Abstract
Background and Objectives
Characterized by sudden onset of severe joint pain, swelling, redness, and tenderness to touch, gout ‘flare ups’ have a substantial impact on quality of life (QoL). This research employed a patient-centered approach to explore the symptoms and impacts of gout, and assess the content validity of existing patient-reported outcomes (PROs).
Methods
Qualitative interviews were conducted with 30 US gout patients (non-tophaceous: n = 20, tophaceous: n = 10) and five expert rheumatologists. Each interview included both concept elicitation (CE) questioning to learn about the patient experience and cognitive debriefing to assess the content validity of three PRO instruments (HAQ-DI, GAQ, and TIQ-20). Nine of the patients provided further real-time qualitative data through a smart phone application. All qualitative data were subject to thematic analysis using Atlas.ti. Two patient advisors and three expert clinicians were engaged as advisors at key stages throughout the research.
Results
Interview and real-time data identified the same core symptoms and proximal impact concepts. Severe pain (typically in joints of extremities) was described as the cardinal symptom, often accompanied by swelling, redness, heat, sensitivity to touch, and stiffness. Domains of QoL impacted included physical functioning, sleep, daily activities, and work. The PRO instruments were generally well-understood by patients, but each included items with questionable relevance to at least some of the sample, dependent on the specific joints affected.
Conclusions
Gout patients experience severe pain in affected joints, resulting in substantial limitations in physical functioning. Both the HAQ-DI and the TIQ-20 are useful for specific research purposes in the gout population, although modifications are recommended.
Similar content being viewed by others
A conceptual model was developed, based on qualitative data, detailing the patient experience of gout. A conceptual model can be critical in informing the selection of optimal outcome assessments for research studies and general clinical practice. |
Pain was identified as being the cardinal, defining symptom of gout, leading to a range of impacts on health-related quality of life (HRQoL), most notably physical functioning and sleep. |
The HAQ-DI, the ‘overall concern’ GAQ domain, and the TIQ-20 demonstrated some value for the assessment of symptoms, impacts, and limitations in gout, which highlights that there could be benefit from developing a new measure specific to gout. |
1 Background
Gout is among the most common inflammatory rheumatic diseases of adulthood, affecting approximately 1–2 % of adults in Western Europe [1] and 3.9 % of adults in the USA [2]. With a higher incidence in men than women (3:1) [2], the prevalence of gout is also rapidly increasing, with an increase of 4 % per year reported in the UK alone [3]. Gout results from elevated or excess serum uric acid (SUA) levels in the body [4], leading to the formation and deposition of monosodium urate (MSU) crystals in the synovial fluid and lining of joints and soft tissue [5, 6]. Shedding of crystals into the synovial fluid of a peripheral joint (typically the first metatarsophalangeal joint, or ‘big toe’) typically triggers the first episode or ‘flare’ [7]. Other commonly affected joints include the mid-tarsal joints, ankles, knees, fingers, wrists, and elbows [5].
Flares are characterized by sudden onset of severe pain, swelling, erythema, and tenderness to touch in the joint [8]. Without treatment, or through poor clinical management, chronic tophaceous gout can develop, characterized by chronic pain and stiffness, joint damage, and visibly evident subcutaneous nodular deposits of MSU crystals (tophi) [5]. Only 10 % of the overall gout patient population are currently estimated to progress to chronic tophaceous gout [9].
While there is evidence that the symptoms experienced during flares can substantially impact the health-related quality of life of patients with gout [8], qualitative research documenting the patient experience in depth is limited [10, 11]. Gout has been reported to impact on mobility (especially walking and climbing stairs), activities of daily living (such as gardening and doing housework), emotional functioning, sleep, and diet [12, 13], as well as work productivity [10, 14]. A number of studies have demonstrated that individuals with gout have lower physical functioning than normative populations and study controls [8]. However, those existing studies are limited by the use of mostly generic instruments to measure HRQoL, which arguably lack the sensitivity to capture the full impact of the condition, particularly in those with less severe gout [8].
Qualitative research can help provide a better understanding of the patient experience and overall health burden of gout. Furthermore, the subsequent development of a conceptual model detailing the experience from the patient perspective could provide a starting point to aid selection of appropriate clinical study endpoints or guide the development of a new disease-specific measure. The ability to effectively measure HRQoL is crucial for evaluating the effects of the disease and treatment, as well as helping to better understand the best approach to managing gout [15].
OMERACT (Outcome Measures in Rheumatology Clinical Trials) recently published a report summarizing the appropriateness of patient-reported outcomes (PROs) in measuring impacts of chronic gout [16], based on assessments of the OMERACT filters of truth (face, content, construct and criterion validity), discrimination (reliability, responsiveness), and feasibility (how easily the measure can be applied given constraints of time, money, and interpretability) [16]. Based on these criteria, OMERACT endorsed the Health Assessment Questionnaire-Disability Index (HAQ-DI) for use in assessing the physical impacts of chronic gout [17]. Conversely, a gout-specific QoL measure (Gout Assessment Questionnaire [GAQ]-v2.0) [18] was not deemed appropriate because of several concerns, including low internal consistency and construct validity [17]. Following publication of the OMERACT guidance, the Tophus Impact Questionnaire (TIQ-20) was developed using qualitative interviews to assess tophi burden; its content validity and psychometric validity have been established [19]. These existing measures are either gout-specific or have been used in gout populations. Nevertheless, it is essential to ensure all concepts that are relevant and important to patients are captured. The core domains relevant to assess in acute gout, as identified by OMERACT, include pain, joint swelling, joint tenderness, patient global assessment, and activity limitations. For chronic gout, the core domains identified are serum urate, acute gout attacks, tophus burden, HRQoL, activity limitations, pain, and patient global assessment [12].
This study aimed to gain a strong understanding of gout patients’ experiences of symptoms, flares, tophi burden, and the broader impact of gout using a patient-centred approach to inform development of a conceptual model. Supplementary to traditional patient interviews, the study employed novel digital methods to collect real-time qualitative data. Additionally, the content validity of three existing PROs in the specific context of use in gout populations was assessed in accordance with the criteria outlined in the US FDA PRO guidance [20].
Throughout, a ‘patient-centric’ approach was taken. As well as conducting patient interviews in a rigorous and ethical fashion, this also involved two patient advisors providing input and guidance as research partners rather than being interviewed as ‘subjects’ [19, 21].
2 Methods
2.1 Overview of Study Methods
This was a qualitative, non-interventional interview study involving 20 US patients with non-tophaceous gout, ten US patients with tophaceous gout, and five expert rheumatologists.
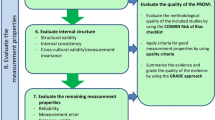
As illustrated in Fig. 1, three rounds of interviews, each with ten patients were conducted: two rounds with patients with non-tophaceous gout and a third with patients with tophaceous gout. Interim analysis was conducted between each round to allow for any potential revisions to the PROs being evaluated. Following the interviews, nine of the patients with non-tophaceous gout also took part in real-time collection of qualitative data through a smart phone application (‘app’).
Overview of study methodology for clinician and patient interviews, digital collection of real-time qualitative data, and input from patient advisors and clinical experts. CRF case report form, GAQ Gout Assessment Questionnaire, HAQ Health Assessment Questionnaire, ICF informed consent form, TIQ Tophus Impact Questionnaire
To support a patient-centered approach and gain clinical insight, two patient advisors and three of the expert rheumatologists interviewed provided input and guidance as research partners at key stages throughout the research.
2.2 Qualitative Patient Data Collection
2.2.1 Recruitment
The patients were recruited via rheumatologists and primary care physicians in Baltimore, New Orleans, and St. Louis, USA, in May/June 2014. Eligible patients had to be aged ≥18 years, literate, fluent in English, have a physician-confirmed diagnosis of gout, and a history of flares and/or tophi. Patients with tophaceous gout had to have at least one measurable tophus on the hands/wrists and/or feet/ankles measuring 5–20 mm in the longest diameter. A purposive sampling approach was taken to ensure a range of clinical and demographic characteristics.
2.2.2 Ethics
The study was approved and overseen by an Independent Review Board in the US (approval codes: ADE1-14-472, ADE2-14-168). Written informed consent was obtained prior to the collection of any data.
2.2.3 Interview Process
Interviews lasted approximately 1.5 h. Detailed interview guides were used by trained interviewers (see Supplementary Table A in the Electronic Supplementary Material [ESM] for an overview of the key questions included). The patient advisors reviewed the interview guides and provided feedback on the language used, structure, and content being covered.
The concept elicitation (CE) section of the interview used open-ended exploratory questions to facilitate spontaneous and un-biased elicitation of content regarding the patient experience of gout [22–24], followed by direct focused questions if concepts of interest had not been fully explored with patients.
The cognitive debriefing (CD) section of the interview assessed the content validity of the HAQ-DI, the GAQ ‘overall concern’ domain (patients with non-tophaceous gout only) and TIQ-20 (tophaceous gout only). A ‘think aloud’ approach [25, 26] was employed where patients shared their thoughts and reasoning for selecting each response. Patients were asked about their understanding of instructions and item wording, the relevance of concepts captured, and the appropriateness of response options and recall periods. All interviews were audio-recorded and transcribed verbatim, and identifiable information was removed.
2.2.4 Instruments
The HAQ-DI is a 20-item measure used in a range of pain conditions [27, 28] to assess eight categories of physical functioning: dressing, rising, eating, walking, hygiene, reach, grip, and usual activities [29, 30]. All items employ a response scale from zero (‘without any difficulty’) to three (‘unable to do’). The HAQ-visual analog scale (HAQ-VAS) is an anchored horizontal VAS scored from 0 (no pain) to 100 (severe pain) assessing severity of arthritis-related pain [29, 30].
The GAQ ‘overall concern’ domain consists of 13 items assessing the emotional impacts of gout [18, 31]. Although OMERACT did not endorse the GAQ, the research team felt the emotional impacts captured in the ‘overall concern’ domain were relevant and warranted exploration [17].
The TIQ-20 is a 20-item questionnaire assessing tophi burden, developed and validated in a tophaceous gout population; initial results demonstrated promising face and construct validity, reproducibility, and feasibility [19]. The TIQ-20, being specific to patients with tophi, was only tested in the third round.
2.2.5 Digital Collection of Real-Time Qualitative Data (RTQD)
Following interviews, half of the non-tophaceous gout sample (n = 9) consented to also take part in additional digital collection of real-time qualitative data (RTQD). Logistical challenges meant RTQD were not collected in the tophaceous gout sample; this is acknowledged as a limitation. This method enhances ecological validity by capturing data as patients go about their daily lives and at the exact point where a symptom or impact is experienced, in contrast with traditional interviews, where patients are required to recall previous experiences in a formal setting [20]. Given the nature of gout, whereby patients experience fluctuations in the onset, frequency, and duration of signs/symptoms (i.e. flares), this novel methodology allowed patients to report on their experiences as and when flares occurred rather than having to recall their experiences of previous flares during a later interview. Data collected through this medium arguably have stronger ecological validity than data collected from an interview.
Patients were asked to download a research app (Field Notes®) to their smart phone. Six ‘tasks’ were devised by the research team to generate insight into the patient experience based on previous literature and open-ended questions used in the patient interview guide. The tasks were sent daily to patients via the app over a 7-day period (see ESM 2). Patients responded by submitting images or self-recorded videos via the app.
2.3 Clinician Interviews
Five English-speaking rheumatologists (from the US [n = 2], the UK, New Zealand, and Spain) who specialized in treating gout were identified via clinical networks and participated in 60-min qualitative telephone interviews. Questioning focused on the patient experience of gout, symptoms/signs, and forms of treatments. Interviews were conducted using a semi-structured interview guide and were audio-recorded and transcribed verbatim.
2.4 Patient Advisors
As a patient-centered approach, two US English-speaking patients with a clinician-confirmed diagnosis of non-tophaceous gout provided input into the study design, the patient interview guide, the conceptual model, the HAQ-DI, the GAQ domain, and findings from round one of the interviews with patients with non-tophaceous gout (n = 10). The patient advisors were each engaged via teleconference calls or presentations with the research team. Ideally, both patient advisors would have been consulted in the same call to facilitate more of a group discussion; unfortunately this was not possible because of scheduling difficulties. The patients were recruited via rheumatologists and primary care physicians, and neither patient participated in the qualitative interviews. Prior to involvement, the advisors were provided with a training session on PROs and the purpose of the study to give them the confidence to contribute as collaborative active members of the research team rather than being interviewed as ‘subjects’ [19, 21].
2.5 Clinician Advisors
Three of the rheumatologists interviewed also provided guidance throughout the study by reviewing and providing key clinical insights on study documents, the conceptual model, and the full set of findings from the interviews with patients with non-tophaceous gout (n = 20). As these rheumatologists were also interviewed, they only provided input on study documents and findings related to the patient interviews, not the clinician interviews.
2.6 Qualitative Analysis of Interview Transcripts
Verbatim transcripts and video/audio recordings were subject to thematic analysis and visual analysis [25, 32, 33] using Atlas.Ti software [34]. Each transcript was assessed, and patient comments pertaining to the research questions were highlighted. A coding scheme was created and used throughout the analysis process. New codes were organically added throughout coding. Conceptual saturation (i.e., the point at which no new concepts would emerge with continued data collection [35]) was evaluated for the CE component of the interviews. Saturation was evaluated by dividing the tophaceous and non-tophaceous samples into sets of equal numbers of transcripts (tophaceous: n = 2 in each set; non-tophaceous: n = 5 in each set) and comparing the concepts that emerged from each additional set of transcripts. Saturation was considered achieved when no new concepts emerged from analysis of subsequent transcripts.
3 Results
3.1 Patient Sample Characteristics
All sampling quotas were achieved, ensuring patients with a range of demographic and clinical characteristics were recruited (Table 1). There was a higher proportion of males than females, consistent with the ratio in the wider population. Moreover, there was good representation of non-Caucasians in both the non-tophaceous (45 % Caucasian; 55 % Black/African American) and the tophaceous (30 % Caucasian; 70 % Black/African American) samples. Patients with a wide range of educational levels were included. For the RTQD collection, patients had to own a certain type of smartphone.
Mean time since diagnosis was 6.8 years in the non-tophaceous sample and 5 years in the tophaceous sample. The non-tophaceous sample had marginally higher mean SUA levels: 7.01 mg/dl compared with 6.6 mg/dl for the tophaceous sample. Over half of patients with tophaceous gout reported tophi on the ‘big toe’ (n = 70 %), with others reported in the upper extremities, including the elbow (40 %), wrist (20 %), fingers (20 %), hand (10 %), and shoulder (10 %).
3.2 Clinician Sample Characteristics
With one exception, all the expert clinicians interviewed had been treating patients for 15–25 years, with caseloads ranging from 100 to 230 patients per year, or 10–60 patients per month; one clinician was active in conducting clinical rheumatology research but had stopped treating in the prior year.
3.3 Patient Concept Elicitation (CE) Interviews
3.3.1 Flares
All patients apart from one recognized or demonstrated an understanding of the term “flare” or “flare-up”. Patients similarly defined a flare with reference to pain, swelling, and/or redness. Further detail is provided in Table 2.
The frequency of flares was reported as highly variable in both samples (ranging from monthly to yearly occurrences) and dependent on the forms of treatment taken, if any. Most patients with non-tophaceous gout (n = 12/15) described their flares lasting just a few days (dependent on promptly taking their medication, n = 4/15); in contrast, five of the six patients with tophaceous gout described their flares as lasting a week or longer.
Among patients with non-tophaceous gout, flares were most commonly reported to occur in the toe (n = 5/10), foot (n = 5/10), hands (n = 3/10), and ankles (n = 3/10). Similarly, patients with tophaceous gout commonly reported flares occurring in the feet (n = 4/7), hands (n = 3/7), elbow (n = 3/7), and knee (n = 3/7).
The majority of patients with non-tophaceous gout who talked about the onset of flares described them commonly occurring, or being more noticeable, during the night (n = 7/15), while most patients with tophaceous gout specified that flares occurred at any time of the day (n = 3/5).
All signs or symptoms experienced during flares are presented in Fig. 2. The signs and symptoms reported were broadly similar across both patient samples, although a number of symptoms were only reported by one or two of the patients with tophaceous gout, such as skin damage and stinging.
The most commonly reported symptoms were joint pain, swelling, and tenderness or sensitivity to touch. See Table 3 for a summary of symptoms reported by over 30 % of the non-tophaceous or tophaceous gout samples, with example quotes.
3.3.2 Pain
All patients spontaneously reported experiencing severe and debilitating pain during flares, most frequently describing it as a “throbbing” sensation (non-tophaceous: n = 8/20; tophaceous: n = 3/10). A number of patients spoke metaphorically, three of whom described the pain to be like a toothache: “You know how a toothache is? And it just keeps throbbing and throbbing and aching and aching. This is exactly what this feels like.” Others compared the pain to childbirth, while one patient said the pain was so severe he thought he had broken his toe.
Patients most often reported pain in the lower extremities, such as the foot (non-tophaceous: n = 12/20; tophaceous: n = 5/10), toe (non-tophaceous: n = 7/20; tophaceous: n = 4/10), and/or knee (non-tophaceous: n = 6/20, tophaceous: n = 3/10). A subset of patients described how the pain builds in the first phase of the attack and then remains constant without subsiding until the episode is over (non-tophaceous: n = 7/11; tophaceous: n = 6/6). Patients talked about the duration of their pain within a wide range of timeframes, ranging from days to weeks (non-tophaceous: n = 18/20, tophaceous: n = 7/10).
3.3.3 Swelling
In total, 25 of the 30 patients (non-tophaceous: n = 16/20; tophaceous: n = 9/10) described swelling as co-occurring with other symptoms during a flare. Two patients described the affected area swelling up to twice the normal size, while others described it becoming “puffy” (n = 2), looking “distorted”/“deformed” (n = 2) or getting a “lump” (n = 1). The swelling was reported to occur in the same joints as the pain, with duration ranging from a day to several months (non-tophaceous: n = 12/20; tophaceous: n = 7/10).
3.3.4 Tenderness or Sensitivity to Touch
In total, 16 of the 30 patients (non-tophaceous: n = 11/20; tophaceous: n = 5/10) talked about their joints feeling tender or sensitive to touch: “I just can’t stand nothing to touch it, don’t touch it.” A number of patients (non-tophaceous: n = 6/10; tophaceous: n = 3/10) spontaneously talked about the weight of a bed sheet on the affected area being too painful to bear.
3.3.5 Signs or Symptoms Between Flares
In the non-tophaceous sample, six patients reported some experience of signs or symptoms between flares, including pain in affected joints (n = 3/6), swelling (n = 2/6), tenderness (n = 1/6), and discomfort (n = 1/6). However, these symptoms were reported to be infrequent and less severe than during a flare.
3.3.6 Tophi
All patients with tophaceous gout interviewed (n = 10) discussed their tophi (or “knots”, “nodules”, “bumps”, or “lumps”), commonly located on the toe (n = 6/10) and/or elbow (n = 5/10). Symptoms directly attributed to the tophi, during or between flares, included pain (n = 7/10), soreness (n = 3/10), and throbbing (n = 3/10). Two patients described coping strategies to avoid bumping or knocking the tophi as this would cause pain. However, four others did not find their tophi bothersome. One patient talked about people looking at his tophi, or feeling the need to hide his tophi.
3.3.7 Triggers
Across both samples of patients, dietary triggers for gout symptoms were commonly discussed, particularly red meat (non-tophaceous: n = 13/20; tophaceous: n = 6/9), seafood (non-tophaceous: n = 8/20; tophaceous: n = 8/9), and alcohol (non-tophaceous: n = 6/20; tophaceous: n = 2/9). Other triggers described by patients with tophaceous gout included too much physical movement and past injury (n = 2/9, respectively).
3.3.8 Impacts
Patients described a number of QoL domains being impacted: physical functioning, sleep, daily activities, working life, emotional/psychological wellbeing, diet, and social functioning (see Table 3).
Limitations in physical functioning, specifically gross motor movements, were reported by all patients, including difficulty walking (non-tophaceous: n = 18/20; tophaceous: n = 9/10) and limitation in range of movement (non-tophaceous: n = 18/20; tophaceous: n = 9/10) due to the pain and swelling that occurs particularly in the toe or foot. Patients also reported difficulty exercising, arising, and climbing stairs.
Sleep disturbance was the second most commonly reported impact, with most patients reporting difficulty falling asleep or being woken up by the pain during flares (non-tophaceous: n = 18/20; tophaceous: n = 10/10).
Impact of flares on their daily activities and working life was also discussed (non-tophaceous n = 18/20, tophaceous n = 10/10). Areas affected included work productivity (non-tophaceous: n = 15/20; tophaceous: n = 9/10), choice of footwear (non-tophaceous: n = 11/20; tophaceous: n = 3/10), and general daily routine (non-tophaceous: n = 10/20; tophaceous: n = 5/10).
Most patients (non-tophaceous: n = 15/20, tophaceous: n = 9/10) described impacts on their emotional or psychological well-being, notably, feelings of unhappiness/depression (non-tophaceous: n = 11/20, tophaceous: n = 2/10) and irritation/frustration (non-tophaceous: n = 9/20, tophaceous: n = 3/10) due to not being able to take part in usual daily activities or plans. Patients described feeling worried (non-tophaceous: n = 9/20, tophaceous: 6/10) about when they would experience the next flare.
3.4 Saturation Analysis
Conceptual saturation was achieved in both patient groups, with no new concepts emerging in the final set of interviews. For both patient groups, saturation was achieved after eight interviews whereby no new concepts emerged in any of the subsequent transcripts.
3.5 Digital Collection of RTQD
All core symptoms and proximal impact concepts emerged from both the patient interviews and the digital collection of RTQD. However, as the traditional interview methodology enabled more direct probing, nine additional concepts were elicited in comparison with the RTQD, including soreness, throbbing sensation, redness, physical weakness, difficulty bending down, difficulty with self-care tasks, difficulty driving, irritation, and frustration. While the interviews generally provided a greater depth of understanding regarding the descriptions of key concepts and identification of more distal concepts, the RTQD often brought the data ‘to life’ and better conveyed the severity of symptoms and impacts through visual imagery and spoken/written text captured at the time the symptom and/or impact was experienced. One patient sent a picture of his foot swelling during a flare and explained in a video: “The picture shows when the foot is inflamed and the swelling is so bad and it hurts so bad you can’t even get up off the bed.” Another patient recorded a video during the night when he was woken by pain: “Another night when you can’t sleep because you’re in pain and your feet is inflamed with gout, it’s very difficult … two in the morning, this pain is killing me.”
3.6 Conceptual Model
A key aim of the CE questioning was to inform the development of a conceptual model that comprehensively summarises the symptoms and impacts experienced by patients with gout (see Fig. 3). The model comprises all symptoms and impacts reported by patients and clinicians in the interviews. As presented in the model, symptoms were considered to be concepts proximal to gout, with impacts such as dietary or social functioning considered more distal. The majority of symptoms and impacts were elicited by both non-tophaceous and tophaceous patients. ‘Tophi’, ‘skin damage’, and ‘physical deformity’ were the only concepts elicited only by patients with tophaceous gout.
3.7 Clinician CE Interviews
Findings from the five clinician interviews supported the relevance of all symptoms and impacts elicited from patients in the CE interviews and RTQD. Clinicians described flares as self-defined by patients, of variable duration (longer without treatment), of variable frequency and abrupt onset, often worse at night or in the morning. Symptoms included severe pain (n = 5/5), redness (n = 4/5), swelling (n = 4/5), burning/warmth (n = 4/5), and tenderness/sensitivity to touch (n = 2/5). Three clinicians suggested tophi are largely asymptomatic unless physically touched and not overly bothersome (n = 3/5). Patients’ emotional well-being, physical functioning, activities of daily living, sleep, and diet/alcohol intake were considered most commonly impacted.
3.8 Patient Cognitive Debriefing (CD) Interviews
3.8.1 HAQ-DI
All patients (n = 30) were cognitively debriefed on the HAQ-DI and HAQ-VAS pain scale. The instructions and response options were generally well understood. Six patients (five with non-tophaceous gout; one with tophaceous) felt the 7-day recall period was not long enough to capture impacts of flares because of the variable frequency of their flares. With the exception of two ‘aids and devices’ items (‘built up or special utensils’ and ‘long-handled bathroom appliances’), all items were well understood and completed without difficulty. However, only 12 of 34 items were reported to be relevant by >50 % of the non-tophaceous sample (n = 20; see ESM 3). In contrast, 24 items were relevant to ≥50 % of the tophaceous sample, reflecting the greater functional impact of patients with tophaceous gout (n = 10; see ESM 4). No concepts of importance were reported to be missing by any of the patients.
The HAQ-VAS pain scale was well understood by all patients and relevant to nearly all patients who were asked (n = 10/11 patients).
3.8.2 ‘Overall Concern’ GAQ Domain
The 20 patients with non-tophaceous gout were cognitively debriefed on the items in the ‘overall concern’ GAQ domain. All items, the definition of a ‘gout attack’, instructions, and response options provided in the GAQ were well understood by all patients.
However, 7/13 items were not found to be relevant to ≥50 % of the non-tophaceous sample (see ESM 5). The lack of recall period also caused inconsistencies in the patients’ responses (i.e., during flares only, or during and between flares).
3.8.3 TIQ-20
The definition of a ‘gouty tophi’ was well understood by all ten patients with tophaceous gout. Patient understanding of item wording was also high. While 9/20 items were not described as relevant by ≥50 % of patients (see ESM 6), the concepts included in the TIQ-20 were reported by patients during CE. With no recall period, patients were unsure whether to consider only impacts of tophi experienced during flares (where the impact was reported to be greater) or whether to consider all impacts of their tophi.
3.9 Feedback from Expert Clinicians
Upon reviewing results from patient interviews, the expert clinicians found the preliminary conceptual model was consistent with their experience of treating patients with non-tophaceous gout. Additionally, the three expert clinicians agreed with the CD findings for the HAQ-DI (notably the lack of relevance in the non-tophaceous sample), explaining that the HAQ-DI is generally used with more severe or tophaceous gout that may limit physical functioning in the upper extremities.
3.10 Patient Advisors
The patient advisors deemed the types of questions in the interview guide to be relevant and worded appropriately. All CE and CD findings resonated with the advisors. The advisors confirmed the majority of items in the HAQ-DI and HAQ-VAS were not relevant to their experience of non-tophaceous gout that would flare in the lower extremities rather than the hands.
4 Discussion
This study employed a patient-centered approach [19, 21] to support the development of a conceptual model of gout patients’ experiences of symptoms, management of gout attacks (flares), tophi burden, and the broader impact of gout. This was followed by evaluation of the adequacy of existing PROs for measuring impacts from gout.
Consistent with the literature [8, 19, 36, 37], CE activities (both patient and clinician interviews and qualitative digital ethnography) identified pain as being the cardinal, defining symptom of gout, leading to a range of impacts on QoL. In particular, this study found that patients discussed severe debilitating flares of pain causing an inability to weight bear and an impact on physical functioning (e.g., difficulty walking), sleep, daily activities, and work (e.g., productivity) and social activities (e.g., missing/cancelling plans). Such findings support a previous qualitative interview study whereby pain, isolation, and work disability were described as key impacts of gout [10]. Furthermore, the findings are consistent with previous work that specifically demonstrated the impact of gout on work and productivity [10, 14]. The relationship between pain and sleep, and the subsequent impact on QoL, is also well documented in other pain conditions [38–40]. Interestingly, despite being mentioned by almost all patients in this study and as a key outcome identified in other qualitative studies, sleep disturbance did not make it into OMERACT’s core outcome domains for studies of acute and chronic gout [12]. Tophi were not considered generally bothersome, but were painful when knocked and impacted footwear choice.
The resulting conceptual model illustrates that the vast majority of symptoms elicited from patients with tophaceous gout were also reported by those with non-tophaceous gout, aside from those specifically related to tophi, such as skin damage. A model based on qualitative evidence is of value to aid selection of the optimal outcomes for monitoring, both in general clinical care and in clinical research, and evaluating treatment efficacy. The added value of digital RTQD should be considered in conjunction with traditional patient interview methods when designing future qualitative research [41]. While traditional patient interviews remain the gold standard in exploring the patient experience, qualitative data collected in real-time arguably have stronger ecological validity and provide valuable additional insights into the patient experience of non-tophaceous gout; specifically the severity of symptoms and impacts discussed. However, not all patients experienced flares during the period of digital data collection, therefore some concepts only emerged from the interviews.
CD findings and feedback from expert clinicians indicated that the HAQ-DI lacks relevance in the non-tophaceous gout sample, predominantly because most items assess impacts on physical functioning in the upper extremities and fine motor movements as opposed to lower extremities and gross motor movements. The HAQ-DI was more relevant to the patients with tophaceous gout, who were more likely to experience symptoms in the upper extremities. These findings support previous literature [8] and to some extent the OMERACT guidance to use the HAQ-DI for assessing physical impacts of chronic gout only, as the measure lacks sensitivity to capture the impact of gout in those with less severe disease. However, the findings also suggest potential value in developing a measure of functioning specific to gout and relevant to both patient groups that is less focused on the impact on upper extremities/fine motor skills and has greater focus on the lower extremities. The ability to effectively measure HRQoL is critical for assessing treatment benefit in terms of change over time and determining the best approach to managing gout [15].
The majority of concepts captured in the GAQ domain were reported to be too severe for patients with non-tophaceous gout, suggesting the domain will have limited value and is likely to have floor effects. The domain may have value in a population of patients with poorer control over their gout and who therefore potentially experience stronger emotional impacts—but the responsiveness of the instrument would need careful exploration.
CD findings for the TIQ-20 demonstrated conceptual comprehensiveness in capturing impacts on functioning specific to tophi. To capture the full impact of all gout symptoms (and not just tophi-specific burden), it is recommended the measure is used in conjunction with an instrument capturing wider functional impacts of gout. Additionally, in terms of measuring a treatment intervention, it may be useful to employ a response scale capturing severity from 0 to 10 to clearly capture improvement rather than an attitudinal scale (agree/disagree), and to clarify the recall period.
5 Limitations and Future Research
While the patient advisors supported a ‘patient-centric’ approach [19, 21], only two advisors were engaged, the views of whom may not represent the diversity of views among the gout patient population. To capture a greater breadth of experience, future research could include more patient advisors. It is also important to note that, while quantitative data have been reported in terms of the frequency of concepts reported, the data are based on a small number of patients, therefore limiting the generalizability of the findings. Finally, it is acknowledged that real-time data capture was only employed in the sample of patients with non-tophaceous gout because of logistical challenges, and future research could explore the added value of utilizing this novel method in a sample of patients with tophaceous gout.
6 Conclusions
In this qualitative interview study, a patient-centric approach combined expert clinical input with patient interviews and novel digital methods of qualitative data collection to increase patient engagement and the ecological validity of the data. The findings provide evidence that the instruments evaluated have some value for the assessment of patients with gout but also some limitations. These shortcomings could be overcome with modifications or through the development of a new measure capturing all functional impacts in both populations as guided by the conceptual model.
References
Smith EU, Diaz-Torne C, Perez-Ruiz F, March LM. Epidemiology of gout: an update. Best Prac Res Clin Rheumatol. 2010;24(6):811–27. doi:10.1016/j.berh.2010.10.004.
Zhu Y, Pandya B, Choi H. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 2011;63:3136–41.
Torjesen I. Rates of gout continue to rise in UK, but GP care has not improved. BMJ. 2014;358. doi:10.1136/bmj.g239.
Underwood M. Diagnosis and management of gout. BMJ. 2006;332(7553):1315–9. doi:10.1136/bmj.332.7553.1315.
Roddy E. Revising the pathogenesis of podagra: why does gout target the foot? J Foot Ankle Res. 2011;4(13).
Cassagnol M, Saad M. Pharmacologic Management of Gout. US Pharm. 2013;38(3):22–6.
Perez-Ruiz F. Treating to target: a strategy to cure gout. Rheumatology. 2009;48(suppl 2):ii9–14. doi:10.1093/rheumatology/kep087.
Chandratre P, Roddy E, Clarson L, Richardson J, Hider SL, Mallen CD. Health-related quality of life in gout: a systematic review. Rheumatology (Oxford, England). 2013;52(11):2031–40. doi:10.1093/rheumatology/ket265.
Schumacher HR Jr, Wortmann RL. Monosodium urate crystal deposition arthropathy part I: review of the stages and diagnosis of gout. Adv Stud Med. 2005;5(3):133–8.
Lindsay K, Gow P, Vanderpyl J, Logo P, Dalbeth N. The experience and impact of living with gout: a study of men with chronic gout using a qualitative grounded theory approach. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis. 2011;17(1):1–6. doi:10.1097/RHU.0b013e318204a8f9.
Prowse RL, Dalbeth N, Kavanaugh A, Adebajo AO, Gaffo AL, Terkeltaub R, et al. A delphi exercise to identify characteristic features of gout—opinions from patients and physicians, the first stage in developing new classification criteria. J Rheumatol. 2013;40(4):498–505. doi:10.3899/jrheum.121037.
Schumacher HR, Taylor W, Edwards L, Grainger R, Schlesinger N, Dalbeth N, et al. Outcome domains for studies of acute and chronic gout. J Rheumatol. 2009;36(10):2342–5. doi:10.3899/jrheum.090370.
Klooster PM, Vonkeman HE, Oude Voshaar MAH, Bode C, Laar MAFJ. Experiences of gout-related disability from the patients’ perspective: a mixed methods study. Clin Rheumatol. 2013;33(8):1145–54. doi:10.1007/s10067-013-2400-6.
Kleinman NL, Brook RA, Patel PA, Melkonian AK, Brizee TJ, Smeeding JE, et al. The impact of gout on work absence and productivity. Value Health. 2007;10(4):231–7. doi:10.1111/j.1524-4733.2007.00173.x.
Kim SY, Choi HK. Gout and quality of life. J Rheumatol. 2009;36(5):865–8. doi:10.3899/jrheum.090034.
Grainger R, Taylor WJ, Dalbeth N, Perez-Ruiz F, Singh JA, Waltrip RW, et al. Progress in measurement instruments for acute and chronic gout studies. J Rheumatol. 2009;36(10):2346–55.
Singh J, Taylor W, Simon L, Khanna P, Stamp L, McQueen F et al. Patient-reported outcomes in chronic gout: a report from OMERACT 10. J Rheumatol. 2011;38(7):1452–7.
Colwell HH, Hunt BJ, Pasta DJ, Palo WA, Mathias SD, Joseph-Ridge N. Gout Assessment Questionnaire: initial results of reliability, validity and responsiveness. Int J Clin Pract. 2006;60(10):1210–7. doi:10.1111/j.1742-1241.2006.01104.x.
Aati O, Taylor WJ, Siegert RJ, Horne A, House ME, Tan P, et al. Development of a patient-reported outcome measure of tophus burden: the Tophus Impact Questionnaire (TIQ-20). Ann Rheum Dis. 2015;74(12):2144–50.
Burke L, Stifano T, Dawisha S. Guidance for industry: patient-reported outcome measures: Use in medical product development to support labeling claims: Draft guidance. Health Qual Life Outcomes 2006;4:79.
Frank L, Forsythe L, Ellis L, Schrandt S, Sheridan S, Gerson J, et al. Conceptual and practical foundations of patient engagement in research at the patient-centered outcomes research institute. Qual Life Res. 2015;24(5):1033–41. doi:10.1007/s11136-014-0893-3.
Patrick DL, Burke LB, Powers JH, Scott JA, Rock EP, Dawisha S, et al. Patient-reported outcomes to support medical product labeling claims: FDA perspective. Value Health. 2007;10(Suppl 2):S125–37. doi:10.1111/j.1524-4733.2007.00275.x
Lasch KE, Marquis P, Vigneux M, Abetz L, Arnould B, Bayliss M, et al. PRO development: rigorous qualitative research as the crucial foundation. Qual Life Res. 2010;19(8):1087–96. doi:10.1007/s11136-010-9677-6.
Leidy NK, Vernon M. Perspectives on patient-reported outcomes: content validity and qualitative research in a changing clinical trial environment. PharmacoEconomics. 2008;26(5):363–70.
Ericsson KA, Simon HA. Verbal reports as data. Psychol Rev. 1980;87(3):215.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. Thousand Oaks: Sage Publications; 2004.
Poole JL, Steen VD. The use of the Health Assessment Questionnaire (HAQ) to determine physical disability in systemic sclerosis. Arthritis Rheum. 1991;4(1):27–31.
Bruce B, Fries JF. The Stanford Health Assessment Questionnaire: a review of its history, issues, progress, and documentation. J Rheumatol. 2003;30(1):167–78.
Fries JF, Spitz PW, Young DY. The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. J Rheumatol. 1982;9(5):789.
Taylor W, Colvine K, Gregory K, Collis J, McQueen F, Dalbeth N. The Health Assessment Questionnaire Disability Index is a valid measure of physical function in gout. Clin Exp Rheumatol. 2008;26(4):620.
Hirsch JD, Lee SJ, Terkeltaub R, Khanna D, Singh J, Sarkin A, et al. Evaluation of an instrument assessing influence of gout on health-related quality of life. J Rheumatol. 2008;35(12):2406–14.
Joffe H, Yardley L. Content and thematic analysis. In: Marks DF, Yardley L, editors. Research methods for clinical and health psychology. London: Sage Publications; 2004. p. 56–68.
Leeuwen T, Jewitt C. The handbook of visual analysis. London: Sage; 2001.
Atlas.ti software version 7 (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany). 2013.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18:59–82.
Brook RA, Forsythe A, Smeeding JE, Lawrence Edwards N. Chronic gout: epidemiology, disease progression, treatment and disease burden. Curr Med Res Opin. 2010;26(12):2813–21.
Dalbeth N, Zhong CS, Grainger R, Khanna D, Khanna PP, Singh JA, et al. Outcome measures in acute gout: a systematic literature review. J Rheumatol. 2014;41(3):558–68.
Cohen SD, Patel SS, Khetpal P, Peterson RA, Kimmel PL. Pain, sleep disturbance, and quality of life in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2007;2(5):919–25. doi:10.2215/cjn.00820207.
Menefee LA, Frank ED, Doghramji K, Picarello K, Park JJ, Jalali S, et al. Self-reported sleep quality and quality of life for individuals with chronic pain conditions. Clin J Pain. 2000;16(4):290–7.
Morin CM, Gibson D, Wade J. Self-reported sleep and mood disturbance in chronic pain patients. Clin J Pain. 1998;14(4):311–4.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Acknowledgments
In addition to the authors, Fernando Perez-Ruiz, Jordan Kelsey, and David Trock were involved in the research as clinical experts in gout, and Victor Villa and Kathleen Hagerty were involved as patient advisors, who provided input into the development of study documents and analysis. The PF649 team at Pfizer also provided input into the development of study documents and data analysis.
Author contributions
Katja Rüdell participated in the study design, methods, qualitative analysis, and reviewing, and contributed to the manuscript. Sophi Tatlock, Charlotte Panter, and Rob Arbuckle participated in the study design, data collection, analysis, key meetings, discussions, and write-up of the study. Leslie R. Harrold and William J. Taylor participated in the clinician interviews, data analysis, and revision of the manuscript. Tara Symonds participated in the design, results and conclusions, and revision of the manuscript. All authors contributed to the writing of the manuscript and reviewed and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was sponsored by Pfizer. Katja Rudell and Tara Symonds were employees of Pfizer Ltd when the research was conducted and were shareholders of Pfizer. Sophi Tatlock, Charlotte Panter, and Rob Arbuckle are employees of Adelphi Values who were paid consultants to Pfizer in connection with the development of this manuscript. Leslie Harold and Will Taylor were financially compensated by Pfizer for their participation in the clinicians interviews; however, they were not financially compensated for their involvement in the study or their development of this manuscript. The study was approved and overseen by an Independent Review Board in the US (approval codes: ADE1-14-472, ADE2-14-168) and was performed in accordance with the ethical standards of the Declaration of Helsinki. Written informed consent was obtained prior to the collection of any data.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tatlock, S., Rüdell, K., Panter, C. et al. What Outcomes are Important for Gout Patients? In-Depth Qualitative Research into the Gout Patient Experience to Determine Optimal Endpoints for Evaluating Therapeutic Interventions. Patient 10, 65–79 (2017). https://doi.org/10.1007/s40271-016-0184-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-016-0184-x