Abstract
Background
Patient-reported outcomes (PROs) can provide important information about treatment tolerability in HIV-1-infected patients.
Objective
The aim of this study was to evaluate PROs following switching from a boosted protease inhibitor-based regimen to the single-tablet regimen (STR) of rilpivirine/emtricitabine/tenofovir disoproxil fumarate (RPV/FTC/TDF) in the 48-week open-label Switching Boosted PI to Rilpivirine in Combination with Truvada as a Single-Tablet Regimen (SPIRIT) trial.
Methods
In the open-label SPIRIT trial, patients were randomized to receive an STR of RPV/FTC/TDF (n = 317) for 48 weeks or stay on their baseline regimen of a ritonavir-boosted protease inhibitor and two nucleoside/nucleotide analog reverse transcriptase inhibitors (PI + RTV + 2NRTIs, n = 159) for 24 weeks before switching to RPV/FTC/TDF for another 24 weeks. PRO assessments included the HIV Treatment Satisfaction Questionnaire (TSQ) and the HIV Symptom Index Questionnaire (SIQ).
Results
At week 24, the mean HIV TSQ improvement from baseline was significantly greater in the RPV/FTC/TDF group than the PI + RTV + 2NRTIs group (p < 0.001). On the HIV SIQ, the percentage of patients reporting a shift from ‘symptom’ to ‘no symptom’ was significantly greater with RPV/FTC/TDF treatment compared with PI + RTV + 2NRTIs for all items (all p ≤ 0.01), with total within-group occurrence of 13/20 symptoms significantly decreasing from baseline for RPV/FTC/TDF patients. In the delayed switch group, significantly fewer patients reported diarrhea and sleep problems at week 48 vs. week 24.
Conclusions
These data suggest that switching to the STR RPV/FTC/TDF from a PI-based multi-pill regimen is associated with greater patient-reported treatment satisfaction and improved tolerability in HIV-1-infected, virologically suppressed individuals.
Similar content being viewed by others
Patient-reported outcomes can provide significant insight into effectiveness and tolerability of anti-HIV treatments. |
Switching from multi-pill regimens to rilpivirine-based single-tablet regimens may lead to greater patient-reported satisfaction and improved tolerability in HIV-positive patients with virological suppression. |
1 Introduction
Single-tablet regimens (STRs) taken once daily represent a major advancement in the treatment of HIV infection. Available data suggest that reduced pill burden in HIV-infected individuals may result in better efficacy, tolerability, and greater treatment satisfaction, compared with multi-pill regimens [1, 2]. In addition, STRs can arguably maximize the benefits of antiretroviral therapy (ART) by reducing pill burden and simplifying dosage schedule, thereby improving adherence [3].
The trial Switching PI to Rilpivirine in combination with Truvada (SPIRIT, ClinicalTrials.gov identifier NCT01252940) was conducted in HIV-1-infected, virologically suppressed patients [4]. It showed that switching from a multi-pill regimen consisting of a ritonavir-boosted protease inhibitor (PI + RTV) plus two nucleoside or nucleotide analog reverse transcriptase inhibitors (NRTIs) to the STR comprising of rilpivirine, emtricitabine, and tenofovir disoproxil fumarate (RPV/FTC/TDF) was associated with maintenance of virologic suppression, low risk of virological failure or drug–drug interactions, as well as improvements in serum lipid levels and overall tolerability, based on adverse event (AE) reporting [4]. The effects of switching from a multi-pill regimen to the STR RPV/FTC/TDF in this trial were also assessed over 48 weeks using patient-reported outcomes (PROs), and those results have not been previously reported.
PROs can be very useful in the clinical management of HIV/AIDS. For example, available data suggest that PRO questionnaires may be more sensitive instruments for detecting symptoms and estimating their severity than AE-collecting protocols [5, 6], and patient-reported symptoms (especially fatigue, dizziness, fever, appetite, sleep trouble, and muscle/joint pain) were shown to correlate more strongly with measures of quality of life (QoL), physical health, hospitalization, and survival than provider-reported symptoms [5, 7–10]. In addition, higher patient-reported symptom scores, concerns about AEs, and symptom persistence following ART use have been associated with lower treatment adherence [11–13] and with a greater risk of breaking trust between an HIV-infected patient and her/his healthcare provider [14]. The value of PROs has been recognized by the US FDA, which recently committed to the Patient-Focused Drug Development initiative, the goal of which is to obtain the patient perspective in certain diseases, including HIV/AIDS [15].
In this paper, we report the protocol-specified analyses of patient-reported treatment adherence and treatment satisfaction, as well as a post hoc analysis of the change in occurrence of common HIV symptoms following the switch to an STR consisting of RPV/FTC/TDF in the SPIRIT study.
2 Methods
2.1 Study Design
The study design details have been reported previously [4]. Briefly, the SPIRIT study was an open-label, multinational, multicenter, phase IIIB, 48-week trial in which patients were randomized 2:1 to either switch from their baseline regimen (ritonavir-boosted protease inhibitor [PI + RTV] + 2NRTIs) to the STR RPV/FTC/TDF (rilpivirine 25 mg/emtricitabine 200 mg/tenofovir DF 300 mg; Complera® [US], Eviplera® [EU]; supplied by Gilead Sciences, Inc.), or to stay on their baseline PI + RTV + 2NRTIs regimen for 24 weeks. At week 24, patients in the RPV/FTC/TDF group continued with that regimen, while patients in the PI + RTV + 2NRTIs group also switched to RPV/FTC/TDF (Fig. 1).
SPIRIT Trial design. ART antiretroviral therapy, NRTI nucleoside or nucleotide analog reverse transcriptase inhibitor, NNRTI non-nucleoside reverse transcriptase inhibitor, PI protease inhibitor, RTV ritonavir, RPV/FTC/TDF single-tablet regimen consisting of rilpivirine, emtricitabine, and tenofovir disoproxil fumarate, STR single-tablet regimen, VL viral load
2.2 Participants
The trial included men and women, ≥18 years of age, with a life expectancy of at least 1 year, with two sequential plasma HIV-1 RNA <50 copies/mL (using a local assay) over ≥6 months at screening, who were receiving their first or second ART regimen consisting of a PI + RTV plus two NRTIs continuously for ≥6 months prior to screening. Patients randomized to continue PI + RTV + 2NRTIs, and whose two NRTIs were FTC and TDF, were supplied FTC/TDF fixed-dose combination by the study sponsor. Patients were also required to have normal electrocardiogram results, estimated glomerular filtration rate ≥70 mL/min, hepatic transaminases and serum amylase ≤5 times the upper limit of normal, total bilirubin ≤1.5 mg/dL, and adequate hematologic parameters. Exclusion criteria included a history of resistance (including documented genotyping results for the reverse transcriptase resistance mutations K65R, K101E/P, E138G/K/R/Q, Y181C/I/V, M184V/I, or H221Y) or hypersensitivity to any of the study agents at any time, acute hepatitis within 30 days before study entry, active serious infections, liver disease, history of malignancies (within the previous 5 years), current use of drugs contraindicated for use with RPV, FTC, or TDF, current use of investigational drugs or unapproved enrollment in other clinical studies, and use of immunosuppressants within 3 months prior to study entry. At baseline, patients were required to complete an enrollment survey to evaluate the reason for willingness to switch their ART regimen. The study was approved by individual Institutional Review Boards and conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave their informed consent prior to inclusion in the study.
2.3 Patient-Reported Outcome Measures
Patients read and answered questions from the PRO questionnaires themselves, at visits indicated below for each instrument.
2.3.1 Visual Analog Scale (VAS) Adherence Questionnaire [16]
Adherence to the treatment regimen was estimated using this validated instrument by patients marking a linear scale ranging from 0 % (no ART doses taken) to 100 % (all doses prescribed taken). The questionnaires were completed at baseline and at weeks 4, 8, 12, 24, 36, and 48 for both groups, and additionally at weeks 28 and 32 for the PI + RTV + 2NRTIs group, representing their week 4 and week 8 after switching to RPV/FTC/TDF.
2.3.2 HIV Treatment Satisfaction Questionnaire (TSQ) [17]
The HIV Treatment Satisfaction Questionnaire (HIV TSQ) is a validated 10-item instrument (Table 1) that was initially completed by patients at baseline (HIV TSQs [status at baseline]), with scores ranging from 0 (least favorable response) to 6 (most favorable response; score range: 0–60, with higher scores indicating greater treatment satisfaction), with a recall period encompassing ‘the past few weeks’. Scores 1–5 do not have specific descriptions defined on the questionnaire but represent intermediary responses between least favorable and most favorable. At weeks 24 and 48, the post-baseline score change for each item was assessed using the HIV TSQc (change from baseline) scale ranging from −3 (least favorable response) to +3 (most favorable overall response for the ten questions; score change range: −30 to +30, with scores <0 and >0 indicating a decrease and increase in treatment satisfaction, respectively). Patients were instructed to compare their present satisfaction with their experience just prior to initiating the new therapy. Scores from −2 to +2 do not have specific descriptions assigned; rather, they represent intermediary responses between least favorable and most favorable.
Two HIV TSQ subscales were also evaluated, with five items each: The General Satisfaction/Clinical subscale (1, 2, 3, 9, and 10) and the Lifestyle/Ease subscale (4–8) [17]. Baseline scores for each subscale ranged from 0–30, with post-baseline score changes ranging from −15 to +15.
2.3.3 HIV Symptom Index Questionnaire (SIQ) [18]
The HIV Symptom Index Questionnaire (HIV SIQ; Table 2), a validated instrument, was used to assess a total of 20 symptoms on a 5-point scale (0, I do not have this symptom; 1, does not bother me; 2, bothers me a little; 3, it bothers me; 4, it bothers me a lot), for a total score range of 0–80. The questionnaires were completed at baseline and at weeks 4, 8, 12, 24, 36, and 48 for both groups, and additionally at weeks 28 and 32 for the PI + RTV + 2NRTIs group. The recall period at each visit was 4 weeks.
2.4 Statistical Analysis
Analyses were based on the full data set, which comprised all randomized patients who received at least one dose of study medication; patients with missing surveys were not included in the analysis. The Visual Analog Scale percentage scores at each visit and change from baseline were descriptively summarized; the within-group and between-group comparisons of changes from baseline were performed using the Wilcoxon rank sum test. Total HIV TSQ scores and subscale scores at baseline and their changes from baseline to weeks 24 and 48 were descriptively summarized; the between-group comparison of the total score changes from baseline to week 24 was performed using an analysis of covariance (ANCOVA) model, with the baseline score as a covariate. For each HIV SIQ item, scores were dichotomized to indicate a response (presence of a symptom: scores 1, 2, 3, or 4) or no response (absence of a symptom: score 0), and the within-group percentages of patients experiencing the presence of each of the 20 symptoms at each visit were compared vs. baseline using the McNemar test. Post hoc between-group comparisons of proportions of patients who reported a shift in symptom status (from ‘symptom’ to ‘no symptom’ and vice versa) from baseline at week 24 were performed using the Cochran–Mantel–Haenszel row mean score test with modified ridit scores.
3 Results
3.1 Patient Disposition and Demographics
Baseline demographic and clinical characteristics have been previously reported [4]. Of the 476 enrolled patients, 87.6 % (417/476) were men, 76.7 % (365/476) were White, and the mean ± SD age was 42 ± 9 years. The mean duration of ART was 3.3 ± 2.2 years, and the most common NRTI combination at screening was a fixed-dose combination of FTC/TDF (385/476 [80.9 %]). The most common PIs were atazanavir (176 [37.0 %]), lopinavir (155 [32.6 %]), and darunavir (96 [20.2 %]). The only demographic characteristic with a between-group difference exceeding 5 % was the percentage of Black patients (RPV/FTC/TDF 19.2 % [61/317]; PI + RTV + 2NRTIs 13.8 % [22/159]). A total of 152 (95.6 %) patients in the PI + RTV + 2NRTIs group switched to RPV/FTC/TDF at week 24.
In both groups, most patients noted a desire to simplify their current anti-HIV regimen as their reason to enroll in the study; a greater proportion of patients randomized to stay on their baseline regimen (PI + RTV + 2NRTIs) than patients randomized to switch to RPV/FTC/TDF reported a concern about the long-term side effects of current ART as their reason for enrollment (21.4 vs. 13.9 %; Table 3).
3.2 VAS Adherence Questionnaire
Patient-reported adherence rates at baseline were 97.0 % (RPV/FTC/TDF) and 98.2 % (PI + RTV + 2NRTIs). At week 4, a significant increase in adherence from baseline was observed in the RPV/FTC/TDF group (1.4 ± 12.5 %, p = 0.006) but not in the PI + RTV + 2NRTIs group (−0.6 ± 6.2 %, p = 0.73), and both groups had significant improvements in adherence from baseline to weeks 8 (RPV/FTC/TDF, 1.4 ± 11.0 %, p < 0.001; PI + RTV + 2NRTIs, 0.7 ± 3.2 %, p = 0.034) and 12 (RPV/FTC/TDF, 1.6 ± 12.5 %, p < 0.001; PI + RTV + 2NRTIs, 0.9 ± 2.7 %, p < 0.001). Changes in adherence from baseline at weeks 24, 36, and 48 were not significant for the RPV/FTC/TDF group. Adherence in the PI + RTV + 2NRTIs group improved significantly at weeks 28 (0.6 ± 9.0 %, p < 0.001) and 32 (0.7 ± 4.5 %, p = 0.036), i.e. 4 and 8 weeks post-switch, respectively.
3.3 HIV TSQ
At baseline, the mean HIV TSQ score in both groups was 51, i.e. at 85 % of the maximum of 60 (Table 4). At week 24, the mean improvement in treatment satisfaction from baseline in the RPV/FTC/TDF group was 60 % greater than the one observed in the PI + RTV + 2NRTIs group (24 vs. 15, p < 0.001); patients in the PI + RTV + 2NRTIs group who switched to RPV/FTC/TDF experienced a mean total HIV TSQc improvement of 23 from week 24 to 48 (Table 4). The improvements in total treatment satisfaction at weeks 24 and 48 were equally attributable to the changes observed in the General Satisfaction/Clinical and Lifestyle/Ease subscales (Table 4). The baseline to week 24 changes in response to the individual questions that comprise the TSQ are shown in electronic supplementary Fig. 1.
3.4 HIV SIQ
At baseline, the overall occurrence of symptoms captured by HIV SIQ ranged from 15.2 % (67/440; nausea) to 50.6 % (221/437; fatigue). For 17 of 20 symptoms, the between-group difference in occurrence at baseline was ≤5 %, and <10 % for the remaining three (hand/foot pain, nausea, and memory loss) (Table 5).
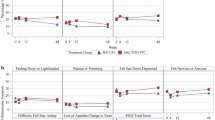
At week 24, the occurrence of each of the 20 HIV SIQ symptoms in the RPV/FTC/TDF group was lower than that recorded in the PI + RTV + 2NRTIs group, with occurrence differences of >10 % being observed for diarrhea, bloating/gas, skin problems, and problems having sex (Figs. 2, 3; Table 5). The visit-by-visit rates of diarrhea, bloating/gas, and problems having sex are presented in Fig. 3 (for all HIV SIQ symptoms, see electronic supplementary Fig. 2).
HIV Symptom Index Questionnaire: individual symptom rates at week 24 (scores 1, 2, 3, or 4). NRTI nucleoside or nucleotide analog reverse transcriptase inhibitor, PI protease inhibitor, RTV ritonavir, RPV/FTC/TDF single-tablet regimen consisting of rilpivirine, emtricitabine, and tenofovir disoproxil fumarate; *p < 0.05, **p < 0.01, ***p < 0.001 (within-group comparison vs. baseline using the McNemar test)
HIV Symptom Index Questionnaire: visit-by-visit rates of three symptoms with between-group rate difference of ≥10 % at week 24. Of the 159 patients initially treated with their baseline PI + RTV + 2NRTIs regimen, 152 switched to RPV/FTC/TDF at week 24 (delayed-switch arm). NRTI nucleoside or nucleotide analog reverse transcriptase inhibitor, PI protease inhibitor, RTV ritonavir, RPV/FTC/TDF single-tablet regimen consisting of rilpivirine, emtricitabine, and tenofovir disoproxil fumarate; *p < 0.05, **p < 0.01, ***p < 0.001 for within-group comparison vs. baseline (RPV/FTC/TDF, PI + RTV + 2NRTIs) or vs. week 24 (delayed switch), using the McNemar test
Within the RPV/FTC/TDF group, the occurrences of 13 of 20 symptoms were significantly lower at week 24 than at baseline; of these, seven symptoms had a >10 % reduction from baseline (fatigue, diarrhea, sadness, bloating/gas, muscle/joint pain, sex problems, and anxiety). No significant within-group differences were observed for any of the symptoms in the PI + RTV + 2NRTIs group at week 24 compared with baseline (Table 5, electronic supplementary Fig. 2). With the exception of three HIV SIQ symptoms (hand/foot pain, headache, appetite loss), switching to RPV/FTC/TDF at the start of the study was associated with a significant reduction in occurrence within 4, 8 or 12 weeks compared with baseline (electronic supplementary Fig. 2).
At week 48, there were significantly fewer patients in the RPV/FTC/TDF group reporting symptoms of fatigue, diarrhea, bloating/gas, muscle aches/joint pain, and problems having sex compared with baseline. Among patients who switched from PI + RTV + 2NRTIs to RPV/FTC/TDF at week 24, the percentages of those reporting diarrhea and difficulty falling or staying asleep were significantly reduced at week 48 compared with week 24; no symptoms significantly worsened in either group after patients switched to RPV/FTC/TDF therapy (Table 5).
The post hoc between-group analysis revealed that, compared with staying on the PI + RTV + 2NRTI regimen, switching to RPV/FTC/TDF resulted in significant improvements from baseline to week 24 on each HIV SIQ item, as measured by the shift in scores of 1–4 (‘symptom’) to 0 (‘no symptom’) (Fig. 4). The treatment switch was associated with a subset of patients shifting from ‘symptom’ to ‘no symptom’ status on each of the HIV SIQ items, with no such shifts being registered in the arm randomized to stay on their PI + RTV + 2NRTI regimen. In addition, a lower proportion of RPV/FTC/TDF-treated than PI + RTV + 2NRTI-treated patients reported a shift from ‘no symptom’ to ‘symptom’ on 14 of 20 HIV SIQ items (Fig. 4). In this analysis, the greatest improvements in the RPV/FTC/TDF group were recorded for diarrhea (33.5 % shifting from ‘symptom’ to ‘no symptom’), bloating/gas (23.6 %), and fatigue (22.1 %) (Fig. 4).
HIV Symptom Index Questionnaire: change in symptom status from baseline to week 24 (post hoc analysis). The combined rates of improvement, worsening, and no change comprise 100 % (the rates of no change were not presented). In addition, no patients in the PI + RTV + 2NRTIs arm demonstrated improvement. NRTI nucleoside or nucleotide analog reverse transcriptase inhibitor, PI protease inhibitor, RTV ritonavir, RPV/FTC/TDF single-tablet regimen consisting of rilpivirine, emtricitabine, and tenofovir disoproxil fumarate; *p < 0.05, **p < 0.01, ***p < 0.001 (between-group comparisons using a Cochran–Mantel–Haenszel row mean score test with modified ridit scores)
4 Discussion
This analysis of PROs from the open-label SPIRIT trial suggests that switching HIV-1-infected, virologically suppressed patients from a PI + RTV + 2NRTI regimen to the STR RPV/FTC/TDF is associated with greater treatment satisfaction and a lower occurrence of a variety of HIV/AIDS-associated or treatment-associated symptoms, especially diarrhea and bloating/gas. The observed advantages of the STR RPV/FTC/TDF over the baseline regimen of PI + RTV + 2NRTI could be a consequence of better tolerability of the individual treatment components, reduced pill burden, or lower dosing frequency. However, with the exception of a transient effect following the first 4 weeks of treatment, the improvements in tolerability and patient satisfaction with the STR did not translate into a significant improvement in treatment adherence, most likely due to the fact that adherence in both groups was high, both at baseline and throughout the trial.
It should be pointed out that the advantages observed 24 weeks into STR RPV/FTC/TDF therapy were more pronounced in the immediate-switch group compared with the delayed-switch group. This could be a consequence of greater satisfaction with immediate switching (or dissatisfaction with delayed switching, or both), as 88.2 % of participants listed a desire to simplify their current anti-HIV regimen as the main reason to enroll in the trial (Table 3). That said, even the delayed-switch group experienced a nominal reduction in occurrence in 14 of 20 HIV SIQ symptoms and a significant improvement over baseline in two (diarrhea, sleep trouble; Table 5).
Some apparent benefits of switching to the STR RPV/FTC/TDF (e.g. decrease in the proportion of patients reporting feelings of sadness or anxiety) are not easy to interpret. It was shown previously that RPV could be associated with fewer neuropsychiatric symptoms than efavirenz (EFV) [19] but, to the best of our knowledge, there have been no previous comparisons between RPV- and PI-based regimens in this regard. These neuropsychiatric benefits could also be a reflection of positive expectations of a new therapy in an open-label trial, or related to an easier treatment regimen, including the possibility of feeling less ill or less burdened when taking one pill to treat HIV (historically, HIV/AIDS treatment regimens have been associated with a large pill burden). In addition, a greater proportion of patients in the PI + RTV + 2NRTIs arm than in the RPV/FTC/TDF arm (21.4 vs. 13.9 %) were concerned about the long-term side effects of their current treatment (Table 3), which could have had a differential effect on mental state in the two groups.
Results from this study suggest a greater range of patient-reported benefits than those observed in the only other trial to date that assessed the PRO effects of switching from a multi-pill regimen (PI-based or NNRTI-based) to an STR [20, 21]. In that 48-week trial, also conducted in a predominantly male population (88 %) of virologically suppressed, HIV-1-infected patients with a high adherence to treatment [20], the group that switched to the STR EFV/FTC/TDF reported a lower occurrence of four HIV SIQ symptoms (diarrhea, bloating/gas, changes in body appearance, problems having sex) at week 48 compared with baseline, while the group randomized to stay on their baseline regimen did not have any significant symptom improvements [21]. An apparent wider range of benefits following a switch to RPV/FTC/TDF in this trial compared with EFV/FTC/TDF in the previous trial may be due to replacement of a PI-based regimen with an NNRTI-based regimen (in the EFV/FTC/TDF trial, approximately half of the study population were using PIs at baseline [20], as opposed to all the patients in this trial) and potentially due to a better tolerability of RPV compared with EFV.
Although the differences in utility between various PRO tools used in HIV trials are not yet clear [22], it is increasingly recognized that the integration of PRO data into clinical practice (e.g. maintaining a database of PROs associated with individual ART regimens that also includes the degree of bother) would facilitate patient counseling and treatment optimization, and therefore improve patients’ QoL [22–24]. In addition, an accurate assessment of PROs could address the problem of underreporting certain AEs in clinical trials [9]. This phenomenon may be generated by patients not reporting a symptom that they had grown accustomed to or considered difficult to improve (and which they would be more likely to report if prompted by a PRO questionnaire, as opposed to reporting it as an AE during a clinical encounter) or by physicians neglecting symptoms that are multifactorial in origin and not easily addressed (e.g. fatigue) [6]. For example, the treatment-emergent AEs collected by SPIRIT investigators suggested a total 24-week occurrence of diarrhea of 7.9 % for the RPV/FTC/TDF group and 5.0 % for the PI + RTV + 2NRTIs group (Gilead Sciences, Inc., data on file), with the rates of diarrhea deemed by the investigators as related to study medication of 3.2 and 0.6 %, respectively [4]. Conversely, data from the SIQ demonstrate that, compared with baseline, there were significantly fewer patients reporting diarrhea in the RPV/FTC/TDF group at all post-baseline visits, and that the shift in symptom status at week 24 was significantly better than the one observed in the PI + RTV + 2NRTIs treatment arm. In addition, it has been reported that diarrhea associated with PI treatment generally resolves within several weeks of the initiation of therapy [25]. In contrast, the PRO data indicate a much higher baseline frequency of that symptom (49.7 %), with benefits of switching to the STR RPV/FTC/TDF (19.3 vs. 49.7 % for PI + RTV + 2NRTIs at week 24), suggesting that PROs are more sensitive in estimating the actual rates of certain symptoms, which is in agreement with the available literature [5, 6]. Based on the discrepancies in symptom occurrence reported as AEs and PROs, the authors of this paper believe that all HIV/AIDS clinical trials should consider employing a PRO assessment tool. The importance of PROs is also underscored by an observation that their integration in clinical practice can lead to improved patient–provider trust and communication [23]; conversely, a poorly optimized treatment regimen has been shown to result in low patient satisfaction, which may lead to the breach of patient–provider trust and abandonment of treatment [14].
Limitations of this trial include the open-label design, the predominance of male and White patients, and the fact that eligible patients were already highly adherent to their multi-pill baseline regimen. A trial that would mimic a real-life scenario of patients switching to an STR due to poor multi-pill regimen adherence, caused by poor tolerability or other factors, would be informative but possibly difficult to conduct. In addition, our trial did not include recently developed HIV-specific QoL questionnaires such as PROQOL-HIV [26], which would have allowed for additional validation of PRO results.
5 Conclusions
These results suggest that in HIV-1-infected, virologically suppressed individuals, switching to the STR RPV/FTC/TDF from a ritonavir-boosted PI regimen with two NRTIs is associated with greater treatment satisfaction and better tolerability, as reported by patients. Because guidelines increasingly recommend starting lifelong therapy as early as possible, and because the life expectancy of HIV-infected individuals has measurably improved, the use of effective, easier-to-take ART regimens is imperative for HIV-infected patients embarking upon therapy.
References
Aldir I, Horta A, Serrado M. Single-tablet regimens in HIV: does it really make a difference? Curr Med Res Opin. 2014;30:89–97.
Nachega JB, Parienti JJ, Uthman OA, Gross R, Dowdy DW, Sax PE, et al. Lower pill burden and once-daily antiretroviral treatment regimens for HIV infection: a meta-analysis of randomized controlled trials. Clin Infect Dis. 2014;58:1297–307.
Llibre JM, Clotet B. Once-daily single-tablet regimens: a long and winding road to excellence in antiretroviral treatment. AIDS Rev. 2012;14:168–78.
Palella FJ Jr, Fisher M, Tebas P, Gazzard B, Ruane P, Van Lunzen J, et al. Simplification to rilpivirine/emtricitabine/tenofovir disoproxil fumarate from ritonavir-boosted protease inhibitor antiretroviral therapy in a randomized trial of HIV-1 RNA-suppressed participants. AIDS. 2014;28:335–44.
Justice AC, Rabeneck L, Hays RD, Wu AW, Bozzette SA. Sensitivity, specificity, reliability, and clinical validity of provider-reported symptoms: a comparison with self-reported symptoms. Outcomes Committee of the AIDS Clinical Trials Group. J Acquir Immune Defic Syndr. 1999;21:126–33.
Raboud J, Lesosky M, Sterling S, Phillips E, Walmsley S, Bayoumi A. An estimate of the proportion of symptoms reported in self-administered questionnaires that are captured as adverse drug events in an observational database. HIV Clin Trials. 2007;8:311–9.
Briongos Figuero LS, Bachiller Luque P, Palacios Martin T, Gonzalez Sagrado M, Eiros Bouza JM. Assessment of factors influencing health-related quality of life in HIV-infected patients. HIV Med. 2011;12:22–30.
Degroote S, Vogelaers D, Vandijck DM. What determines health-related quality of life among people living with HIV: an updated review of the literature. Arch Public Health. 2014;72:40.
Justice AC, Chang CH, Rabeneck L, Zackin R. Clinical importance of provider-reported HIV symptoms compared with patient-report. Med Care. 2001;39:397–408.
Preau M, Leport C, Salmon-Ceron D, Carrieri P, Portier H, Chene G, et al. Health-related quality of life and patient-provider relationships in HIV-infected patients during the first three years after starting PI-containing antiretroviral treatment. AIDS Care. 2004;16:649–61.
Cooper V, Gellaitry G, Hankins M, Fisher M, Horne R. The influence of symptom experiences and attributions on adherence to highly active anti-retroviral therapy (HAART): a six-month prospective, follow-up study. AIDS Care. 2009;21:520–8.
Cooper V, Moyle GJ, Fisher M, Reilly G, Ewan J, Liu HC, et al. Beliefs about antiretroviral therapy, treatment adherence and quality of life in a 48-week randomised study of continuation of zidovudine/lamivudine or switch to tenofovir DF/emtricitabine, each with efavirenz. AIDS Care. 2011;23:705–13.
Ammassari A, Murri R, Pezzotti P, Trotta MP, Ravasio L, De Longis P, et al. Self-reported symptoms and medication side effects influence adherence to highly active antiretroviral therapy in persons with HIV infection. J Acquir Immune Defic Syndr. 2001;28:445–9.
Preau M, Leport C, Villes V, Michelet C, Collin F, Carrieri MP, et al. Prevalence and predictors of deterioration of a trustful patient-provider relationship among HIV-infected persons treated with antiretroviral therapy. J Acquir Immune Defic Syndr. 2008;47:467–71.
US FDA. Enhancing benefit-risk assessment in regulatory decision-making. Silver Spring: US FDA; 2013.
Giordano TP, Guzman D, Clark R, Charlebois ED, Bangsberg DR. Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clin Trials. 2004;5:74–9.
Woodcock A, Bradley C. Validation of the revised 10-item HIV Treatment Satisfaction Questionnaire status version and new change version. Value Health. 2006;9:320–33.
Justice AC, Holmes W, Gifford AL, Rabeneck L, Zackin R, Sinclair G, et al. Development and validation of a self-completed HIV symptom index. J Clin Epidemiol. 2001;54(Suppl 1):S77–90.
Mills AM, Antinori A, Clotet B, Fourie J, Herrera G, Hicks C, et al. Neurological and psychiatric tolerability of rilpivirine (TMC278) vs. efavirenz in treatment-naive, HIV-1-infected patients at 48 weeks. HIV Med. 2013;14:391–400.
Dejesus E, Young B, Morales-Ramirez JO, Sloan L, Ward DJ, Flaherty JF, et al. Simplification of antiretroviral therapy to a single-tablet regimen consisting of efavirenz, emtricitabine, and tenofovir disoproxil fumarate versus unmodified antiretroviral therapy in virologically suppressed HIV-1-infected patients. J Acquir Immune Defic Syndr. 2009;51:163–74.
Hodder SL, Mounzer K, Dejesus E, Ebrahimi R, Grimm K, Esker S, et al. Patient-reported outcomes in virologically suppressed, HIV-1-Infected subjects after switching to a simplified, single-tablet regimen of efavirenz, emtricitabine, and tenofovir DF. AIDS Patient Care STDs. 2010;24:87–96.
Simpson KN, Hanson KA, Harding G, Haider S, Tawadrous M, Khachatryan A, et al. Patient reported outcome instruments used in clinical trials of HIV-infected adults on NNRTI-based therapy: a 10-year review. Health Qual Life Outcomes. 2013;11:164.
Snyder CF, Aaronson NK. Use of patient-reported outcomes in clinical practice. Lancet. 2009;374:369–70.
Snyder CF, Aaronson NK, Choucair AK, Elliott TE, Greenhalgh J, Halyard MY, et al. Implementing patient-reported outcomes assessment in clinical practice: a review of the options and considerations. Qual Life Res. 2012;21:1305–14.
Wegzyn CM, Fredrick LM, Stubbs RO, Woodward WC, Norton M. Diarrhea associated with lopinavir/ritonavir-based therapy: results of a meta-analysis of 1469 HIV-1-infected participants. J Int Assoc Physicians AIDS Care (Chic). 2012;11:252–9.
Duracinsky M, Herrmann S, Berzins B, Armstrong AR, Kohli R, Le Coeur S, et al. The development of PROQOL-HIV: an international instrument to assess the health-related quality of life of persons living with HIV/AIDS. J Acquir Immune Defic Syndr. 2012;59:498–505.
Acknowledgments
This study and analysis was supported by Gilead Sciences, Inc. Editorial assistance was provided by Prescott Medical Communications Group, and funded by Gilead Sciences, Inc.
Conflicts of interest
Jason Brunetta has received honoraria from Abbvie Canada, Gilead Sciences Canada, Merck Canada, Janssen Canada, and ViiV Canada; Santiago Moreno Guillén has undertaken speaking activities for, and received research grants from, Abbott, Boehringer-Ingelheim, Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Janssen Cilag, Merck Sharp & Dohme, Pfizer, Roche, and Schering Plough; Barbara Wade is an investigator and speaker for Gilead Sciences; Andrea Antinori has received honoraria for consultancy with Gilead Sciences, ViiV Healthcare, Merck, Janssen-Cilag, Abbvie, and Bristol Myers Squibb, and has also received research grants from Gilead Sciences, Bristol Myers Squibb, and ViiV Healthcare; Peter Shalit has received grants/research support from Gilead Sciences, Glaxo Smithkline, Merck, Janssen, and ViiV, is a consultant for Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck, and is on the speaker’s bureau and/or has received honoraria from Bristol-Myers Squibb, Gilead Sciences, Merck, Janssen, and ViiV; Ramin Ebrahimi, Bethsheba Johnson, Ivan Walker, and Shampa De-Oertel are employees of Gilead Sciences, Inc., with ownership of Gilead stocks. Patrick Yeni and Margaret Johnson have no conflicts of interest to disclose.
Author contributions
Jason Brunetta and Santiago Moreno Guillén collected the data and created the first draft of the manuscript. Andrea Antinori, Patrick Yeni, Barbara Wade, Margaret Johnson, and Peter Shalit collected the data and critically revised the manuscript. Ramin Ebrahimi, Bethsheba Johnson, Ivan Walker, and Shampa De-Oertel were involved in the data analysis and data interpretation, and critically revised the manuscript. All authors had access to the data and approved the final version of the manuscript for submission. Jason Brunetta, the corresponding author, is the guarantor of the overall content.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
40271_2015_123_MOESM1_ESM.tif
HIV Treatment Satisfaction Questionnaire Items: Change from Baseline to Week 24. LEGEND: Post-baseline responses range from -3 (much less satisfied) to +3 (much more satisfied); see Methods. NRTI indicates a nucleoside or nucleotide analog reverse transcriptase inhibitor; PI, protease inhibitor; RTV, ritonavir; RPV/FTC/TDF, single-tablet regimen consisting of rilpivirine, emtricitabine, and tenofovir DF (TIFF 1081 kb)
40271_2015_123_MOESM2_ESM.tif
HIV Symptom Index Questionnaire: Visit-by-visit Rates, All Symptoms. LEGEND: Of the 159 patients initially treated with their baseline PI+RTV+2NRTI regimen, 152 switched to RPV/FTC/TDF at Week 24 (Delayed Switch Arm). *p<0.05, **p<0.01, ***p<0.001 for within-group comparison vs baseline (RPV/FTC/TDF, PI+RTV+2NRTIs) or vs Week 24 (Delayed Switch), using McNemar test. NRTI indicates a nucleoside or nucleotide analog reverse transcriptase inhibitor; PI, protease inhibitor; RTV, ritonavir; RPV/FTC/TDF, single-tablet regimen consisting of rilpivirine, emtricitabine, and tenofovir DF (TIFF 5000 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Brunetta, J., Moreno Guillén, S., Antinori, A. et al. Patient-Reported Outcomes After a Switch to a Single-Tablet Regimen of Rilpivirine, Emtricitabine, and Tenofovir DF in HIV-1-Positive, Virologically Suppressed Individuals: Additional Findings From a Randomized, Open-Label, 48-Week Trial. Patient 8, 257–267 (2015). https://doi.org/10.1007/s40271-015-0123-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-015-0123-2