Abstract
Background
Treatment of hereditary angioedema (HAE) in ‘older adults’ (those aged ≥65 years) has not been well studied. The international Berinert Patient Registry collected data on the use of intravenous plasma-derived, pasteurized, nanofiltered C1-inhibitor concentrate (pnfC1-INH; Berinert®/CSL Behring) in patients of any age, including many older adults.
Methods
This observational registry, conducted from 2010 to 2014 at 30 US and seven European sites, gathered prospective (post-enrollment) and retrospective (pre-enrollment) usage and adverse event (AE) data on subjects treated with pnfC1-INH.
Results
The registry documented 1701 pnfC1-INH infusions in 27 older adults. A total of 1511 HAE attacks treated with pnfC1-INH administration were reported among 25 of the 27 (92.6 %) older adults. Among the older adults, mean (standard deviation [SD]) (8.8 [4.1] IU/kg) and median (6.4 IU/kg) pnfC1-INH doses were lower than those reported for 252 ‘younger adults’ (those aged <65 years: 12.9 [6.2], 12.5 IU/kg, respectively). A total of 19 AEs occurred in 8 of 23 (34.8 %) older adults with prospective data, for rates of 0.83 events per subject and 0.02 events per infusion, similar to corresponding rates in younger adults (0.91 and 0.03, respectively). None of the AEs were considered related to pnfC1-INH, and all but two events (prostatectomy, gastrointestinal bleeding) were mild or moderate in severity. Administration of pnfC1-INH outside of a healthcare setting was reported for 1609 infusions in 16 older adults, representing 94.6 % of all pnfC1-INH infusions in this age group. There were no recorded instances of difficulty with self-administration of intravenous pnfC1-INH.
Conclusions
These findings suggest a high degree of safety with intravenous pnfC1-INH use in older adults with HAE, regardless of administration setting.
Trial Registration Clinicaltrials.gov NCT01108848.
Similar content being viewed by others
Published data and treatment recommendations specific to the management of hereditary angioedema (HAE) in older patients (aged ≥65 years) are lacking. |
The Berinert Patient Registry dataset included 27 older adults with HAE who used a combined total of 1701 Berinert (plasma-derived C1-inhibitor concentrate) infusions. |
In this subset of older adults using Berinert for HAE, the rate of adverse events was low (0.02 events per infusion), and a majority of infusions (94.6 %) were administered outside of a healthcare setting, with no evidence of subjects having difficulty with home administration. |
1 Introduction
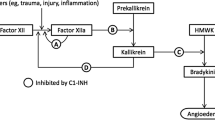
Hereditary angioedema (HAE) is a rare, autosomal dominant disorder characterized in most cases by a quantitative and/or qualitative deficiency in the C1-inhibitor (C1-INH) protein primarily due to genetic mutations [1, 2]. As C1-INH is a key regulator of inflammation, inadequate activity leads to unchecked activation of the classic complement pathway and bradykinin system with subsequent vascular leakage and angioedema. Clinically, presenting symptoms include acute non-pruritic and recurrent episodes of localized subcutaneous or submucosal swelling, often involving the extremities, upper airways, and gastrointestinal (GI) and urogenital tracts [1]. Laryngeal edema, while less frequent, poses a serious risk for asphyxiation unless properly treated [3, 4]. With the potential for high morbidity and mortality, coupled with the unpredictable nature of attacks, HAE can have a substantial effect on quality of life for patients and their families [5–8].
Although HAE is commonly diagnosed during childhood or early adulthood [9, 10], the chronic nature of the disease requires ongoing medical follow-up and treatment throughout the patient’s entire lifespan, including into old age. As treatment options for HAE have continued to improve over recent decades, it is likely that many individuals are living longer and requiring continued treatment well into later adulthood. In general, as patients age, it is not uncommon for medical needs to shift because of physiologic changes, higher rates of comorbidities, and concomitant drug use [11]. Therefore, drug therapies are often studied specifically in elderly populations to ensure safety and appropriate usage in this demographic. With regard to HAE management, current consensus guidelines do not address issues specific to older adults, and there is a gap in research regarding HAE management in this age group, including general treatment strategies and outcomes [12]. Furthermore, the current paradigm in HAE management focuses heavily on administration outside of a healthcare setting (home- or self-administration) [13–17], but the technical and medical feasibility of this approach has not yet been studied in older adult patients specifically [12].
The plasma-derived, highly-purified, pasteurized, nanofiltered C1-INH concentrate (pnfC1-INH; Berinert®/CSL Behring) is approved in the USA for the treatment of HAE attacks in patients of all ages, and in the EU for the treatment of HAE attacks and short-term prophylaxis in adults and children. To evaluate the continued safety of pnfC1-INH administration within the real-world setting, the international Berinert Patient Registry (hereafter, ‘registry’) was designed to gather data on pnfC1-IHN treatment across all age groups [18]. The final registry dataset included a sufficient number of subjects aged ≥65 years (hereafter, ‘older adults’) to allow for analysis of usage patterns and safety in this population. This report presents findings from the registry pertaining to older adult subjects.
2 Methods
2.1 Study Design
This multicenter observational patient registry (NCT01108848) was conducted between 2010 and 2014 at 30 sites in the USA and seven sites in Europe (five in Germany, one in Denmark, one in Switzerland). Retrospective (pnfC1-INH infusions given prior to registry enrollment) and prospective (pnfC1-INH infusions given after registry enrollment) data were captured by medical chart review in accordance with local regulatory requirements pertaining to non-interventional studies. All subjects provided informed consent for the collection of treatment data prior to enrollment, allowing data to be gathered willingly without impact on treatment decisions or a patient’s choice to use pnfC1-INH. The study protocol and master informed consent form were reviewed and approved by relevant institutional review boards and institutional ethics committees. Subject information was anonymized, and project staff adhered to procedures to ensure the confidentiality of all data as required by the guidelines of the International Conference on Harmonization [19].
2.2 Subjects
Subjects enrolled in the registry included individuals of any age who used pnfC1-INH for any reason, irrespective of regionally approved product indication.
2.3 Data Collection
Both retrospective and prospective data on pnfC1-INH use among enrolled subjects were obtained through chart review. Subject data were documented in the subjects’ medical records by study site personnel and transferred to an electronic case report form (eCRF) for remote storage and monitoring. The following data were collected: patient demographics, reason for pnfC1-INH administration (on demand, prophylaxis, or other), pnfC1-INH dose, setting of administration (healthcare facility or outside of a healthcare facility), concomitant medications, attack characteristics (e.g., anatomic location, severity, potential triggers), and adverse events (AEs). HAE attack data were collected only for attacks treated with pnfC1-INH. Data about the use of C1-INH products other than Berinert were not collected, nor were data collected on attacks that were untreated or were treated with products other than Berinert. Treatment outside of a healthcare setting included any pnfC1-INH infusion administered by the subject, a family member, friend, or other caregiver in a non-healthcare setting (e.g., home). Treatment in a healthcare setting included any pnfC1-INH infusion administered by a healthcare professional (e.g., a physician or nurse) within a healthcare institution (e.g., hospital or clinic).
AEs experienced by subjects within a 30-day period following treatment with pnfC1-INH were recorded regardless of suspected causality to pnfC1-INH administration. For each AE, investigators evaluated causality to pnfC1-INH treatment based on clinical judgment and graded AE intensity as mild (easily tolerated, no interference with daily activities), moderate (causing some interference with daily activities), or severe (incapacitating; unable to work or perform usual activities). AEs resulting in death, life-threatening circumstances, hospitalization, or persistent or significant disability or incapacity were pre-defined as serious AEs (SAEs). Investigators engaged in subject follow-up for all AEs until symptom resolution was achieved or the condition was deemed chronic. Monitoring for suspected viral transmissions was done per usual clinical practice, in which investigators tested for viral transmission based upon their medical judgment and local standard of medical care.
2.4 Data Analysis
Data were summarized using descriptive statistics, and select outcomes were compared with findings from adult subjects aged 17 to <65 years (hereafter, ‘younger adults’). Thromboembolic events (TEEs) were classified according to the criteria of the Medical Dictionary for Regulatory Activities (MedDRA) queries for embolic and thrombotic events. HAE attacks and HAE attack signs and symptoms were not recorded as AEs unless the attack also met SAE criteria (e.g., hospitalization). These were then dually reported as both SAEs and HAE attacks. AEs reported without an intensity grading were conservatively categorized as ‘severe’ and included in both ‘severe’ and ‘missing’ groupings on data tables. Events with missing causality were categorized by convention as ‘related’. No efficacy analyses were performed for acute HAE therapy. Prophylaxis findings for the entire study population are to be reported separately.
3 Results
The registry enrolled 318 subjects who received at least one pnfC1-INH dose. Of these, 27 (8.5 %) were aged ≥65 years (all White; mean [standard deviation (SD)] age 70.5 [4.9] years, and predominantly from European sites) (Table 1). Among older adult subjects, the registry captured 1701 pnfC1-INH infusions, which form the basis of this report. A majority of the older adults (n = 25, 92.6 %) used pnfC1-INH for treatment of HAE attacks (12 exclusively for this reason); 13 (48.1 %) used pnfC1-INH for both attack treatment and prophylaxis, and two (7.4 %) used pnfC1-INH for prophylaxis only and had no pnfC1-INH-treated attacks recorded in the registry (Table 2). Of the 1701 pnfC1-INH infusions, 841 (49.4 %) were recorded prospectively and 860 (50.6 %) were recorded retrospectively. Of the 27 older adults, 21 (77.8 %) were using a variety of concomitant medications (Table 3).
3.1 Characteristics of Hereditary Angioedema (HAE) Attacks
A total of 1511 pnfC1-INH-treated HAE attacks were recorded among 25 of the 27 (92.6 %) older adult registry subjects. The number of attacks per subject (treated with pnfC1-INH) ranged from 0 to 610. The majority of attacks (88.0 %) occurred in the absence of an apparent trigger and were categorized as spontaneous in origin. HAE attack patterns by anatomic location were generally similar between older adult subjects and the 252 younger adult registry subjects, who experienced 9575 pnfC1-INH-treated attacks (Fig. 1). With regard to anatomic location, abdominal attacks were the most common among the older adults, accounting for 33.8 % of all reported attacks and occurring in 72.0 % of the older adults. A majority (88.0 %) of the older adults experienced at least one attack that was categorized as severe, although severe attacks were a small proportion of all reported attacks (86 of 1511; 5.7 %) (Fig. 2).
Hereditary angioedema attack* patterns by anatomic location for subjects aged ≥65 years compared with those for subjects aged 17 to <65 years. a Percentage of subjects experiencing at least one attack per anatomic location. Percentages are based on the number of subjects with at least one attack. Subjects were included only one time for each anatomic location for which they experienced at least one attack. Anatomic location data were missing for seven subjects aged ≥65 years and 54 subjects aged 17 to <65 years. b Percentage of all reported attacks* by anatomic location. Anatomic location data were missing for 589 (39.0 %) of attacks in subjects aged ≥65 years and 1211 (12.6 %) of attacks in subjects aged 17 to <65 years. *Only attacks treated with pnfC1-INH (Berinert). HAE hereditary angioedema
Severity of hereditary angioedema attacks*. a Per subject (highest intensity reported) and b per attack among subjects aged ≥65 years compared with subjects aged 17 to <65 years. a Per subject†, highest intensity reported. Attack density ratings were not available in three (1.2 %) subjects aged 17 to <65 years. b Severity distribution of all recorded attacks*. Attack intensity ratings were not available for 280 (18.5 %) of attacks in subjects aged ≥65 years and 1267 (13.2 %) of attacks in subjects aged 17 to <65 years. *Only attacks treated with pnfC1-INH (Berinert). †For per subject reporting of attack intensity, each subject is included in only one category based on the maximum intensity attack
3.2 pnfC1-INH Usage and Dosing
A majority of all pnfC1-INH infusions in older adult registry subjects (1511 of 1701; 88.8 %) were administered for on-demand treatment of HAE attacks (Table 2). The number of pnfC1-INH infusions per subject exhibited substantial variability, ranging from 1 to 612. Among the older adults, mean [SD] (8.8 [4.1] IU/kg) and median (6.4 IU/kg) pnfC1-INH doses were lower than those reported for the younger adults (12.9 [6.2] and 12.5 IU/kg, respectively) (Table 4) and were also the lowest of any age group in the registry [18].
The majority of pnfC1-INH infusions in the older adults (94.7 %; 1611 of 1701) were recorded at European study sites. Mean weight-based doses for the 20 European subjects ranged from 5.9 to 20.3 IU/kg; the mean of the subject means was 12.0 IU/kg. For the seven US subjects, mean doses per subject ranged from 15.6 to 22.0 IU/kg (mean of the subject means 19.4 IU/kg).
3.3 Administration Setting
Ten (37 %) older adults had all of their pnfC1-INH infusions administered in a healthcare setting; 11 (40.7 %) had all infusions outside of a healthcare setting; five (18.5 %) had infusions administered both in healthcare settings and outside of a healthcare setting; and the setting was unknown for one subject. Overall, a majority (94.6 %) of all pnfC1-INH infusions in the older adults were given outside of a healthcare setting and 4.4 % were given within a healthcare setting (setting not recorded for 1.0 % of infusions).
Of particular interest were instances in which pnfC1-INH was administered outside of a healthcare setting (e.g., home) with a subsequent infusion(s) given in a healthcare setting; the reasons for the change in setting were evaluated whenever possible, with an interest in whether there were issues relating to difficulty with self-infusion. Five older adults had one or more such changes in administration setting, most of which appeared to be related to patient preference or already being at a medical facility when the infusion was required. There were no recorded instances of difficulty with pnfC1-INH infusion being the reason for switching back to administration in a healthcare setting, although reasons were not recorded in all cases.
3.4 Safety
In the entire registry, no AEs were identified in retrospective data; therefore, the safety analysis was based on prospectively recorded infusions only (841 infusions in 23 older adults). A total of 19 AEs were reported in 8 of 23 (34.8 %) subjects with prospective infusion data, for an overall rate of 0.83 events per subject and 0.02 events per pnfC1-INH infusion. The majority (n = 13 [68.4 %]) of AEs were categorized as mild in intensity, and no AEs were considered related to pnfC1-INH administration. These rates were similar to AE rates reported for younger adults (0.91 per subject; 0.03 per infusion). Four SAEs were reported in four older adults (prostatectomy; urinary tract infection requiring hospitalization; fat embolism; and GI bleeding), though none were considered related to treatment with pnfC1-INH. There were no reports of hypersensitivity, anaphylaxis, or events consistent with anaphylaxis. In accordance with the observational nature of the registry, viral testing would have been conducted only if considered necessary by the treating physician. There were no reports of testing for blood-borne viral infection conducted on any subject beyond baseline.
4 Discussion
Despite the lifelong nature of HAE and the growing number of individuals aged ≥65 years entering the healthcare system [20, 21], few published data are available on the treatment of HAE among patients ≥65 years [12]. Research focused specifically on the older adult population is important given that medical needs can differ from those of younger adults [11]. By generating a considerable volume of real-world data on the use of pnfC1-INH to treat HAE in 27 older adults through 1701 pnfC1-INH infusions, the findings from the Berinert Registry can help fill this knowledge gap. To our knowledge, the registry data described here are the first to specifically evaluate HAE attack characteristics and pnfC1-INH usage in patients aged ≥65 years.
In examining HAE attack patterns and characteristics, registry data for the older adult population generally paralleled those found among younger adults, with abdominal attacks reported most frequently. Abdominal attacks in the older adult population may be of particular interest, as other GI events that may present as an acute abdomen (e.g., diverticulitis, intestinal perforation) tend to occur more frequently in older individuals. Given the greater risk for anesthesia in this population, the differential diagnosis, inclusive of an abdominal HAE attack, is important. Fewer older adults reported ever having experienced a laryngeal attack. This may reflect a self-selection bias of this population, given the absence of effective, readily available HAE treatments decades ago and an ensuing higher likelihood of death from laryngeal attacks during younger years in this group. No triggering event was indicated for the majority of attacks in older adults. Previous research has identified similar attack patterns in general [22–25], although the data reflected in the registry are limited to attacks treated with pnfC1-INH. While at least one severe attack was experienced by a majority (88.0 %) of older adults, mild attacks constituted the largest percentage of all documented attacks experienced within the older adult population.
Even in the absence of regulatory approval of pnfC1-INH for prophylactic treatment in the USA, half of older adult registry subjects used pnfC1-INH for this purpose, and two subjects received pnfC1-INH infusions exclusively for prophylaxis. These findings are not unexpected in light of consensus guidelines that recommend C1-INH for long- or short-term prophylaxis [1, 13, 14, 26, 27] and clinical data that support such use [28–38].
Current dosing recommendations for pnfC1-INH suggest a dose of 20 IU/kg, regardless of patient age [39]. Prior to the current registry analysis, no known research has described pnfC1-INH dosing in older adults. Among older adult subjects in the registry, mean (8.8 IU/kg) and median (6.4 IU/kg) weight-based pnfC1-INH doses were notably lower than the recommended dose and also lower than the mean and median weight-based doses reported for 252 younger adults in the registry (12.9 and 12.5 IU/kg, respectively). Dosing patterns by geographic location identified a trend of lower mean weight-based pnfC1-INH doses for subjects in Europe relative to those in the USA, a pattern that was also demonstrated for the entire registry population, regardless of subject age [18]. Given that the older adult subgroup was skewed heavily toward European subjects, this presents another contributing factor to the relatively low mean pnfC1-INH doses observed in this subgroup as a whole.
Drug dosing in older adults is often approached conservatively given age-related physiologic changes that can influence the pharmacokinetics and pharmacodynamics of drug therapy [11, 40–43]. Physical changes related to normal aging can be further complicated by the tendency of older adults to manifest comorbid medical conditions requiring concomitant therapy, as reflected by the majority of subjects in this study who were using a variety of medications along with pnfC1-INH. While there is no reason to suspect altered disposition of a naturally occurring therapeutic protein such as pnfC1-INH, the lower mean doses reflected in this subset of registry patients overall may reflect, at least in part, general attitudes about drug usage and conservative dosing strategies in older adults. These findings may also reveal consequences of long-term experience with pnfC1-INH and personalized dosage tailoring in these older patients, especially in European markets where Berinert has been marketed for several decades. Older adults are more likely to be retired and possibly have less stress and more time to focus on managing their disease.
Recent HAE consensus guidelines stress individualization of therapy [13, 14, 27, 44, 45]. The variation in dosing noted in the registry subjects seems to support an apparent lack of ‘one dose fits all’ mindset, regardless of the specific reasons for the lower doses reflected in this older adult subset. While attack treatment efficacy data were not captured as part of the registry, given this real-world setting for pnfC1-INH, it could be assumed that dosing was being tailored in these patients to maintain a satisfactory level of benefit.
Considering the possibly higher-risk status of older adults for drug-related problems due to the aforementioned age-related conditions, determining the safety of real-world use of pnfC1-INH in older patients is of particular interest, and data from the registry confirm the overall safety of pnfC1-INH within this population. Since retrospective data are not a reliable source of safety information, safety analyses in all age groups of the registry were conducted for prospectively recorded events only. In the older adult subgroup, the share of such data was 49.4 % (841 of 1701) of all recorded infusions in 23 of 25 older adults, which still constitutes a sizeable dataset. The observed AE rates for older adult registry subjects were very low, both as events per infusion and as events per subject, and were similar to corresponding rates noted in younger adults in the registry. None of the events were considered related to pnfC1-INH, and there were no reports of TEEs, hypersensitivity, or anaphylaxis. Viral transmission was not prospectively assessed, but there was no evidence that any patient was evaluated for suspected blood-borne viral illness during the registry. As previously noted, the majority of older adults were also receiving concomitant medications during the time of pnfC1-INH administration, thus highlighting safe use even in the presence of multiple concomitant therapies.
Regarding setting of pnfC1-INH administration, recent HAE expert guidelines consistently recommend training and equipping patients for self- or home-based administration of HAE medications, with treatment outside of a healthcare setting providing more timely symptom relief, mitigation of attack severity, lower healthcare costs, and improved quality of life [8, 46–49]. For older adults, age-related changes in physical or mental capacity and the presence of medical comorbidities could be deterrents to self-administration of intravenous medication. Research has implicated several conditions, including osteoarthritis, vision difficulties, and cognitive impairment, that may negatively affect the elderly population’s self-management of various at-home therapies [12, 43, 50]. However, the registry findings support the safety and feasibility of pnfC1-INH administration outside of a healthcare setting in older adults with HAE. The vast majority (94.6 %) of infusions in older adult registry subjects were administered outside of the healthcare setting, and in 11 of the 27 older adult subjects, all pnfC1-INH administration occurred in a non-healthcare setting. Almost all pnfC1-INH infusions administered outside of a healthcare setting in older adults were reported as self-infusion; one infusion in one subject was documented as given by a caregiver.
Subjects within the group receiving pnfC1-INH outside of the healthcare setting had a wide range of number of infusions (from 1 to 612), suggesting achievability of self-administration regardless of attack frequency. This substantiates research identifying the skill of self-infusion as a long-term competency in patients with HAE, and time between attacks should not exclude patients from the option of self-administration [49]. While four older adults experienced at least one change in infusion setting from non-healthcare setting to healthcare setting, there were no recorded instances of difficulty with pnfC1-INH infusion being the reason for any of these instances. The rates of AEs remained low regardless of treatment setting and corroborate reports indicating the high safety profile of pnfC1-INH administration outside of a healthcare setting [51, 52]. While every patient should be assessed individually before being considered a candidate for home-based HAE treatment, the registry findings support the supposition that age itself should not preclude the option of self-managed intravenous pnfC1-INH therapy. Numerous studies have noted a marked increase in overall health and treatment adherence when care is patient driven [16, 41–43, 49, 50, 53]. During a stage of life when independence is often threatened, the autonomy derived from medication self-administration can foster a sense of control in older adults, thereby improving morale and quality of life.
The data from this registry analysis are subject to several limitations. Inherent to the observational nature of the study, there was no control group (other than younger age groups) and no governance over pnfC1-INH usage or dosing patterns, all of which were determined by the treating physicians according to local standards of care. As such, patterns of individual usage varied widely, including the number of infusions per subject. Data were limited by what was gathered by the treating physician, and AEs for retrospective infusions were not reported. Furthermore, only HAE attacks treated with pnfC1-INH were recorded. The generalizability of the findings is limited by the racial homogeneity of the population, the relatively small sample size (although sizable for a rare disease subgroup), voluntary nature of participation. Finally, the nature of the registry data precluded analysis of attack treatment efficacy.
5 Conclusions
These registry data support the safe use of pnfC1-INH in older adults with HAE, with very low rates of AEs similar to rates reported in younger adults in the registry, and none considered related to treatment. Weight-based dosing of pnfC1-INH was notably lower for older than for younger adults, the reasons for which are unknown, nor was the registry designed to evaluate efficacy ramifications of these lower doses. The registry data support the safety and feasibility of pnfC1-INH administration outside of a healthcare setting in older adults and document widespread implementation of such practice in this demographic subgroup.
References
Cicardi M, Aberer W, Banerji A, Bas M, Bernstein JA, Bork K, et al. Classification, diagnosis, and approach to treatment for angioedema: consensus report from the Hereditary Angioedema International Working Group. Allergy. 2014;69:602–16.
Cugno M, Zanichelli A, Foieni F, Caccia S, Cicardi M. C1-inhibitor deficiency and angioedema: molecular mechanisms and clinical progress. Trends Mol Med. 2009;15(2):69–78.
Bork K, Hardt J, Schicketanz KH, Ressel N. Clinical studies of sudden upper airway obstruction in patients with hereditary angioedema due to C1 esterase inhibitor deficiency. Arch Intern Med. 2003;163:1229–35.
Bork K, Hardt J, Witzke G. Fatal laryngeal attacks and mortality in hereditary angioedema due to C1-INH deficiency. J Allergy Clin Immunol. 2012;130:692–7.
Lumry WR, Castaldo AJ, Vernon MK, Blaustein MB, Wilson DA, Horn PT. The humanistic burden of hereditary angioedema: Impact on health-related quality of life, productivity, and depression. Allergy Asthma Proc. 2010;31(5):407–14.
Fouche AS, Saunders EFH, Craig T. Depression and anxiety in patients with hereditary angioedema. Ann Allergy Asthma Immunol. 2014;112(4):371–5.
Bewtra AK, Levy RJ, Jacobson KW, Wasserman RL, Machnig T, Craig TJ. C1-inhibitor therapy for hereditary angioedema attacks: Prospective patient assessments of health-related quality of life. Allergy Asthma Proc. 2012;33(5):427–31.
Bygum A, Aygören-Pürsün E, Beusterien K, Hautamaki E, Sisic Z, Wait S, et al. Burden of illness in hereditary angioedema: A conceptual model. Acta Derm Venereol. 2015;95(6):706–10.
Nanda MK, Elenburg S, Bernstein JA, Assa’ad AH. Clinical features of pediatric hereditary angioedema. J Allergy Clin Immunol Pract. 2015;3(3):392–5.
Zanichelli A, Magerl M, Longhurst H, Fabien V, Maurer M. Hereditary angioedema with C1 inhibitor deficiency: delay in diagnosis in Europe. Allergy Asthma Clin Immunol. 2013;9(1):29.
Vinks THAM, Egberts TCG, de Lange TM, de Koning FHP. Pharmacist-based medication review reduces potential drug-related problems in the elderly: The SMOG controlled trial. Drugs Aging. 2009;26(2):123–33.
Kuhlen JL, Banerji A. Hereditary angioedema: Special consideration in children, women of childbearing age, and the elderly. Allergy Asthma Proc. 2015;36(6):425–32.
Cicardi M, Bork K, Caballero T, Craig T, Li HH, Longhurst H, et al. Evidence-based recommendations for the therapeutic management of angioedema owing to hereditary C1 inhibitor deficiency: consensus report of an International Working Group. Allergy. 2012;67:147–57.
Craig TJ, Pürsün EA, Bork K, Bowen T, Boysen H, Farkas H, et al. WAO guideline for the management of hereditary angioedema. World Allergy Organ J. 2012;5:182–99.
Cicardi M, Craig TJ, Martinez-Saguer I, Hebert J, Longhurst HJ. Review of recent guidelines and consensus statements on hereditary angioedema therapy with focus on self-administration. Int Arch Allergy Immunol. 2013;161(1):3–9.
Wang A, Fouche A, Craig TJ. Patients perception of self-administrated medication in the treatment of hereditary angioedema. Ann Allergy Asthma Immunol. 2015;115(2):120–5.
Longhurst HJ, Farkas H, Craig T, Aygoren-Pursun E, Bethune C, Bjorkander J, et al. HAE international home therapy consensus document. Allergy Asthma Clin Immunol. 2010;6(1):22.
Riedl M, Bygum A, Lumry W, et al. Safety and Usage of C1-esterase Inhibitor in Hereditary Angioedema: Berinert Registry Data. J Allergy Clin Immunol Pract. 2016;4(5):963–71.
International Council for Harmonisation (ICH). Guidance for Industry. E6 Good Clinical Practice: Consolidated Guidance. 1996. Available at: http://www.ich.org/products/guidelines/efficacy/efficacy-single/article/good-clinical-practice.html. Accessed 14 Sept 2016.
Roehr B. US geriatric mental health workforce needs to expand, says Institute of Medicine. BMJ. 2012;345:e4686.
Rich PB, Adams SD. Health care: Economic impact of caring for geriatric patients. Surg Clin North Am. 2015;95(1):11–21.
Craig TJ, Bewtra AK, Bahna SL, Hurewitz D, Schneider LC, Levy RJ, et al. C1 esterase inhibitor concentrate in 1085 Hereditary Angioedema attacks—final results of the I.M.P.A.C.T.2 study. Allergy. 2011;66(12):1604–11.
Tachidjian R, Banerji A, Guyer A, Morphew T. Current characteristics associated with hereditary angioedema attacks and treatment: the home infusion based patient experience. Allergy Asthma Proc. 2015;36(2):151–9.
Bork K, Meng G, Staubach P, Hardt J. Hereditary angioedema: new findings concerning symptoms, affected organs, and course. Am J Med. 2006;119:267–74.
Bork K, Staubach P, Eckardt AJ, Hardt J. Symptoms, course, and complications of abdominal attacks in hereditary angioedema due to C1 inhibitor deficiency. Am J Gastroenterol. 2006;101:619–27.
Lang DM, Aberer W, Bernstein JA, Chng HH, Grumach AS, Hide M, et al. International consensus on hereditary and acquired angioedema. Ann Allergy Asthma Immunol. 2012;109:395–402.
Zuraw BL, Banerji A, Bernstein JA, Busse PJ, Christiansen SC, Davis-Lorton M, et al. US hereditary angioedema association medical advisory board 2013 recommendations for the management of hereditary angioedema due to C1 inhibitor deficiency. J Allergy Clin Immunol Pract. 2013;1:458–67.
Pedrosa M, Lobera T, Panizo C, Jurado J, Caballero T. Long-term prophylaxis with C1-inhibitor concentrate in patients with hereditary angioedema. J Investig Allergol Clin Immunol. 2014;24:271–3.
Farkas H, Jakab L, Temesszentandrási G, Visy B, Harmat G, Füst G, et al. Hereditary angioedema: a decade of human C1-inhibitor concentrate therapy. J Allergy Clin Immunol. 2007;120(4):941–7.
Czaller I, Visy B, Csuka D, Fust G, Toth F, Farkas H. The natural history of hereditary angioedema and the impact of treatment with human C1-inhibitor concentrate during pregnancy: a long-term survey. Eur J Obstet Gynecol Reprod Biol. 2010;152(1):44–9.
Bork K, Hardt J. Hereditary angioedema: long-term treatment with one or more injections of C1 inhibitor concentrate per week. Int Arch Allergy Immunol. 2011;154(1):81–8.
Helsing P, Nielsen EW. Hepatocellular focal nodular hyperplasia after danazol treatment for hereditary angio-oedema. Acta Derm Venereol. 2006;86(3):272–3.
Hermans C. Successful management with C1-inhibitor concentrate of hereditary angioedema attacks during two successive pregnancies: A case report. Arch Gynecol Obstet. 2007;276(3):271–6.
Gorman P. Hereditary angioedema and pregnancy: a successful outcome using C1 esterase inhibitor concentrate. Can Fam Physician. 2008;54(3):365–6.
Tallroth GA. Long-term prophylaxis of hereditary angioedema with a pasteurized C1 inhibitor concentrate. Int Arch Allergy Immunol. 2011;154(4):356–9.
Gower R, Aygören-Pürsün E, Davis-Lorton M, Hurewitz D, Johnston D. Hereditary angioedema caused by C1-esterase inhibitor deficiency: a literature-based analysis and clinical commentary on prophylaxis treatment strategies. World Allergy Organ J. 2011;4(2 Suppl):S9–21.
Farkas H, Zotter Z, Csuka D, Szabo E, Nebenfuhrer Z, Temesszentandrasi G, et al. Short-term prophylaxis in hereditary angioedema due to deficiency of the C1-inhibitor—a long-term survey. Allergy. 2012;67(12):1586–93.
Roldán Sevilla T, González Fernández MA, Roldán Rincón A, Herrero Ambrosio A. The use of C1 esterase inhibitor in long term prophylaxis of recurrent acute hereditary angioedema exacerbated by tamoxifen. Aten Farm. 2013;15(2):124–7.
Berinert (human C1-esterase inhibitor [human]) Prescribing information. Marburg: CSL Behring; 2011.
Mangoni AA, Jackson SHD. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharamcol. 2004;57:6–14.
Lam P, Elliott RA, George J. Impact of a self-administration of medications programme on elderly inpatients’ competence to manage medications: a pilot study. J Clin Pharm Ther. 2011;36(1):80–6.
Nützel A, Dahlhaus A, Fuchs A, Gensichen J, Konig HH, Riedel-Heller S, et al. Self-rated health in multimorbid older general practice patients: a cross-sectional study in Germany. BMC Fam Pract. 2014;15:1.
Westerbotn M, Fahlström E, Fastbom J, Agüero-Torres H, Hillerås P. How do people experience their management of medicines? J Clin Nurs. 2008;17(5A):106–15.
Betschel S, Badiou J, Binkley K, Hebert J, Kanani A, Keith P, et al. Canadian hereditary angioedema guideline. Allergy Asthma Clin Immunol. 2014;10:50.
Longhurst HJ, Tarzi MD, Ashworth F, Bethune C, Cale C, Dempster J, et al. C1 inhibitor deficiency: 2014 United Kingdom consensus document. Clin Exp Immunol. 2015;180:475–83.
Aygören-Pürsün E, Martinez-Saguer I, Rusicke E, Klingebiel T, Kreuz W. On demand treatment and home therapy of hereditary angioedema in Germany—the Frankfurt experience. Allergy Asthma Clin Immunol. 2010;6:21.
Maurer M, Aberer W, Bouillet L, Caballero T, Fabien V, Kanny G, et al. Hereditary angioedema attacks resolve faster and are shorter after early icatibant treatment. PLoS One. 2013;8(2):e53773.
Tourangeau LM, Castaldo AJ, Davis DK, Kozoil J, Christensen SC, Zuraw BL. Safety and efficacy of physician-supervised self-managed C1 inhibitor replacement therapy. Int Arch Allergy Immunol. 2012;157:417–24.
Boysen HB, Bouillet L, Aygren-Pursun E. Challenges of C1-inhibitor concentrate self-administration. Int Arch Allergy Immunol. 2013;161:21–5.
Marek KD, Stetzer F, Ryan PA, Bub LD, Adams SJ, Schlidt A, et al. Nurse care coordination and technology effects on health status of frail older adults via enhanced self-management of medication: randomized clinical trial to test efficacy. Nurs Res. 2013;62(4):269–78.
Bygum A, Andersen KE, Mikkelsen CS. Self-administration of intravenous C1-inhibitor therapy for hereditary angioedema and associated quality of life benefits. Eur J Dermatol. 2009;19:147–51.
Kreuz W, Rusicke E, Martinez-Saguer I, Aygören-Pürsün E, Heller C, Klingebiel T. Home therapy with intravenous human C1-inhibitor in children and adolescents with hereditary angioedema. Transfusion. 2012;52:100–7.
Stretton CM, Latham NK, Carter KN, Lee AC, Anderson CS. Determinants of physical health in frail older people: the importance of self-efficacy. Clin Rehabil. 2006;20(4):357–66.
Acknowledgments
Editorial assistance was provided by Rachel Greenfield, RN, of Churchill Communications (Maplewood, NJ). This assistance was funded by CSL Behring (Marburg, Germany). The authors retained full control over manuscript content.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
This study was funded by CSL Behring.
Disclosures
Dr. Anette Bygum has received consulting fees and travel expenses from CSL Behring and Shire; grants and writing assistance from CSL Behring; fees for participation in reviews and speaker fees as a chairperson for Shire; she has taken an unpaid part in educational events with SOBI; and has provided unpaid writing assistance for ViroPharma. Dr. Inmaculada Martinez-Saguer has received consultancy fees and fees for participation in reviews from CSL Behring, Shire, Sobi, BioCryst, and Pharming. Dr. Murat Bas has received grants, consulting fees, honorarium, and travel support from CSL Behring. Dr. Jeffrey Rosch has no conflicts to disclose. Drs Jonathan Edelman and Mikhail Rojavin are employees at CSL Behring. Dr. Debora Williams-Herman was an employee of CSL Behring at the time of study conduct.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bygum, A., Martinez-Saguer, I., Bas, M. et al. Use of a C1 Inhibitor Concentrate in Adults ≥65 Years of Age with Hereditary Angioedema: Findings from the International Berinert® (C1-INH) Registry. Drugs Aging 33, 819–827 (2016). https://doi.org/10.1007/s40266-016-0403-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-016-0403-0