Abstract
Background
Statins are one of the most common medications for stroke prevention. Increasing evidence indicates that the effect of statins against stroke may depend on the optimal adherence of the patients to the long-term therapies. However, the magnitude of the association between statin adherence and the risk of stroke has not been determined.
Objective
We conducted a dose-response meta-analysis to investigate the association between statin adherence and the risk of stroke.
Methods
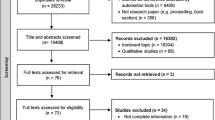
The Medline and Embase databases were systematically searched to identify relevant observational studies that evaluated the association between statin adherence and stroke risk. Statin adherence was primarily quantified by the proportion of days covered by prescribed statins. Studies in which relative risks (RRs) with 95% confidence intervals (CIs) for the association between statin adherence and stroke risk were reported or could be estimated were included in this meta-analysis.
Results
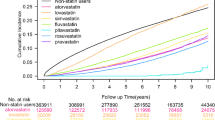
A total of 15 studies with 710,504 participants were included. The pooled RR of total stroke for the categories with the highest compared with the lowest adherence to statins was 0.72 (95% CI 0.65–0.79). Stratified by stroke subtype, the pooled RR for ischemic stroke (IS) was 0.83 (95% CI 0.74–0.92) and for hemorrhagic stroke was 0.75 (95% CI 0.51–1.09). The dose-response analysis indicated that an improvement in statin adherence of 20% was associated with an 8% lower risk of total stroke (RR 0.92; 95% CI 0.89–0.94). In the subgroup analysis for IS, an improvement in statin adherence of 20% was associated with a 7% lower risk of IS (RR 0.93; 95% CI 0.88–0.99).
Conclusion
Improved adherence to statins was associated with a lower risk of stroke, particularly of IS.




Similar content being viewed by others
References
Chroinin DN, Asplund K, Asberg S, Callaly E, Cuadrado-Godia E, et al. Statin therapy and outcome after ischemic stroke: systematic review and meta-analysis of observational studies and randomized trials. Stroke. 2013;44(2):448–56.
Sikora Newsome A, Casciere BC, Jordan JD, Rhoney DH, Sullivan KA, Morbitzer KA, Moore JD, Durr EA. The role of statin therapy in hemorrhagic stroke. Pharmacotherapy. 2015;35(12):1152–63.
Giannopoulos S, Katsanos AH, Tsivgoulis G, Marshall RS. Statins and cerebral hemodynamics. J Cereb Blood Flow Metab. 2012;32(11):1973–6.
Dowlatshahi D, Demchuk AM, Fang J, Kapral MK, Sharma M, Smith EE. Association of statins and statin discontinuation with poor outcome and survival after intracerebral hemorrhage. Stroke. 2012;43(6):1518–23.
Sett AK, Robinson TG, Mistri AK. Current status of statin therapy for stroke prevention. Expert Rev Cardiovasc Ther. 2011;9(10):1305–14.
Rannanheimo PK, Tiittanen P, Hartikainen J, Helin-Salmivaara A, Huupponen R, Vahtera J, Korhonen MJ. Impact of statin adherence on cardiovascular morbidity and all-cause mortality in the primary prevention of cardiovascular disease: a population-based cohort study in Finland. Value Health. 2015;18(6):896–905.
Chowdhury R, Khan H, Heydon E, Shroufi A, Fahimi S, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34(38):2940–8.
Lavikainen P, Helin-Salmivaara A, Eerola M, Fang G, Hartikainen J, Huupponen R, Korhonen MJ. Statin adherence and risk of acute cardiovascular events among women: a cohort study accounting for time-dependent confounding affected by previous adherence. BMJ Open. 2016;6(6):e011306.
Herttua K, Martikainen P, Batty GD, Kivimaki M. Poor adherence to statin and antihypertensive therapies as risk factors for fatal stroke. J Am Coll Cardiol. 2016;67(13):1507–15.
Chen PS, Cheng CL, Kao Yang YH, Li YH. Statin adherence after ischemic stroke or transient ischemic attack is associated with clinical outcome. Circ J. 2016;80(3):731–7.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705.
Gomez Sandoval YH, Braganza MV, Daskalopoulou SS. Statin discontinuation in high-risk patients: a systematic review of the evidence. Curr Pharm Des. 2011;17(33):3669–89.
Korhonen MJ, Ruokoniemi P, Ilomaki J, Meretoja A, Helin-Salmivaara A, Huupponen R. Adherence to statin therapy and the incidence of ischemic stroke in patients with diabetes. Pharmacoepidemiol Drug Saf. 2016;25(2):161–9.
Bijlsma MJ, Janssen F, Hak E. Estimating time-varying drug adherence using electronic records: extending the proportion of days covered (PDC) method. Pharmacoepidemiol Drug Saf. 2016;25(3):325–32.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Thompson SG, Higgins JP. How should meta-regression analyses be undertaken and interpreted? Stat Med. 2002;21(11):1559–73.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–292.
Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135(11):1301–9.
Berlin JA, Longnecker MP, Greenland S. Meta-analysis of epidemiologic dose-response data. Epidemiology. 1993;4(3):218–28.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Peng B, Ni J, Anderson CS, Zhu Y, Wang Y, et al. Implementation of a Structured Guideline-Based Program for the Secondary Prevention of Ischemic Stroke in China. Stroke. 2014;45(2):515–9.
Shalev V, Goldshtein I, Porath A, Weitzman D, Shemer J, Chodick G. Continuation of statin therapy and primary prevention of nonfatal cardiovascular events. Am J Cardiol. 2012;110(12):1779–86.
Rublee DA, Chen SY, Mardekian J, Wu N, Rao P, Boulanger L. Evaluation of cardiovascular morbidity associated with adherence to atorvastatin therapy. Am J Ther. 2012;19(1):24–32.
Degli Esposti L, Saragoni S, Batacchi P, Benemei S, Geppetti P, Sturani A, Buda S, Degli Esposti E. Adherence to statin treatment and health outcomes in an Italian cohort of newly treated patients: results from an administrative database analysis. Clin Ther. 2012;34(1):190–9.
Putaala J, Haapaniemi E, Kaste M, Tatlisumak T. Statins after ischemic stroke of undetermined etiology in young adults. Neurology. 2011;77(5):426–30.
Dragomir A, Cote R, White M, Lalonde L, Blais L, Berard A, Perreault S. Relationship between adherence level to statins, clinical issues and health-care costs in real-life clinical setting. Value Health. 2010;13(1):87–94.
Risselada R, Straatman H, van Kooten F, Dippel DW, van der Lugt A, Niessen WJ, Firouzian A, Herings RM, Sturkenboom MC. Withdrawal of statins and risk of subarachnoid hemorrhage. Stroke. 2009;40(8):2887–92.
Perreault S, Ellia L, Dragomir A, Cote R, Blais L, Berard A, Lalonde L. Effect of statin adherence on cerebrovascular disease in primary prevention. Am J Med. 2009;122(7):647–55.
Blackburn DF, Dobson RT, Blackburn JL, Wilson TW. Cardiovascular morbidity associated with nonadherence to statin therapy. Pharmacotherapy. 2005;25(8):1035–43.
Spencer FA, Allegrone J, Goldberg RJ, Gore JM, Fox KA, Granger CB, Mehta RH, Brieger D. Association of statin therapy with outcomes of acute coronary syndromes: the GRACE study. Ann Intern Med. 2004;140(11):857–66.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
Merwick A, Albers GW, Arsava EM, Ay H, Calvet D, et al. Reduction in early stroke risk in carotid stenosis with transient ischemic attack associated with statin treatment. Stroke. 2013;44(10):2814–20.
Tsivgoulis G, Katsanos AH, Sharma VK, Krogias C, Mikulik R, et al. Statin pretreatment is associated with better outcomes in large artery atherosclerotic stroke. Neurology. 2016;86(12):1103–11.
O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388(10046):761–75.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the National Science Foundation of China (No. 81571259).
Conflicts of interest
Tao Xu, Xinyuan Yu, Shu Ou, Xi Liu, Jinxian Yuan, and Yangmei Chen declare that they have no conflicts of interest.
Additional information
T. Xu and X. Yu equally contributed to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xu, T., Yu, X., Ou, S. et al. Statin Adherence and the Risk of Stroke: A Dose-Response Meta-Analysis. CNS Drugs 31, 263–271 (2017). https://doi.org/10.1007/s40263-017-0420-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-017-0420-5