Am J Dis Child. 1986;140(8):741–2. doi:10.1001/archpedi.1986.02140220023017.
Teles MG, Bianco SD, Brito VN, Trarbach EB, Kuohung W, Xu S, et al. A GPR54-activating mutation in a patient with central precocious puberty. N Engl J Med. 2008;358(7):709–15. doi:10.1056/NEJMoa073443.
Luan X, Yu H, Wei X, Zhou Y, Wang W, Li P, et al. GPR54 polymorphisms in Chinese girls with central precocious puberty. Neuroendocrinology. 2007;86(2):77–83. doi:10.1159/000107511.
Silveira LG, Noel SD, Silveira-Neto AP, Abreu AP, Brito VN, Santos MG, et al. Mutations of the KISS1 gene in disorders of puberty. J Clin Endocrinol Metab. 2010;95(5):2276–80. doi:10.1210/jc.2009-2421.
Abreu AP, Dauber A, Macedo DB, Noel SD, Brito VN, Gill JC, et al. Central precocious puberty caused by mutations in the imprinted gene MKRN3. N Engl J Med. 2013;368(26):2467–75. doi:10.1056/NEJMoa1302160.
Macedo DB, Abreu AP, Reis AC, Montenegro LR, Dauber A, Beneduzzi D, et al. Central precocious puberty that appears to be sporadic caused by paternally inherited mutations in the imprinted gene makorin ring finger 3. J Clin Endocrinol Metab. 2014;99(6):E1097–103. doi:10.1210/jc.2013-3126.
Settas N, Dacou-Voutetakis C, Karantza M, Kanaka-Gantenbein C, Chrousos GP, Voutetakis A. Central precocious puberty in a girl and early puberty in her brother caused by a novel mutation in the MKRN3 gene. J Clin Endocrinol Metab. 2014;99(4):E647–51. doi:10.1210/jc.2013-4084.
Zhao Y, Chen T, Zhou Y, Li K, Xiao J. An association study between the genetic polymorphisms within GnRHI, LHbeta and FSHbeta genes and central precocious puberty in Chinese girls. Neurosci Lett. 2010;486(3):188–92. doi:10.1016/j.neulet.2010.09.049.
Freitas KC, Ryan G, Brito VN, Tao YX, Costa EM, Mendonca BB, et al. Molecular analysis of the neuropeptide Y1 receptor gene in human idiopathic gonadotropin-dependent precocious puberty and isolated hypogonadotropic hypogonadism. Fertil Steril. 2007;87(3):627–34. doi:10.1016/j.fertnstert.2006.07.1519.
Parent AS, Matagne V, Westphal M, Heger S, Ojeda S, Jung H. Gene expression profiling of hypothalamic hamartomas: a search for genes associated with central precocious puberty. Horm Res. 2008;69(2):114–23. doi:10.1159/000111815.
Park SW, Lee ST, Sohn YB, Cho SY, Kim SH, Kim SJ, et al. LIN28B polymorphisms are associated with central precocious puberty and early puberty in girls. Korean J Pediatr. 2012;55(10):388–92. doi:10.3345/kjp.2012.55.10.388.
Silveira-Neto AP, Leal LF, Emerman AB, Henderson KD, Piskounova E, Henderson BE, et al. Absence of functional LIN28B mutations in a large cohort of patients with idiopathic central precocious puberty. Horm Res Paediatr. 2012;78(3):144–50. doi:10.1159/000342212.
Carel JC, Eugster EA, Rogol A, Ghizzoni L, Palmert MR, Group E-LGACC, et al. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics. 2009;123(4):e752–62. doi:10.1542/peds.2008-1783.
Eksioglu AS, Yilmaz S, Cetinkaya S, Cinar G, Yildiz YT, Aycan Z. Value of pelvic sonography in the diagnosis of various forms of precocious puberty in girls. J Clin Ultrasound. 2013;41(2):84–93. doi:10.1002/jcu.22004.
Badouraki M, Christoforidis A, Economou I, Dimitriadis AS, Katzos G. Evaluation of pelvic ultrasonography in the diagnosis and differentiation of various forms of sexual precocity in girls. Ultrasound Obstetr Gynecol. 2008;32(6):819–27. doi:10.1002/uog.6148.
de Vries L, Horev G, Schwartz M, Phillip M. Ultrasonographic and clinical parameters for early differentiation between precocious puberty and premature thelarche. Eur J Endocrinol. 2006;154(6):891–8. doi:10.1530/eje.1.02151.
Herter LD, Golendziner E, Flores JAM, Moretto M, Di Domenico K, Becker E, et al. Ovarian and uterine findings in pelvic sonography: comparison between prepubertal girls, girls with isolated thelarche, and girls with central precocious puberty. J Ultrasound Med. 2002;21(11):1237–46.
Pienkowski C, Cartault A, Carfagna L, Ernoult P, Vial J, Lemasson F, et al. Ovarian cysts in prepubertal girls. Endocr Dev. 2012;22:101–11. doi:10.1159/000326627.
Pedicelli S, Alessio P, Scire G, Cappa M, Cianfarani S. Routine screening by brain magnetic resonance imaging is not indicated in every girl with onset of puberty between the ages of 6 and 8 years. J Clin Endocrinol Metab. 2014;99(12):4455–61. doi:10.1210/jc.2014-2702.
Ng SM. Cranial MRI scans are indicated in all girls with central precocious puberty. Arch Dis Child. 2003;88(5):414–8. doi:10.1136/adc.88.5.414.
Chalumeau M, Hadjiathanasiou CG, Ng SM, Cassio A, Mul D, Cisternino M, et al. Selecting girls with precocious puberty for brain imaging: validation of European evidence-based diagnosis rule. J Pediatr. 2003;143(4):445–50. doi:10.1067/s0022-3476(03)00328-7.
Mogensen SS, Aksglaede L, Mouritsen A, Sorensen K, Main KM, Gideon P, et al. Pathological and incidental findings on brain MRI in a single-center study of 229 consecutive girls with early or precocious puberty. PloS One. 2012;7(1):e29829. doi:10.1371/journal.pone.0029829.
Carel JC, Roger M, Ispas S, Tondu F, Lahlou N, Blumberg J, et al. Final height after long-term treatment with triptorelin slow release for central precocious puberty: importance of statural growth after interruption of treatment. French Study Group of Decapeptyl in Precocious Puberty. J Clin Endocrinol Metab. 1999;84(6):1973–8. doi:10.1210/jcem.84.6.5647.
Pasquino AM, Pucarelli I, Accardo F, Demiraj V, Segni M, Di Nardo R. Long-term observation of 87 girls with idiopathic central precocious puberty treated with gonadotropin-releasing hormone analogs: impact on adult height, body mass index, bone mineral content, and reproductive function. J Clin Endocrinol Metab. 2008;93(1):190–5. doi:10.1210/jc.2007-1216.
Lazar L, Padoa A, Phillip M. Growth pattern and final height after cessation of gonadotropin-suppressive therapy in girls with central sexual precocity. J Clin Endocrinol Metab. 2007;92(9):3483–9. doi:10.1210/jc.2007-0321.
Carel JC, Lahlou N, Roger M, Chaussain JL. Precocious puberty and statural growth. Hum Reprod Update. 2004;10(2):135–47. doi:10.1093/humupd/dmh012.
Thodberg HH. Clinical review: an automated method for determination of bone age. J Clin Endocrinol Metab. 2009;94(7):2239–44. doi:10.1210/jc.2008-2474.
Mul D, Bertelloni S, Carel JC, Saggese G, Chaussain JL, Oostdijk W. Effect of gonadotropin-releasing hormone agonist treatment in boys with central precocious puberty: final height results. Horm Res. 2002;58(1):1–7. doi:10.1159/000063209.
Walvoord EC, Mazur T. Behavioral problems and idiopathic central precocious puberty: fact or fiction? Pediatr Endocrinol Rev. 2007;4(S3):306–12.
Schoelwer MJ, Donahue KL, Bryk K, Didrick P, Berenbaum SA, Eugster EA. Psychological assessment of mothers and their daughters at the time of diagnosis of precocious puberty. Int J Pediatr Endocrinol. 2015;2015(1):5. doi:10.1186/s13633-015-0001-7.
Badaru A, Wilson DM, Bachrach LK, Fechner P, Gandrud LM, Durham E, et al. Sequential comparisons of one-month and three-month depot leuprolide regimens in central precocious puberty. J Clin Endocrinol Metab. 2006;91(5):1862–7. doi:10.1210/jc.2005-1500.
Fuld K, Chi C, Neely EK. A randomized trial of 1- and 3-month depot leuprolide doses in the treatment of central precocious puberty. J Pediatr. 2011;159(6):982–7 e1. doi:10.1016/j.jpeds.2011.05.036.
Lee PA, Klein K, Mauras N, Lev-Vaisler T, Bacher P. 36-month treatment experience of two doses of leuprolide acetate 3-month depot for children with central precocious puberty. J Clin Endocrinol Metab. 2014;99(9):3153–9. doi:10.1210/jc.2013-4471.
Miller BS, Shukla AR. Sterile abscess formation in response to two separate branded long-acting gonadotropin-releasing hormone agonists. Clin Ther. 2010;32(10):1749–51. doi:10.1016/j.clinthera.2010.09.009.
Hirsch HJ, Gillis D, Strich D, Chertin B, Farkas A, Lindenberg T, et al. The histrelin implant: a novel treatment for central precocious puberty. Pediatrics. 2005;116(6):e798–802. doi:10.1542/peds.2005-0538.
Eugster EA, Clarke W, Kletter GB, Lee PA, Neely EK, Reiter EO, et al. Efficacy and safety of histrelin subdermal implant in children with central precocious puberty: a multicenter trial. J Clin Endocrinol Metab. 2007;92(5):1697–704. doi:10.1210/jc.2006-2479.
Silverman LA, Neely EK, Kletter GB, Lewis K, Chitra S, Terleckyj O, Eugster EA. Long-term continuous suppression with once-yearly histrelin subcutaneous implants for the treatment of central precocious puberty: a final report of a phase 3 multicenter trial. J Clin Endocrinol Metab (Epub 2015 Mar 24).
Lewis KA, Goldyn AK, West KW, Eugster EA. A single histrelin implant is effective for 2 years for treatment of central precocious puberty. J Pediatr. 2013;163(4):1214–6. doi:10.1016/j.jpeds.2013.05.033.
Rahhal S, Clarke WL, Kletter GB, Lee PA, Neely EK, Reiter EO, et al. Results of a second year of therapy with the 12-month histrelin implant for the treatment of central precocious puberty. Int J Pediatr Endocrinol. 2009;2009:812517. doi:10.1155/2009/812517.
Davis JS, Alkhoury F, Burnweit C. Surgical and anesthetic considerations in histrelin capsule implantation for the treatment of precocious puberty. J Pediatr Surg. 2014;49(5):807–10. doi:10.1016/j.jpedsurg.2014.02.067.
Vottero A, Pedori S, Verna M, Pagano B, Cappa M, Loche S, et al. Final height in girls with central idiopathic precocious puberty treated with gonadotropin-releasing hormone analog and oxandrolone. J Clin Endocrinol Metab. 2006;91(4):1284–7. doi:10.1210/jc.2005-1693.
Pucarelli I, Segni M, Ortore M, Arcadi E, Pasquino AM. Effects of combined gonadotropin-releasing hormone agonist and growth hormone therapy on adult height in precocious puberty: a further contribution. J Pediatr Endocrinol Metab. 2003;16(7):1005–10.
Zhao X, Zhang Q. Clinical efficacy of letrozole in boys with idiopathic central precocious puberty. Chin J Contemp Pediatr. 2014;16(4):397–400. doi:10.7499/j.issn.1008-8830.2014.04.018.
Lewis KA, Eugster EA. Random luteinizing hormone often remains pubertal in children treated with the histrelin implant for central precocious puberty. J Pediatr. 2013;162(3):562–5. doi:10.1016/j.jpeds.2012.08.038.
Neely EK, Lee PA, Bloch CA, Larsen L, Yang D, Mattia-Goldberg C, et al. Leuprolide acetate 1-month depot for central precocious puberty: hormonal suppression and recovery. Int J Pediatr Endocrinol. 2010;2010:398639. doi:10.1155/2010/398639.
Fisher MM, Lemay D, Eugster EA. Resumption of puberty in girls and boys following removal of the histrelin implant. J Pediatr. 2014;164(4):912–6 e1. doi:10.1016/j.jpeds.2013.12.009.
Magiakou MA, Manousaki D, Papadaki M, Hadjidakis D, Levidou G, Vakaki M, et al. The efficacy and safety of gonadotropin-releasing hormone analog treatment in childhood and adolescence: a single center, long-term follow-up study. J Clin Endocrinol Metab. 2010;95(1):109–17. doi:10.1210/jc.2009-0793.
Poomthavorn P, Suphasit R, Mahachoklertwattana P. Adult height, body mass index and time of menarche of girls with idiopathic central precocious puberty after gonadotropin-releasing hormone analogue treatment. Gynecol Endocrinol. 2011;27(8):524–8. doi:10.3109/09513590.2010.507289.
Franceschi R, Gaudino R, Marcolongo A, Gallo MC, Rossi L, Antoniazzi F, et al. Prevalence of polycystic ovary syndrome in young women who had idiopathic central precocious puberty. Fertil Steril. 2010;93(4):1185–91. doi:10.1016/j.fertnstert.2008.11.016.
Dajani T, Reiner B, Salem G, Shea H, Rappaport M, Alzohaili O, Van Meter Q, Domek D, Bethin K, Kaplowitz P, Klein K, Merritt D, Rose S, Kletter G, Aisenberg J, Brenner D, Rogers D, Silverman L, Lee P, Gomez R, Cassorla F, Yang J, Eugster E, Flores O, Wright N. Efficacy, safety, and pharmacokinetics (PK) of triptorelin 6-month formulation in patients with central precocious puberty. In: ClinicalTrials.gov [Internet]. National Library of Medicine (US), Bethesda (MD). 2014. https://clinicaltrials.gov/ct2/show/NCT01467882.
Pinilla L, Aguilar E, Dieguez C, Millar RP, Tena-Sempere M. Kisspeptins and reproduction: physiological roles and regulatory mechanisms. Physiol Rev. 2012;92(3):1235–316. doi:10.1152/physrev.00037.2010.
Hirsch HJ, Lahlou N, Gillis D, Strich D, Rosenberg-Hagen B, Chertin B, et al. Free alpha-subunit is the most sensitive marker of gonadotropin recovery after treatment of central precocious puberty with the histrelin implant. J Clin Endocrinol Metab. 2010;95(6):2841–4. doi:10.1210/jc.2009-2078.
Acknowledgments
None.
Conflict of interest
Dr. Chen has no conflicts of interest to disclose. Dr. Eugster participates in clinical trials investigating treatment of CPP, funded by Endo Pharmaceuticals. No sources of funding were used to support the writing of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, M., Eugster, E.A. Central Precocious Puberty: Update on Diagnosis and Treatment. Pediatr Drugs 17, 273–281 (2015). https://doi.org/10.1007/s40272-015-0130-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-015-0130-8