Abstract
Background and objectives
Colesevelam significantly lowers cholesterol in patients with hypercholesterolemia, and both cholesterol and hemoglobin A1C (A1C) in patients with type 2 diabetes mellitus (T2DM). The purpose of this post hoc analysis was to evaluate the efficacy and safety/tolerability of colesevelam in older (≥65 years) and younger (<65 years) adults.
Methods
We conducted post hoc analyses of pooled clinical trial data from seven phase II and III randomized, double-blind, placebo-controlled, primary hyperlipidemia and T2DM clinical trials. The hyperlipidemia safety/tolerability analysis included seven studies (≥65 years, n = 154; <65 years, n = 381); the efficacy analysis utilized one study with sufficient patients in both age groups for meaningful comparison. The T2DM analyses included four studies (safety/tolerability: ≥65 years, n = 249; <65 years, n = 880) or three studies (efficacy). In the hyperlipidemia studies, patients received colesevelam 1.5–4.5 g/day or placebo, alone or with a statin, for 4 weeks to 6 months. In the T2DM studies, colesevelam 3.75 g/day or placebo was added to existing antidiabetes therapies for 16 or 26 weeks. Low-density lipoprotein cholesterol (LDL-C), A1C, and adverse events were assessed.
Results
In the hyperlipidemia analysis, colesevelam versus placebo produced similar mean reductions from baseline in LDL-C in older (−16.6 vs. +0.5 %) and younger (−13.7 vs. +0.4 %) patients. In the T2DM analysis, older and younger patients had similar reductions from baseline in A1C (treatment difference −0.59 and −0.54 %, respectively; both p < 0.001) and LDL-C (−14.7 and −15.5 %, respectively; both p < 0.001) with colesevelam. In both analyses, adverse event incidence was generally similar between subgroups. In the T2DM analysis, hypoglycemia was slightly more frequent with colesevelam versus placebo in older patients (5.8 vs. 2.3 %); no reports of hypoglycemia were considered serious adverse events.
Conclusions
In primary hyperlipidemia and in T2DM, colesevelam appeared to be generally as safe, well tolerated, and efficacious in patients aged ≥65 years as in those aged <65 years.
Similar content being viewed by others
1 Background and Objectives
The population in the USA aged ≥65 years has a disproportionately high prevalence of dyslipidemia (65–74 years, 37.1 %; 75–84 years, 37.7 %) [1] and diabetes mellitus (26.9 %) [2], both of which are risk factors for cardiovascular disease [3]. Achieving recommended treatment targets for hypercholesterolemia and diabetes can be difficult with lifestyle modification alone, and typically requires pharmacological therapy [4–6]. It is important to note that although clinical practice guidelines have historically focused on achieving specific low-density lipoprotein cholesterol (LDL-C) targets to reduce cardiovascular disease risk, the recently published American College of Cardiology/American Heart Association guidelines have instead placed the emphasis on reducing risk in patient groups known to be at a high risk for cardiovascular disease, and using the appropriate intensity of statin therapy to reduce risk. The optimal LDL-C goal has remained the same; however, the clinical focus has shifted to who can most benefit from statin therapy as well as using higher-dose statins instead of a low-dose statin combined with a cholesterol-lowering agent from another drug class. These guidelines represent a change in the historical treatment paradigm that is still being debated and is discussed in more detail below [7].
Standard and intensive doses of statins are effective in reducing LDL-C levels [8]. However, for patients who are unable to tolerate maximal doses of statins, or who do not achieve treatment targets with such therapy, combination therapy with statins may be necessary. The Lipid Treatment Assessment Project found that National Cholesterol Education Program LDL-C targets were achieved by 40 % of patients receiving statin monotherapy overall and 18 % of those with coronary heart disease (CHD) [5]. Add-on therapies can enhance the cardiovascular benefits; each mmol/L (39 mg/dL) reduction in LDL-C has been shown to be associated with a 19 % reduction in coronary mortality and a 21 % reduction in risk of any major vascular event (p < 0.001 for both) [9].
Similarly, an analysis of National Health and Nutrition Examination Survey data (excluding patients likely to have type 1 diabetes) showed that in 2003–2006, hemoglobin A1C (A1C) <7.0 % was achieved by 57 % of patients overall (64 % of those aged ≥60 years) [10]. There is a progressive requirement for multiple therapies to achieve glycemic control in patients with type 2 diabetes mellitus (T2DM) [11]. Nevertheless, each 1 % reduction in A1C has been shown to be associated with a 21 % reduction in risk for deaths related to diabetes and a 14 % reduction in risk for myocardial infarction (p < 0.001 for both) [12].
Drug safety is an important consideration in the treatment of elderly patients. Indeed, this is among the leading considerations driving the current consensus around the requirement for individualization of treatment for older patients with T2DM who have a longer duration of disease or more complicated disease [13]. Furthermore, in the USA, the expanding population aged ≥65 years is included in the Medicare population, and it is important in the current climate to show that drugs are safe and efficacious in this population. Although numerous pharmacological options are available for lipid and glycemic control, special care must be taken in prescribing for elderly patients, who may be more susceptible to adverse effects due to age-related changes in pharmacokinetics and pharmacodynamics [14, 15]. The risk of muscle-related adverse effects associated with 3-hydroxy-3-methyl-glutaryl-CoA reductase inhibitors (statins), which are considered first-line lipid-lowering therapy, appears to increase with increasing age [16].
In a study examining hospitalizations for adverse drug events among the elderly population in the USA, two-thirds of hospitalizations were attributable to four drugs or drug classes (alone or in combination); two of these drugs/drug classes were diabetes treatments (insulins 13.9 %; oral antidiabetes drugs 10.7 %) [17]. Drug-induced hypoglycemia is an important consideration for antidiabetes therapies, particularly sulfonylureas [14]. Elderly patients with T2DM are at increased risk of hypoglycemia compared with younger patients [18], leading to increased risk for falls [19] and fall-related fractures [20]. In addition, elderly patients with T2DM display unawareness of hypoglycemia relative to middle-aged patients, which may contribute to an increased risk of developing severe hypoglycemia [21]. Thiazolidinediones are associated with adverse effects that may limit their use in elderly patients [15]; these include edema and potential congestive heart failure, and fractures [14, 22–24].
Colesevelam hydrochloride is a bile acid sequestrant that was designed to have a high affinity and capacity to bind bile acids. It is unabsorbed by the body and its distribution is confined to the digestive tract. Colesevelam binds to bile acids in the intestine, and these complexes are excreted in the feces [25], thereby decreasing the bile acid pool. Correspondingly, there is an increased conversion of cholesterol to bile acids that results in a compensatory uptake of LDL-C by the liver from the blood, which ultimately decreases serum LDL-C. The glucose-lowering mechanism of colesevelam is not completely understood; however, it is believed that its binding to bile acids activates a G-protein-coupled receptor for bile acids that results in increased secretion of GLP-1, and perhaps other incretins, which inhibits hepatic glycogenolysis [26–28]. Colesevelam is approved by the US FDA as an adjunct to diet and exercise for the reduction of LDL-C in adults with primary hyperlipidemia (Fredrickson Type IIa) or in boys and postmenarchal girls (aged 10–17 years) with heterozygous familial hypercholesterolemia, as monotherapy or in combination with a statin, and also for improvement of glycemic control in adults with T2DM in combination with oral antidiabetes drugs and insulin [29]. In double-blind placebo-controlled trials in patients with moderate hypercholesterolemia, colesevelam was shown to be effective in lowering LDL-C levels (13–21 % reduction vs. placebo) and was generally well tolerated [25, 30, 31], with less constipating effect than other bile acid sequestrants [30]. In adults with T2DM inadequately controlled by sulfonylurea-, metformin-, or insulin-based therapy, the addition of colesevelam significantly reduced A1C (−0.5 % reduction vs. placebo) and LDL-C levels (13–17 % reduction vs. placebo) and was generally well tolerated in three double-blind, placebo-controlled, parallel-group, multicenter studies [32–34].
Although the safety and efficacy of colesevelam have been well documented in the general population, its safety and efficacy have been less extensively evaluated in older patients. Here, we report the results of post hoc integrated analyses of pooled clinical trial data conducted to evaluate the efficacy and safety/tolerability of colesevelam in older adults (men and women aged ≥65 years) as well as younger adults aged <65 years.
2 Methods
2.1 Primary Hyperlipidemia Analysis
This was a post hoc analysis of the pooled data from patients with hyperlipidemia (N = 1,350) included in seven phase II and III randomized, double-blind, placebo-controlled clinical studies designed to establish the safety and efficacy of colesevelam as a monotherapy or in combination with a statin (lovastatin, simvastatin, or atorvastatin). The studies enrolled patients aged ≥18 years with primary hypercholesterolemia. Patients received colesevelam 1.5–4.5 g/day or placebo for durations ranging from 4 weeks to 6 months. The demographic characteristics of the treatment categories (placebo, colesevelam only, colesevelam/statin, statin only) and colesevelam dose groups (placebo, low, medium, high) created from the integrated database were very similar, with the single exception of duration of exposure. Due to a low number of older patients in the hyperlipidemia studies, no formal statistical analysis had been performed in these studies.
2.1.1 Efficacy
A pivotal 6-month phase III dose-ranging study that demonstrated the long-term safety and efficacy of colesevelam monotherapy in a larger patient population was sufficiently large enough for analysis of drug–demographic efficacy interactions. This study included 133 patients aged <65 years (colesevelam, n = 68; placebo, n = 65) and 50 patients aged ≥65 years (colesevelam, n = 27; placebo, n = 23). Efficacy parameters included mean percent changes from baseline to study end in LDL-C and triglyceride levels.
2.1.2 Safety
The safety and tolerability analysis included data from all seven studies. These studies included 381 patients aged <65 years (colesevelam, n = 289; placebo, n = 92) and 154 patients aged ≥65 years (colesevelam, n = 117; placebo, n = 37). Safety and tolerability were evaluated on the basis of adverse events (AEs).
2.2 Integrated Type 2 Diabetes Mellitus (T2DM) Analysis
2.2.1 Efficacy
This was a post hoc analysis of the pooled data from all patients (N = 1,018) included in three double-blind, placebo-controlled, pivotal trials of colesevelam as add-on therapy for patients with T2DM inadequately controlled with metformin-, insulin-, or sulfonylurea-based therapy [32–34]. The studies enrolled patients aged 18–75 years with T2DM who had A1C values of 7.5–9.5 %. In all three trials, colesevelam (3.75 g/day) or placebo was added on to patients’ established antidiabetes therapies for 16 weeks (insulin-based therapy study) or 26 weeks (metformin- and sulfonylurea-based therapy studies). The studies included a total of 790 patients aged <65 years (colesevelam, n = 402; placebo, n = 388) and 228 patients aged ≥65 years (colesevelam, n = 110; placebo, n = 118). Efficacy parameters included mean change in A1C and fasting plasma glucose (FPG), and mean percent changes in LDL-C, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), non-HDL-C, triglyceride, apolipoprotein (apo) A-I, and apo B, from baseline to study end.
2.2.2 Safety
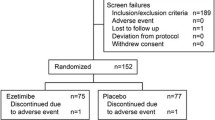
The safety analysis included pooled data from the same three pivotal trials [32–34], plus those from a small randomized, double-blind, placebo-controlled pilot study that included patients inadequately controlled on metformin and/or sulfonylureas [35]. Thus, this safety/tolerability pooled analysis included a total of 249 patients aged ≥65 years (colesevelam, n = 121; placebo, n = 128) and 880 patients aged <65 years (colesevelam, n = 446; placebo, n = 434). One subject aged <65 years was randomized to colesevelam but did not take the study medication and therefore was not included in the safety analysis. Safety and tolerability were evaluated on the basis of AEs.
2.3 Ethical Standards
All clinical studies were conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. The protocol and informed consent documents at each site were approved by an Institutional Review Board. All subjects provided informed consent prior to entering any of the studies.
3 Results
3.1 Integrated Primary Hyperlipidemia Analysis
3.1.1 Efficacy
Colesevelam monotherapy resulted in similar mean reductions from baseline in LDL-C levels compared with placebo in both patients aged ≥65 years (−16.6 % [n = 27] vs. +0.5 % [n = 23]) and those aged <65 years (−13.7 % [n = 68] vs. +0.4 % [n = 65]). These changes in LDL-C were accompanied by a similar modest increase from baseline in levels of triglyceride with colesevelam compared with placebo in both patients aged ≥65 years (+13.4 % [n = 27] vs. +2.9 % [n = 23]) and those aged <65 years (+12.7 % [n = 68] vs. +3.1 % [n = 65]).
3.1.2 Safety
Colesevelam therapy was generally well tolerated in the primary hyperlipidemia studies. The most common AEs were gastrointestinal, including constipation and dyspepsia (Table 1); the incidence of these AEs was similar in both age subgroups.
3.2 Integrated T2DM Analysis
3.2.1 Efficacy
In patients aged ≥65 years as well as those aged <65 years, colesevelam treatment added to existing therapies resulted in similar reductions from baseline in A1C (Fig. 1a) and FPG (Fig. 1b). Adding colesevelam to existing therapies also resulted in similar reductions from baseline in LDL-C and non-HDL-C and similar increases in triglycerides in both age subgroups (Fig. 2). Both older and younger patients also had similar reductions from baseline in apo B (data not shown) and increases in apo A-I (data not shown) with colesevelam, while no significant changes in HDL-C levels (Fig. 2) were seen with colesevelam treatment in either age subgroup.
Mean changes from baseline in LDL-C, non-HDL-C, and HDL-C and median change from baseline in TG in the integrated type 2 diabetes mellitus analysis, by age subgroup. Asterisk indicates that the parameter is not normally distributed so median values are reported. The interquartile range values for patients aged <65 years and ≥65 years were 37.1 and 35.1, respectively. HDL-C high-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol, TG triglyceride
3.2.2 Safety
Overall, treatment with colesevelam was safe and generally well tolerated. The overall incidence of AEs was slightly higher with colesevelam than with placebo in both age subgroups, with slightly lower values overall in patients aged <65 years (Table 2). Serious AE incidence rates in patients aged ≥65 years were lower with colesevelam than with placebo and similar to those in patients aged <65 years. Maximum treatment-emergent AE severity was mild-to-moderate in the majority of patients in both treatment groups among both age groups. The rate of withdrawals due to AEs was relatively low overall, but slightly higher with colesevelam, compared with placebo, among both patients aged ≥65 years (8.3 vs. 6.3 %) and those aged <65 years (6.3 vs. 2.3 %), and again slightly lower in the younger subgroup.
In both age subgroups, the incidence of constipation was higher with colesevelam than with placebo (Table 2). However, the imbalance between treatment groups was less pronounced in patients aged ≥65 years, despite the higher overall incidence of constipation in this subgroup. In both age subgroups, the incidence of diarrhea was lower with colesevelam than with placebo. Dyspepsia was less frequent in patients aged ≥65 years and similar between treatments. Although hypoglycemia was slightly more frequent with colesevelam than with placebo among patients aged ≥65 years, but not those aged <65 years, no episode of hypoglycemia was considered a serious AE.
It should be noted that the study was not powered to detect statistically significant differences in the incidence of specific AEs between the age cohorts and, therefore, no statistical analysis was performed.
4 Discussion
In these integrated analyses, the safety and tolerability profile of colesevelam was generally similar in older patients compared with younger patients. Certain gastrointestinal AEs were slightly more common with colesevelam than with placebo; however, AEs were generally mild-to-moderate and did not often result in drug discontinuation. In addition, colesevelam was effective in lowering LDL-C in patients with primary hyperlipidemia aged ≥65 years; these beneficial effects were similar to those observed in patients aged <65 years. Furthermore, colesevelam was an efficacious add-on treatment for improving both glycemic control and lipid management in adults with T2DM on various antidiabetes regimens; the effects of colesevelam on diabetic and lipid parameters were consistent in patients aged <65 and ≥65 years when added to existing antidiabetes therapies. The results from the integrated T2DM study analysis showed that colesevelam had a minimal impact on HDL-C levels, i.e., patients aged <65 years had an insignificant decrease whereas those ≥65 years had an insignificant increase in HDL-C levels. This is consistent with existing data showing that colesevelam typically has a neutral effect on, or may slightly increase, HDL-C levels [29, 36].
The selection of pharmacological therapies for older patients requires special care and consideration [15]. In particular, older patients may be more susceptible to adverse effects [14], potentially limiting the ability to use certain drugs, or use of higher doses. For example, the incidence of myotoxicity associated with statin therapy appears to increase with increasing age [16], and is also higher with intensive-dose statin therapy [37]. The prevalence of diabetes increases with age, and therefore the use of drugs with potential diabetogenic effects in the elderly population is of concern. Niacin has been associated with modest adverse effects on glycemic control [38], and statin therapy (particularly intensive-dose) has been associated with concerns regarding increased risk of developing diabetes [39–41]. It has been suggested that the cardiovascular benefits of statins outweigh any negative glycemic effects [42]; however, it may be prudent to avoid any potential increased risk of diabetes in the elderly population. This constitutes yet another consideration for combination or alternative therapies. Colesevelam achieves additive LDL-C reductions of approximately 16 % when used in combination with statins [43].
Constipation is common in the elderly population [44]; therefore, the incidence of constipation as an AE may be of particular relevance when treating elderly patients. In the current analyses, while the incidence of constipation was higher with colesevelam than with placebo, as has previously been observed, it was notable that the imbalance between the colesevelam and placebo groups was less pronounced among the older patients, despite the overall incidence of constipation being higher in the older group. Interestingly, in the integrated T2DM analysis, the incidence of diarrhea was lower with colesevelam than with placebo among both age groups. This finding may have been influenced by patients who had study medication added to a regimen that included metformin, which is well known to be associated with the development of diarrhea [45]. The gastrointestinal effects of metformin, together with weight loss effects, may even be detrimental to frail elderly patients [14]. Hypothetically, the slightly constipating effects of colesevelam may have somewhat counteracted the diarrhea-inducing effects of metformin, reducing the incidence of diarrhea in the colesevelam group. A similar reduction in diarrhea was seen with colesevelam versus placebo as add-on therapy to metformin in patients with early T2DM in a previous study [46].
Although tight glycemic control is beneficial in reducing the risk of diabetic complications in patients with T2DM, as shown in the UK Prospective Diabetes Study [12], avoidance of hypoglycemia is especially important, particularly for elderly patients who may be at increased risk of hypoglycemia [18], which can lead to falls and fall-related fractures [19, 20]. Compared with other oral antidiabetes agents, sulfonylureas and repaglinide are associated with a greater risk of hypoglycemia in adults with T2DM [47]. A consensus panel convened by the American Diabetes Association recommends that glyburide, which has the highest risk of hypoglycemia among the sulfonylureas, should not be prescribed to older patients [14]. In the current integrated T2DM analysis, the incidence of hypoglycemia was similar with colesevelam and placebo among patients aged <65 years, and was only slightly higher with colesevelam among patients aged ≥65 years. This increase in hypoglycemia in the older subgroup may have reflected the higher propensity for hypoglycemia in older patients [18]. Nevertheless, the rates of hypoglycemia remained considerably lower than those reported with other classes of drugs, such as sulfonylureas (up to 36 %) [47].
Age-specific hypoglycemic data were not analyzed for each of the antidiabetic agent T2DM studies individually; however, the following data are reported in the literature for the colesevelam and placebo total population cohorts to provide a relative assessment of the incidence of hypoglycemia associated with the individual antidiabetic agents in combination with colesevelam. No significant changes in the incidence of hypoglycemia were noted in the small T2DM pilot study wherein colesevelam was added to sulfonylurea and/or metformin [35]. Colesevelam as add-on therapy to metformin-based therapy [32] reported one patient in the colesevelam group experienced mild hypoglycemia. Colesevelam as add-on therapy to insulin-based therapy [34] had a reported incidence of hypoglycemia in the colesevelam versus placebo group of 3.4 and 5.7 %, respectively, and colesevelam as add-on therapy to sulfonylurea-based therapy [33] reported six patients experienced hypoglycemia versus two patients in the placebo group. No patient discontinued from any of the studies due to hypoglycemia.
One should keep in mind that both renal and hepatic functions diminish with advancing age, requiring consideration in the selection of pharmacological agents in elderly patients [48]. For example, pharmacokinetic studies of metformin in healthy elderly subjects indicate that plasma clearance is decreased, half-life is prolonged, and peak plasma concentration is increased, due primarily to likely changes in renal function associated with aging [49]. Another important consideration is the frequent use of polypharmacy among elderly adults and the possibility of drug interactions and altered pharmacokinetics that may result [50]. Because bile acid sequestrants are not absorbed, they do not cause many of the systemic toxicities that may occur with other classes of lipid-lowering drugs [51]. In addition, colesevelam has been shown to have a low propensity for drug–drug interactions [29, 52–55]. Where an interaction is apparent with a concomitant medication, the effect can typically be avoided by administration of colesevelam 4 h after the other drug [29].
Our analyses showed a modest increase in triglyceride levels with colesevelam, the clinical significance of which remains unclear. Elevated triglyceride levels seem to be a synergistic risk factor for CHD rather than an independent risk factor [56]. In the Lipid Research Clinics Program trial, the risk for CHD was decreased with the reduction of LDL-C even when there was a concurrent modest elevation in triglycerides [57, 58]. However, a prospective cohort study of an elderly outpatient population showed that a triglyceride level >200 mg/dL was a significant risk factor for cardiovascular events, irrespective of the presence of hypertension, abdominal obesity, or diabetes [59]. Confounding the issue even further, the CASTEL (CArdiovascular STudy in the ELderly) study by Mazza et al. [60] showed that a high triglyceride level was an independent predictor of CHD mortality in elderly women but did not have a predictive role in men. Consequently, additional studies will be needed before a definitive statement can be made regarding the role of triglycerides as a coronary risk factor in older patients [60]. Presently, we believe the modest triglyceride increase of 15 % in the present study should be interpreted in conjunction with the benefit of colesevelam therapy in reducing LDL-C, non-HDL-C, and apo B levels [61].
The 2013 American College of Cardiology/American Heart Association guidelines [7] were published recently; although it was beyond the scope of this study to review these guidelines, it is noteworthy that they focus on reducing atherosclerotic cardiovascular disease risk (ASCVD) and recommend high- and moderate-intensity statin therapy for use in secondary and primary prevention. These guidelines also recommend using the appropriate intensity of statin therapy to reduce ASCVD risk in patients most likely to benefit from such treatment. The guidelines use the intensity of statin therapy as the goal of treatment instead of LDL-C or non-HDL-C targets. As such, non-statin cholesterol-lowering agents can be added if the maximum tolerated intensity of statin treatment results in a less-than-anticipated therapeutic response in patients at higher ASCVD risk. However, it is currently unclear as to how these new guidelines will affect the historical use of non-statin lipid-lowering agents used either as monotherapy or in combination with a statin.
A potential limitation of this study is that the number of older patients evaluated in the hyperlipidemia analyses was relatively small; however, it should be noted that it had a sufficient number of patients to perform statistical analyses. A limitation of the study is that the age range of patients making up the older patient cohort in the integrated T2DM analyses was 65–75 years; consequently, it is not known whether the safety and efficacy findings would also be applicable to patients aged >75 years. Therefore, caution should be used in extrapolating the data to age groups beyond those evaluated. In addition, the primary hyperlipidemia analysis only included patients who had primary hypercholesterolemia, and the integrated T2DM analysis only included patients with T2DM; thus, the findings from these individual analyses cannot be extrapolated to patients having other types of lipid disorders, metabolic disorders, or both hyperlipidemia and T2DM. Another limitation is that although there are data showing that a bile acid sequestrant can reduce the risk of cardiovascular events [58], there have not been any randomized clinical trials assessing the effect of colesevelam in improving cardiovascular outcomes/reducing cardiovascular events. Thus, it is currently unknown whether the significant improvement in both the lipid profile and the glycemic control observed with colesevelam administration translates into a reduction in cardiovascular risk in either cohort evaluated. Finally, the data reported in this study were obtained from post hoc analyses of previously conducted pooled analyses rather than performing a meta-analysis of the evaluated colesevelam studies, which would have been more robust statistically. As such, some statistical analyses could not be performed.
5 Conclusions
Among both patients with primary hyperlipidemia and patients with T2DM, colesevelam appeared to be generally as safe and well tolerated in patients aged ≥65 years as in those aged <65 years. In patients aged ≥65 years, colesevelam had similar efficacy to that seen in patients aged <65 years both for lowering LDL-C levels among patients with primary hypercholesterolemia and for lowering A1C and LDL-C levels among patients with T2DM.
References
Goff DC Jr, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, et al. Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation. 2006;113(5):647–56. doi:10.1161/CIRCULATIONAHA.105.552737.
Centers for Disease Control and Prevention. 2011 National Diabetes Fact Sheet. 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011pdf. Accessed 4 Dec 2013.
McDonald M, Hertz RP, Unger AN, Lustik MB. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A Biol Sci Med Sci. 2009. doi:10.1093/gerona/gln016.
Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Pearson TA, Laurora I, Chu H, Kafonek S. The lipid treatment assessment project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000;160:459–67.
American Diabetes Association. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008. doi:10.2337/dc08-S061.
Stone NJ, Robinson J, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA Guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013. doi:10.1161/01.cir.0000437738.63853.7a.
Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004. doi:10.1056/NEJMoa040583.
Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005. doi:10.1016/S0140-6736(05)67394-1.
Cheung BMY, Ong KL, Cherny SS, Sham P-C, Tso AWK, Lam KSL. Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. Am J Med. 2009. doi:10.1016/j.amjmed.2008.09.047.
Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA. 1999;281:2005–12.
Stratton IM, Adler AI, Neil HAW, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–12.
Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012. doi:10.2337/dc12-0413.
Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, et al. Diabetes in older adults. Diabetes Care. 2012. doi:10.2337/dc12-1801.
American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013. doi:10.2337/dc13-S011.
El-Salem K, Ababneh B, Rudnicki S, Malkawi A, Alrefai A, Khader Y, et al. Prevalence and risk factors of muscle complications secondary to statins. Muscle Nerve. 2011. doi:10.1002/mus.22205.
Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011. doi:10.1056/NEJMsa1103053.
Bramlage P, Gitt AK, Binz C, Krekler M, Deeg E, Tschöpe D. Oral antidiabetic treatment in type-2 diabetes in the elderly: balancing the need for glucose control and the risk of hypoglycemia. Cardiovasc Diabetol. 2012. doi:10.1186/1475-2840-11-122.
Signorovitch JE, Macaulay D, Diener M, Yan Y, Wu EQ, Gruenberger J-B, et al. Hypoglycaemia and accident risk in people with type 2 diabetes mellitus treated with non-insulin antidiabetes drugs. Diabetes Obes Metab. 2013. doi:10.1111/dom.12031.
Johnston SS, Conner C, Aagren M, Ruiz K, Bouchard J. Association between hypoglycaemic events and fall-related fractures in Medicare-covered patients with type 2 diabetes. Diabetes Obes Metab. 2012. doi:10.1111/j.1463-1326.2012.01583.x.
Bremer JP, Jauch-Chara K, Hallschmid M, Schmid S, Schultes B. Hypoglycemia unawareness in older compared with middle-aged patients with type 2 diabetes. Diabetes Care. 2009. doi:10.2337/dc09-0114.
Lago RM, Singh PP, Nesto RW. Congestive heart failure and cardiovascular death in patients with prediabetes and type 2 diabetes given thiazolidinediones: a meta-analysis of randomised clinical trials. Lancet. 2007. doi:10.1016/S0140-6736(07)61514-1.
Colhoun HM, Livingstone SJ, Looker HC, Morris AD, Wild SH, Lindsay RS, et al. Hospitalised hip fracture risk with rosiglitazone and pioglitazone use compared with other glucose-lowering drugs. Diabetologia. 2012. doi:10.1007/s00125-012-2668-0.
Takeda Pharmaceuticals America, Inc. Pioglitazone prescribing information. 2013. http://www.takeda.us/products/. Accessed Nov 2013.
Bays H, Dujovne C. Colesevelam HCl: a non-systemic lipid-altering drug. Expert Opin Pharmacother. 2003. doi:10.1517/14656566.4.5.779.
Beysen C, Murphy EJ, Deines K, Chan M, Tsang E, Glass A, et al. Effect of bile acid sequestrants on glucose metabolism, hepatic de novo lipogenesis, and cholesterol and bile acid kinetics in type 2 diabetes: a randomised controlled study. Diabetologia. 2012. doi:10.1007/s00125-011-2382-3.
Smushkin G, Sathananthan M, Piccinini F, Dalla Man C, Law JH, Cobelli C et al. The effect of a bile acid sequestrant on glucose metabolism in subjects with type 2 diabetes. Diabetes. 2013. doi:10.2337/db12-0923.
Katsuma S, Hirasawa A, Tsujimoto G. Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem Biophys Res Commun. 2005. doi:10.1016/j.bbrc.2005.01.139.
Daiichi Sankyo Inc. WELCHOL (colesevelam hydrochloride) US prescribing information. 2014. http://dsi.com/prescribing_information-portlet/getDocument?product=WC&inline=true. Accessed 02 Feb 2014.
Davidson MH, Dillon MA, Gordon B, Jones P, Samuels J, Weiss S, et al. Colesevelam hydrochloride (Cholestagel): a new, potent bile acid sequestrant associated with a low incidence of gastrointestinal side effects. Arch Intern Med. 1999;159:1893–900.
Insull W Jr, Toth P, Mullican W, Hunninghake D, Burke S, Donovan JM, et al. Effectiveness of colesevelam hydrochloride in decreasing LDL cholesterol in patients with primary hypercholesterolemia: a 24-week randomized controlled trial. Mayo Clin Proc. 2001. doi:10.4065/76.10.971.
Bays HE, Goldberg RB, Truitt KE, Jones MR. Colesevelam hydrochloride therapy in patients with type 2 diabetes mellitus treated with metformin: glucose and lipid effects. Arch Intern Med. 2008. doi:10.1001/archinte.168.18.1975.
Fonseca VA, Rosenstock J, Wang AC, Truitt KE, Jones MR. Colesevelam HCl improves glycemic control and reduces LDL cholesterol in patients with inadequately controlled type 2 diabetes on sulfonylurea-based therapy. Diabetes Care. 2008. doi:10.2337/dc08-0283.
Goldberg RB, Fonseca VA, Truitt KE, Jones MR. Efficacy and safety of colesevelam in patients with type 2 diabetes mellitus and inadequate glycemic control receiving insulin-based therapy. Arch Intern Med. 2008. doi:10.1001/archinte.168.14.1531.
Zieve FJ, Kalin MF, Schwartz SL, Jones MR, Bailey WL. Results of the glucose-lowering effect of WelChol study (GLOWS): a randomized, double-blind, placebo-controlled pilot study evaluating the effect of colesevelam hydrochloride on glycemic control in subjects with type 2 diabetes. Clin Ther. 2007. doi:10.1016/j.clinthera.2007.01.003.
Insull W Jr. Clinical utility of bile acid sequestrants in the treatment of dyslipidemia: a scientific review. South Med J. 2006;99:257–73.
Study of the Effectiveness of Additional Reductions in Cholesterol Homocysteine (SEARCH) Collaborative Group. Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12 064 survivors of myocardial infarction: a double-blind randomised trial. Lancet. 2010. doi:10.1016/S0140-6736(10)60310-8.
Elam MB, Hunninghake DB, Davis KB, Garg R, Johnson C, Egan D, et al. Effect of niacin on lipid and lipoprotein levels and glycemic control in patients with diabetes and peripheral arterial disease: the ADMIT study: a randomized trial. JAMA. 2000;284:1263–70.
Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, de Craen AJ, et al. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet. 2010. doi:10.1016/S0140-6736(09)61965-6.
Zaharan NL, Williams D, Bennett K. Statins and risk of treated incident diabetes in a primary care population. Br J Clin Pharmacol. 2013. doi:10.1111/j.1365-2125.2012.04403.x.
Preiss D, Seshasai SR, Welsh P, Murphy SA, Ho JE, Waters DD, et al. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA. 2011. doi:10.1001/jama.2011.860.
Ridker PM, Pradhan A, MacFadyen JG, Libby P, Glynn RJ. Cardiovascular benefits and diabetes risks of statin therapy in primary prevention: an analysis from the JUPITER trial. Lancet. 2012. doi:10.1016/S0140-6736(12)61190-8.
Bays HE, Davidson M, Jones MR, Abby SL. Effects of colesevelam hydrochloride on low-density lipoprotein cholesterol and high-sensitivity C-reactive protein when added to statins in patients with hypercholesterolemia. Am J Cardiol. 2006. doi:10.1016/j.amjcard.2005.11.039.
Talley NJ, Fleming KC, Evans JM, O’Keefe EA, Weaver AL, Zinsmeister AR, et al. Constipation in an elderly community: a study of prevalence and potential risk factors. Am J Gastroenterol. 1996;91:19–25.
Saenz A, Fernandez-Esteban I, Mataix A, Segura MA, Roqué i Figuls M, Moher D. Metformin monotherapy for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005. doi:10.1002/14651858.CD002966.pub3.
Rosenstock J, Fonseca VA, Garvey WT, Goldberg RB, Handelsman Y, Abby SL, et al. Initial combination therapy with metformin and colesevelam for achievement of glycemic and lipid goals in early type 2 diabetes. Endocr Pract. 2010. doi:10.4158/EP10130.OR.
Bolen S, Feldman L, Vassy J, Wilson L, Yeh HC, Marinopoulos S, et al. Systematic review: comparative effectiveness and safety of oral medications for type 2 diabetes mellitus. Ann Intern Med. 2007;147:386–99.
Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004;57:6–14.
Bristol-Myers Squibb Company. GLUCOPHAGE XR (metformin hydrochloride) extended-release tablets—US prescribing information. 2009. http://packageinserts.bms.com/pi/pi_glucophage.pdf. Accessed 02 Feb 2014.
Neumiller JJ, Setter SM. Pharmacologic management of the older patient with type 2 diabetes mellitus. Am J Geriatr Pharmacother. 2009. doi:10.1016/j.amjopharm.2009.12.002.
Rubenfire M, Coletti AT, Mosca L. Treatment strategies for management of serum lipids: lessons learned from lipid metabolism, recent clinical trials, and experience with the HMG CoA reductase inhibitors. Prog Cardiovasc Dis. 1998;41:95–116.
Donovan JM, Stypinski D, Stiles MR, Olson TA, Burke SK. Drug interactions with colesevelam hydrochloride, a novel, potent lipid-lowering agent. Cardiovasc Drugs Ther. 2000;14:681–90.
Donovan JM, Kisicki JC, Stiles MR, Tracewell WG, Burke SK. Effect of colesevelam on lovastatin pharmacokinetics. Ann Pharmacother. 2002;36:392–7.
Jones MR, Baker BA, Mathew P. Effect of colesevelam HCl on single-dose fenofibrate pharmacokinetics. Clin Pharmacokinet. 2004;43:943–50.
Brown KS, Armstrong IC, Wang A, Walker JR, Noveck RJ, Swearingen D, et al. Effect of the bile acid sequestrant colesevelam on the pharmacokinetics of pioglitazone, repaglinide, estrogen estradiol, norethindrone, levothyroxine, and glyburide. J Clin Pharmacol. 2010. doi:10.1177/0091270009349378.
Gotto AM Jr. Triglyceride as a risk factor for coronary artery disease. Am J Cardiol. 1998;82:22Q–25Q.
Lipid Research Clinics Program. The Lipid Research Clinics Coronary Primary Prevention Trial results. II. The relationship of reduction in incidence of coronary heart disease to cholesterol lowering. JAMA. 1984;251:365–74.
Lipid Research Clinics Program. The Lipid Research Clinics Coronary Primary Prevention Trial results. I. Reduction in incidence of coronary heart disease. JAMA. 1984;251:351–64.
Cabrera MA, de Andrade SM, Mesas AE. A prospective study of risk factors for cardiovascular events among the elderly. Clin Interv Aging. 2012. doi:10.2147/CIA.S37211.
Mazza A, Tikhonoff V, Schiavon L, Casiglia E. Triglycerides + high-density-lipoprotein-cholesterol dyslipidaemia, a coronary risk factor in elderly women: the CArdiovascular STudy in the ELderly. Intern Med J. 2005. doi:10.1111/j.1445-5994.2005.00940.x.
Jialal I, Abby SL, Misir S, Nagendran S. Concomitant reduction in low-density lipoprotein cholesterol and glycated hemoglobin with colesevelam hydrochloride in patients with type 2 diabetes: a pooled analysis. Metab Syndr Relat Disord. 2009. doi:10.1089/met.2009.0007.
Acknowledgments
Jacqueline Lanoix, PhD, Alan J. Klopp, PhD, and Sushma Soni of inScience Communications, Springer Healthcare, provided medical writing support funded by Daiichi Sankyo, Inc.
Conflict of interest
Dr. Gavin has served as a consultant to Daiichi Sankyo, Inc. Drs. Ford and Truitt are employees of Daiichi Sankyo, Inc. Dr. Jones was previously employed by Daiichi Sankyo, Inc.
Author contributions
As lead author, James R. Gavin, III was involved in interpretation of the data and was responsible for overall manuscript preparation, inclusive of the findings from the lipid studies and the type 2 diabetes studies. Michael R. Jones was involved in interpretation of the data and manuscript preparation for the lipid studies and all aspects of the diabetes studies. Daniel M. Ford had responsibility for oversight of recruitment and conduct of the type 2 diabetes studies, as well as assurance of integrity of the data and analysis for those studies. He also had input to the practical aspects of protocol design for some of those studies. Kenneth E. Truitt was involved in overseeing study design and conduct, and the interpretation of data. All authors were involved in manuscript review and revision.
Sponsor’s role
The sponsor funded and conducted the clinical trials, as well as data acquisition and analysis. Drs. Ford and Truitt are employees of Daiichi Sankyo, Inc., and Dr. Jones was previously employed by Daiichi Sankyo, Inc.
Funding
The studies and analyses were supported by Daiichi Sankyo, Inc.
Meeting presentation
The type 2 diabetes data were previously presented at the 10th Annual World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease, Los Angeles, CA, 1–3 November 2012.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Gavin, J.R., Jones, M.R., Ford, D.M. et al. Safety and Efficacy of Colesevelam HCl in the Treatment of Elderly Patients. Drugs Aging 31, 461–470 (2014). https://doi.org/10.1007/s40266-014-0174-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-014-0174-4