Abstract
Background
Noncompliance to drug therapy, a common problem in geriatric patients, adversely affects disease outcomes. In India, data addressing noncompliance in elderly patients, the factors responsible for it and possible solutions for the problem are very limited.
Objective
To evaluate the prevalence of drug noncompliance among Indian geriatric patients, explore factors affecting it and examine the impact of educating patients about importance of adhering to drug therapy.
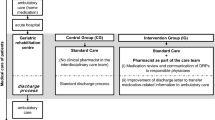
Study design
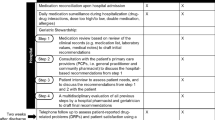
A total of 200 geriatric patients from various outpatient departments were randomly recruited. Baseline information related to diseases and drug therapy were recorded using a structured case-record form that included a questionnaire for evaluation of drug compliance. Patients were randomly divided in two groups of 100 individuals; the interventional group received education about the importance of drug compliance and related issues, and the control group did not. Changes in compliance were evaluated at a follow-up visit 7–14 days later.
Results
Noncompliance to drug therapy was reported in 77.5 % of patients, and was significantly associated with socioeconomic status, prescription-related factors (number of medicines prescribed, purchasing drugs from same pharmacy, patients’ particularity in taking medicines on time, instructions given by doctors); and drug-related factors (frequency and duration of administration, skewed instructions for use, physical difficulties in taking drugs, price of drug as perceived by patient, cost of therapy, risk of adverse drug reactions as perceived by patient). At follow-up, compliance had significantly improved in the group who had received education relative to the group who did not.
Conclusion
Educating geriatric patients about their disease and drug therapy, and the importance of compliance to therapy may improve their short-term compliance behaviour.
Similar content being viewed by others
References
World Health Organization. World health day 2012: good health adds life to years. http://www.who.int/mediacentre/news/releases/2012/whd_20120403/en/index.html. Accessed 10 Apr 2012.
Mar J, Rodriguez-Artalejo F. Which is more important for the efficiency of hypertension treatment: hypertension stage, type of drug or therapeutic compliance? J Hypertens. 2001;19(1):149–55.
Sabate E. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003.
Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–14.
Benner JS, Glynn RJ, Mogun H, et al. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288(4):455–61.
Thrall G, Lip GYH, Lane D. Medication compliance research: still so far to go. J Appl Res Clin Exp Ther. 2003;3(3):254–61.
Kulshreshtha SP. Manual for socio-economic status scale. Agra: National Psychological Corporation; 1975.
Chong CK, Chan JC, Chang S, et al. A patient compliance survey in a general medical clinic. J Clin Pharm Ther. 1997;22(5–6):323–6.
Conry M. Polypharmacy: Pandora’s medicine chest? Geriatric Times. 2000;1:1–4.
Hernández-Ronquillo L, Téllez-Zenteno JF, Garduño-Espinosa J, et al. Factors associated with therapy noncompliance in type-2 diabetes patients. Salud Publica Mex. 2003;45(3):191–7.
Stilley CS, Sereika S, Muldoon MF, et al. Psychological and cognitive function: predictors of adherence with cholesterol lowering treatment. Ann Behav Med. 2004;27(2):117–24.
Wai CT, Wong ML, Ng S, et al. Utility of the Health Belief Model in predicting compliance of screening in patients with chronic hepatitis B. Aliment Pharmacol Ther. 2005;21(10):1255–62.
Balchand K. Now, planning commission lowers the poverty line. The Hindu 2012 Mar 20. http://www.thehindu.com/news/national/article3013870.ece. Accessed 5 Nov 2012.
Cramer JA, Mattson RH, Prevey ML, et al. How often is medication taken as prescribed? A novel assessment technique. JAMA. 1989;261(22):3273–7.
Moore PJ, Sickel AE, Malat J, et al. Psychosocial factors in medical and psychological treatment avoidance: the role of the doctor-patient relationship. J Health Psychol. 2004;9(3):421–33.
Gonzalez J, Williams JW Jr, Noël PH, et al. Adherence to mental health treatment in a primary care clinic. J Am Board Fam Pract. 2005;18(2):87–96.
Lawson VL, Lyne PA, Harvey JN, et al. Understanding why people with type 1 diabetes do not attend for specialist advice: a qualitative analysis of the views of people with insulin-dependent diabetes who do not attend diabetes clinic. J Health Psychol. 2005;10(3):409–23.
Gascon JJ, Sanchez-Ortuno M, Llor B, et al. Why hypertensive patients do not comply with the treatment: results from a qualitative study. Fam Pract. 2004;21(2):125–30.
Ponnusankar S, Surulivelrajan M, Anandamoorthy N, et al. Assessment of impact of medication counseling on patients’ medication knowledge and compliance in an outpatient clinic in South India. Patient Educ Couns. 2004;54(1):55–60.
O’Donoghue MN. Compliance with antibiotics. Cutis. 2004;73(5 Suppl):30–2.
Ellis JJ, Erickson SR, Stevenson JG, et al. Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. J Gen Intern Med. 2004;19(6):638–45.
Choi-Kwon S, Kwon SU, Kim JS. Compliance with risk factor modification: early-onset versus late-onset stroke patients. Eur Neurol. 2005;54(4):204–11.
Avorn J, Monette J, Lacour A, et al. Persistence of use of lipid-lowering medications: a cross national study. JAMA. 1998;279(18):1458–62.
Hope CJ, Wu J, Tu W, et al. Association of medication adherence, knowledge, and skills with emergency department visits by adults 50 years or older with congestive heart failure. Am J Health Syst Pharm. 2004;61(19):2043–9.
Lowe CJ, Raynor DK, Purvis J, et al. Effects of a medicine review and education programme for older people in general practice. Br J Clin Pharmacol. 2000;50(2):172–5.
Acknowledgments
The authors would like to thank Dr. Gaurav Modi for his help in statistical analysis of the data.
Disclosure
No sources of funding were used to conduct this study or prepare the manuscript. The authors have no conflicts of interest that are directly relevant to the content of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, R.B., Desai, S.V., Gajjar, B.M. et al. Factors responsible for noncompliance to drug therapy in the elderly and the impact of patient education on improving compliance. Drugs Ther Perspect 29, 360–366 (2013). https://doi.org/10.1007/s40267-013-0075-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-013-0075-3