Abstract
Background and Objective
IPX066 is a multiparticulate extended-release formulation of carbidopa–levodopa, designed to produce prolonged therapeutic levodopa plasma concentrations. This 9-month open-label extension study assessed its long-term safety and clinical utility in early and advanced Parkinson’s disease (PD).
Methods
Participants were enrolled from two phase III IPX066 studies and one open-label phase II study. Early PD patients were titrated to an appropriate dosing regimen while advanced patients started with regimens established in the antecedent studies. Adjustment was allowed throughout the extension. Clinical utility measures included the Unified Parkinson’s Disease Rating Scale (UPDRS) and Patient Global Impression (PGI) ratings.
Results
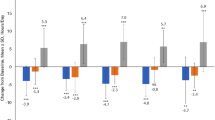
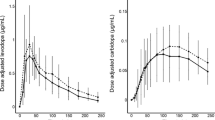
Among 268 early PD patients, 53.4 % reported adverse events (AEs) and 1.1 % (three patients) discontinued due to AEs; the most frequent AEs were nausea (5.6 %) and insomnia (5.6 %). Among 349 advanced patients, 60.2 % reported AEs and 3.7 % (13 patients) discontinued due to AEs; the most frequent AEs were dyskinesia (6.9 %) and fall (6.6 %). At month 9 (or early termination), 78.3 % of early patients were taking IPX066 three times daily (median: 720 mg/day) and 87.7 % of advanced patients were taking IPX066 three or four times daily (median: 1450 mg/day). Adjusting for 70 % bioavailability relative to immediate-release (IR) carbidopa–levodopa, the median dosages correspond to ~500 and ~1015 mg/day of IR levodopa in early and advanced PD, respectively. Based on the plasma profiles previously observed in PD patients, the IPX066 regimens in the extension can be estimated to provide a levodopa C max (maximum plasma drug concentration) similar to or lower than that provided by IR regimens during the antecedent trials. UPDRS and PGI findings showed sustained treatment effects throughout the extension.
Conclusion
During 9 months of extended use, IPX066 exhibited a safety/tolerability profile consistent with dopaminergic PD therapy.
Similar content being viewed by others
Throughout 9 months of extended, open-label treatment, IPX066, an investigational formulation of carbidopa–levodopa, showed acceptable long-term safety and tolerability in early and advanced Parkinson’s disease (PD). |
In early PD, most patients (~80 %) took IPX066 three times per day. Corrected for relative bioavailability, the dosages resembled those reported for immediate-release (IR) levodopa. |
In advanced PD, most patients (~90 %) took IPX066 three or four times per day. Corrected for relative bioavailability, the dosages were higher than those reported for IR levodopa, but this increase may be required to prolong therapeutic concentrations. |
1 Introduction
For treatment of Parkinson’s disease (PD), levodopa is the most effective oral pharmacotherapy developed to date [1, 2], and is typically administered in combination with a dopa-decarboxylase inhibitor such as carbidopa. As PD progresses, however, long-term use of oral levodopa is often associated with motor fluctuations, including ‘wearing-off’ between doses, and dyskinesias (involuntary movements) that often occur at times of peak levodopa plasma concentrations and maximal levodopa benefit [3, 4]. Eventually, patients may experience distressing periods of refractory, sometimes unpredictable, parkinsonism [5], with a large detrimental impact on their quality of life [6, 7]. Neurophysiological research suggests that the complications may be an outcome of long-term non-physiological pulsatile fluctuations in levodopa concentrations associated with dosing of conventional oral levodopa products [8]. Indeed, in clinical studies, continuous levodopa infusion has yielded significant reductions of ‘off’ time and dyskinesia [9–11]. The development of a levodopa formulation capable of delivering more stable plasma concentrations is therefore a major need for PD management. Although a controlled-release formulation is available [12], patients transferred to it from the immediate-release (IR) levodopa formulation have not consistently experienced significant ‘off’ time reduction [13–17] or a predictable response [18–21].
IPX066 (Impax Laboratories, Inc., Hayward, CA, USA) is an investigational multiparticulate, extended-release (ER) formulation of carbidopa and levodopa in a 1:4 ratio. It was designed to rapidly achieve therapeutic plasma levodopa concentrations and maintain them for a prolonged duration to allow a dosing interval of approximately 6 h in both early and advanced disease [22]. In a phase II crossover study [23] comparing IPX066 pharmacokinetics with those of IR carbidopa–levodopa (CD-LD) in advanced PD patients with motor fluctuations, the IPX066 initial absorption rate was rapid, similar to that of IR CD-LD. In addition, IPX066 maintained levodopa plasma concentrations above 50 % of the maximum plasma drug concentration (C max) for a longer duration than IR CD-LD (4 vs. 1.4 h). Compared with IR CD-LD, IPX066 also reduced the levodopa C max/C min (minimum plasma drug concentration) ratio (12.0 ± 18.5 vs. 82.2 ± 67.5) and fluctuation index (1.5 ± 0.4 vs. 3.2 ± 1.3) at steady state. The bioavailability of IPX066 was determined to be approximately 70 % in terms of levodopa area under the plasma concentration–time curve (AUC) and 30 % in terms of levodopa C max compared with IR CD-LD in advanced PD patients [23]. Phase III clinical trials have reported the efficacy and safety of IPX066 during 30 weeks of treatment in early PD [24] and 19 weeks of treatment (including 6 weeks of IPX066 dose conversion) in advanced PD [25].
Here we present safety results, clinical utility findings, and dosing regimens for IPX066 during its long-term use in early and advanced PD patients.
2 Methods
2.1 Study Participants
All patients had completed either of two controlled IPX066 phase III clinical trials [24, 25] or a phase II crossover trial [23] and continued to have a diagnosis of PD eligible for levodopa therapy. One of the phase III trials, APEX-PD [24], was a 30-week randomized, double-blind, double-dummy, parallel-arm study of three fixed-dose IPX066 regimens vs. placebo in 381 early PD patients who were naïve to levodopa (not exposed to levodopa for >30 days, and not within 4 weeks of enrollment) and were not being treated with dopamine agonists. IPX066 or matching placebo was titrated to 145, 245, or 390 mg three times daily. The IPX066 regimens were estimated to produce levodopa AUC values similar to those for IR CD-LD regimens of 300, 500, and 800 mg/day and C max values similar to those for IR CD-LD doses of 45, 75, and 120 mg, respectively. The other phase III trial, ADVANCE-PD [25], was a randomized, double-blind, double-dummy, parallel-arm study of IPX066 vs. IR CD-LD in 393 advanced PD patients with at least 2.5 h/day of ‘off’ time. During a 3-week open-label period, each patient’s IR CD-LD regimen was adjusted. Open-label conversion to IPX066 was then performed during a 6-week period, based on the adjusted IR CD-LD regimen. Patients were then randomized to IPX066 or IR CD-LD for a 13-week maintenance period. Advanced PD patients who had completed an open-label, two-period (8 days per period) crossover phase II study of IPX066 vs. IR CD-LD [23] were also eligible for this extension trial.
2.2 Study Design
For patients who had completed their previous study within 4 weeks before enrolling in this trial, the termination visit in each patient’s previous study served as this trial’s first visit (extension baseline). However, patients who had completed their previous study more than 4 weeks before this extension were required to undergo the first-visit procedures to re-establish baseline measures. For all patients who were enrolled from the phase II study, this gap exceeded 1 year, necessitating a baseline visit.
During the extension, all four strengths of IPX066 capsules (carbidopa/levodopa 23.5/95, 36.25/145, 48.75/195, or 61.25/245 mg) were available for treating patients. Individualized dosing regimens could be achieved by combining different capsules. Because the blind in the early PD study had not yet been broken, IPX066 was up-titrated as if all early PD patients were levodopa-naïve. The recommended starting dosage was one 95 mg capsule three times daily for approximately 3 days, with optional up-titration every 3 days to one 145 mg capsule three times daily, two 95 mg capsules three times daily, and then two 145 mg capsules three times daily. In advanced PD, the recommended starting dosages were the same as those established during the open-label dose conversion period in the antecedent study. For all patients, the recommended dosing interval was approximately every 6 h during waking hours (three doses per day; e.g., at 6 a.m., noon, and 6 p.m.). Patients could also take a bedtime dose (four times daily dosing) but were not to take more than five doses per day. The between-dose interval could vary but had to be ≥4 h. Regimen adjustment was allowed throughout the extension at the investigators’ discretion.
Nonselective monoamine oxidase (MAO) inhibitors were prohibited; rasagiline was allowed at therapeutic dose ranges [26]. The study was registered with ClinicalTrials.gov (identifier: NCT01096186) [27].
2.3 Assessments
At months 1, 5, and 9 (or early termination), IPX066 dosing and safety were assessed, the latter from data including adverse events (AEs) and vital signs. At months 1 and 9 (or early termination), clinical laboratory tests and 12-lead electrocardiograms were also performed. Clinical utility was measured using the Unified Parkinson’s Disease Rating Scale (UPDRS) Parts I–IV (assessed during the patient’s ‘on’ state by a study investigator or appropriately trained site personnel), Patient Global Impression (PGI) scale, EuroQol 5-Dimension (EQ-5D) health-related quality of life scale, 39-item Parkinson’s Disease Questionnaire (PDQ-39), and 36-item Short-Form (SF-36) health survey questionnaire. The UPDRS, PGI, and PDQ-39 were assessed at months 1, 5, and 9 (or early termination). EQ-5D and SF-36 were assessed at months 5 and 9.
2.4 Statistical Methods
The extension’s safety data were summarized descriptively, with separate summaries for the early and advanced PD groups, each of which included all patients who received open-label IPX066. UPDRS scores for Part II (activities of daily living) plus Part III (motor examination) are presented for five timepoints: baseline and end of study in the preceding trial, and months 1, 5, and 9 of the extension. PGI results are presented for extension months 1, 5, and 9, with categories collapsed to three ratings: dissatisfied (“somewhat,” “very,” or “very much”); satisfied (“somewhat,” “very,” or “very much”); and neither satisfied nor dissatisfied.
To evaluate average ‘off’ time, a post hoc descriptive analysis of scores on UPDRS Part IV, Question 39 (“What proportion of the waking day is the patient ‘off’ on average?”) was completed for end-of-study data from the preceding trial and for extension month 9. Question 39 is scored 0 (none), 1 (1–25 %), 2 (26–50 %), 3 (51–75 %), or 4 (76–100 %).
3 Results
3.1 Patient Flow
At 80 sites in North America and Europe, a total of 617 patients were enrolled in the extension, beginning in March 2010. Of 300 eligible patients with early PD (all from APEX-PD), 268 (89.3 %) enrolled. Among them, 254 patients (94.8 %) completed the extension. Of 395 eligible patients with advanced PD, 349 (88.4 %) enrolled (336 from ADVANCE-PD and 13 from the phase II study). Among them, 313 patients (89.7 %) completed the extension.
During the extension, 22 patients (3.6 %) withdrew consent, 16 (2.6 %) discontinued due to AEs, four (0.6 %) discontinued due to lack of efficacy, and four (0.6 %) died (Fig. 1). No early PD patients and one advanced PD patient discontinued due to non-compliance with study drug. Including the length of treatment in the antecedent trials, early PD patients were treated with IPX066 for a total of 39–69 weeks, and advanced PD patients were treated with IPX066 for a total of 40–58 weeks. The final patient completed the extension in October 2011.
3.2 Baseline Characteristics
Overall, extension patients had a mean age of 64.1 years (range 41–89 years), were almost entirely white (Table 1), and comprised more males than females. However, the proportion of females was higher in early PD than in advanced PD (42 vs. 35 %). On average, the early PD group was older at diagnosis than the advanced PD group (62.4 vs. 55.5 years).
3.3 IPX066 Regimens in Early Parkinson’s Disease (PD)
At month 9 of the extension (or early termination), 83.3 % of the patients with early PD (219 of 263) were taking 435–1170 mg/day of IPX066, corresponding to approximately 300–820 mg/day of IR levodopa after correction for 70 % relative bioavailability. The median (mean ± standard deviation [SD]) total dosage of IPX066 was 720 (727 ± 325) mg/day, corresponding to approximately 500 mg/day of IR levodopa. The dosages were similar to the IPX066 dosages used in the antecedent early PD study (435, 735, or 1170 mg/day). In addition, 78.3 % of the patients (206 of 263) had maintained their three times daily dosing. Another 9.9 % were taking IPX066 twice daily, one patient was taking it once daily, 11.0 % were taking it four times daily, and one patient was taking it five times daily.
3.4 IPX066 Regimens in Advanced PD
At month 9 (or early termination), 84.5 % of the patients from ADVANCE-PD (278 of 329) were taking 800–2450 mg/day of IPX066, corresponding to approximately 560–1715 mg/day of IR levodopa. Another 4.9 % were taking <800 mg/day, and 10.6 % were taking >2450 mg/day. The median (mean ± SD) IPX066 dosage was 1450 (1618 ± 726) mg/day, corresponding to approximately 1015 mg/day of IR levodopa. In ADVANCE-PD, the median (mean ± SD) IPX066 dosage among patients who enrolled in the extension had been 1330 (1568 ± 697) mg/day; hence, the median and mean increases during the extension were less than 10 %.
At month 9, 45.2, 42.5, and 10.6 % of advanced PD patients were taking IPX066 three, four, or five times daily, respectively, and four patients (1.2 %) were taking it more than five times daily. For most patients, the dosing frequency established during the preceding study was maintained at month 9, with 79.7, 82.2, and 83.3 % of patients who took IPX066 three or fewer, four, or five times daily in the preceding study still doing so.
3.5 Other PD Drugs
At extension entry, approximately half of the patients with advanced PD and almost no patients with early PD were using dopamine agonists (see Table 1). Approximately one-quarter of patients in each group were using MAO-B inhibitors, approximately one-fifth were using amantadine, and less than 5 % were using anticholinergics. Approximately one-quarter of the early PD patients and one-tenth of the advanced PD patients reported using levodopa-containing products during the gap between their antecedent study and the extension. During the extension, small proportions of patients—6.0 % of the early PD patients (16 of 268) and 6.9 % of the advanced PD patients (24 of 349)—continued taking levodopa-containing medications. In addition, 3.4 % of the early PD patients (nine of 268) and 3.2 % of the advanced PD patients (11 of 349) continued to use a catechol-O-methyltransferase inhibitor.
3.6 Adverse Events
Among the 617 patients who entered the extension, 353 (57.2 %) reported AEs (Table 2). Only fall (reported by 32 patients, or 5.2 %) was reported by more than 5.0 % of the total extension population. Among the AEs reported by more than 5.0 % of patients in the early or advanced PD subgroups, insomnia and nausea were reported by a greater percentage of patients with early PD, whereas fall and dyskinesia were reported by a greater percentage of patients with advanced PD. In early PD, dyskinesia was reported by five patients (1.9 %), all of whom had been treated with IPX066 in the original trial. In advanced PD, dyskinesia was reported by 24 patients (6.9 %).
Four patients (0.6 %) died during the extension. Their causes of death were hemorrhagic stroke, hemorrhagic pancreatitis, prostate cancer, and unknown. None of the deaths was considered by the investigators to be related to IPX066.
Forty-three patients (7.0 %) reported serious AEs. Those reported for more than one patient were femoral neck fracture (n = 3) and fall, atrial fibrillation, gastritis, hyponatremia, spinal column stenosis, and spinal osteoarthritis (n = 2 each).
Sixteen patients (2.6 %) reported AEs as the reason for withdrawal from the extension. Those reported for more than one patient were nausea, hallucinations, and dizziness (n = 2 each).
3.7 Clinical Utility
In early and in advanced PD, UPDRS Parts II + III scores throughout the extension maintained the mean improvement seen during the previous studies (Table 3). In early PD, patients previously on placebo attained mean scores similar to those achieved by patients treated with IPX066 in the antecedent APEX-PD study (24.9 vs. 24.0 at month 9). In advanced PD, patients previously randomized to IR CD-LD in the antecedent ADVANCE-PD study attained mean scores similar to those achieved by patients randomized to IPX066 in that study (28.1 vs. 28.2 at month 9). Mean PDQ-39 total scores at month 9 showed some decline of the improvement attained in the antecedent studies for patients previously randomized to IPX066 treatment (see Table 3). However, the scores at month 9 were similar across all patients whether or not they received IPX066 in the preceding studies. SF-36 and EQ-5D findings suggested little change from the preceding studies (data not shown). On the PGI scale, the proportion of patients satisfied with their IPX066 therapy was approximately 80 % at each extension timepoint (see Table 3).
In a post hoc analysis of time in the ‘off’ state, the mean (SD) score on UPDRS Part IV, Question 39 among early PD patients was 0.1 (0.52) at the end of their antecedent trial, with 92.5 % (248 of 268) scoring 0 (“none”), and 0.1 (0.32) at extension month 9, and 90.6 % (230 of 253) scoring 0. Among patients with advanced PD, the mean at the end of their antecedent trial was 1.3 (0.58), with 4.2 % (14 of 336) scoring 0, and 1.0 (0.59) at extension month 9, and 14.7 % (46 of 313) scoring 0.
4 Discussion
During 9 months of extended, open-label treatment, IPX066 continued to exhibit acceptable safety and tolerability profiles in patients with early or advanced PD. In early PD, the most frequently reported AEs, nausea and insomnia, are commonly reported for dopaminergic drugs [2, 28]. In advanced PD, the most frequently reported AEs, dyskinesia and fall, are commonly associated with PD therapies and/or PD progression [2, 28].
It is worth noting that in early PD, the incidence of dyskinesia reported as an AE during the open-label extension remained low, at 1.9 %, a rate similar to that reported in the antecedent APEX-PD study (2.9 %) [24]. The consistent, low dyskinesia AE rates observed during IPX066 studies [23–25] may have resulted from a prolonged duration of therapeutic levodopa plasma concentrations and reduced peak/trough fluctuations [23], both of which have been shown to reduce the severity of dyskinesia in PD patients [29, 30]. In advanced PD, the reported incidence of dyskinesia during the open-label extension (6.9 %) was similar to that reported during the open-label dose-conversion phase of the antecedent ADVANCE-PD study (6 %) [25].
This study also demonstrated that IPX066 regimens generally remained stable for the duration of the extension. In early PD, most patients (~80 %) continued to take IPX066 three times daily, and dosages were in the range of those used in the antecedent APEX-PD study [24]. The median dosage was 720 mg/day, which corresponds to approximately 500 mg/day of IR levodopa after correction for 70 % relative bioavailability, a dosage similar to the IR dosages reported in other early PD studies [4, 31–33]. The sustained benefit seen in UPDRS II + III score differs from the less sustained benefit reported in the ELLDOPA (Earlier vs. Later Levodopa Therapy in Parkinson Disease) study of levodopa in early PD [4], perhaps reflecting differences in levodopa plasma profiles.
In advanced PD, most patients (~90 %) took IPX066 three or four times per day. The mean and median dosages differed only slightly (<10 %) from those in the antecedent ADVANCE-PD study, suggesting that the antecedent study’s allotment of 6 weeks for dose conversion from IR CD-LD had been appropriate. The median dosage was 1450 mg/day, corresponding to approximately 1000 mg/day of IR levodopa, which is higher than the median dosage of approximately 800 mg/day of IR CD-LD in studies of IPX066 [23, 25] and entacapone [34] in advanced PD with motor fluctuations. The higher dosage is required to sustain therapeutic plasma concentrations of levodopa and minimize the peak/trough fluctuations characteristic of standard IR formulations. Although the dosages were higher, the extension’s advanced PD patients benefitted from IPX066 treatment, and dyskinesia, as a reported AE, remained infrequent throughout long-term IPX066 use.
Interpretations of this study’s findings may be limited by the trial’s open-label design and by the absence of placebo or active comparator groups. In addition, the antecedent double-blind studies differed in their study populations and in the duration of IPX066 treatment [24, 25]. Hence, patients who entered the extension had differing prior exposures to IPX066. Further, the APEX-PD study of patients with early PD had a fixed-dose design vs. placebo [24] while the ADVANCE-PD study utilized individualized dosing of IPX066 vs. an active control, IR CD-LD [25]. Nevertheless, the effects of IPX066 treatment seen in the original trials were sustained with longer exposure to IPX066 in this extension study.
5 Conclusions
Administration of IPX066 for 9 months in early and advanced PD populations appeared to be well-tolerated and exhibited safety patterns consistent with the known effects of commercially available CD-LD products in the PD population. Based on UPDRS and PGI findings, the clinical utility of IPX066 was maintained throughout the study’s extended treatment period.
References
Jankovic J, Stacy M. Medical management of levodopa-associated motor complications in patients with Parkinson’s disease. CNS Drugs. 2007;21:677–92.
Olanow CW, Stern MB, Sethi K. The scientific and clinical basis for the treatment of Parkinson disease. Neurology. 2009;72(21 Suppl 4):S1–136.
Olanow CW, Kieburtz K, Rascol O, et al. Factors predictive of the development of levodopa-induced dyskinesia and wearing-off in Parkinson’s disease. Mov Disord. 2013;28:1064–71.
Fahn S, Oakes D, Shoulson I, et al. Levodopa and the progression of Parkinson’s disease. N Engl J Med. 2004;351:2498–508.
deSouza RM, Moro E, Lang AE, Schapira AH. Timing of deep brain stimulation in Parkinson disease: a need for reappraisal? Ann Neurol. 2013;73:565–75.
Dodel RC, Berger K, Oertel WH. Health-related quality of life and healthcare utilisation in patients with Parkinson’s disease: impact of motor fluctuations and dyskinesias. Pharmacoeconomics. 2001;19:1013–38.
Politis M, Wu K, Molloy S, Bain PG, Chaudhuri KR, Piccini P. Parkinson’s disease symptoms: the patient’s perspective. Mov Disord. 2010;25:1646–51.
Olanow CW, Obeso JA, Stocchi F. Continuous dopamine-receptor treatment of Parkinson’s disease: scientific rationale and clinical implications. Lancet Neurol. 2006;5:677–87.
Sage JI, Trooskin S, Sonsalla PK, Heikkila R, Duvoisin RC. Long-term duodenal infusion of levodopa for motor fluctuations in parkinsonism. Ann Neurol. 1988;24:87–9.
Nilsson D, Hansson LE, Johansson K, Nystrom C, Paalzow L, Aquilonius SM. Long-term intraduodenal infusion of a water based levodopa–carbidopa dispersion in very advanced Parkinson’s disease. Acta Neurol Scand. 1998;97:175–83.
Stocchi F, Vacca L, Ruggieri S, Olanow CW. Intermittent vs continuous levodopa administration in patients with advanced Parkinson disease: a clinical and pharmacokinetic study. Arch Neurol. 2005;62:905–10.
Sinemet-CR (carbidopa–levodopa sustained release) tablets [package insert]. Whitehouse Station: Merck & Co., and Princeton: Bristol-Myers Squibb Company; 2009.
Ahlskog JE, Muenter MD, McManis PG, Bell GN, Bailey PA. Controlled-release Sinemet (CR-4): a double-blind crossover study in patients with fluctuating Parkinson’s disease. Mayo Clin Proc. 1988;63:876–86.
Hutton JT, Morris JL, Roman GC, Imke SC, Elias JW. Treatment of chronic Parkinson’s disease with controlled-release carbidopa/levodopa. Arch Neurol. 1988;45:861–4.
Jankovic J, Schwartz K, Vander Linden C. Comparison of Sinemet CR4 and standard Sinemet: double-blind and long-term open trial in parkinsonian patients with fluctuations. Mov Disord. 1989;4:303–9.
Lieberman A, Gopinathan G, Miller E, Neophytides A, Baumann G, Chin L. Randomized double-blind cross-over study of Sinemet controlled release (CR4 50/200) versus Sinemet 25/100 in Parkinson’s disease. Eur Neurol. 1990;30:75–8.
Pahwa R, Factor SA, Lyons KE, et al. Practice parameter: treatment of Parkinson disease with motor fluctuations and dyskinesia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;66:983–95.
Cedarbaum JM, Hoey M, McDowell FH. A double-blind crossover comparison of Sinemet CR4 and standard Sinemet 25/100 in patients with Parkinson’s disease and fluctuating motor performance. J Neurol Neurosurg Psychiatry. 1989;52:207–12.
Sage JI, Mark MH. Comparison of controlled-release Sinemet (CR4) and standard Sinemet (25 mg/100 mg) in advanced Parkinson’s disease: a double-blind, crossover study. Clin Neuropharmacol. 1988;11:174–9.
Deleu D, Jacques M, Michotte Y, Ebinger G. Controlled-release carbidopa/levodopa (CR) in parkinsonian patients with response fluctuations on standard levodopa treatment: clinical and pharmacokinetic observations. Neurology. 1989;39(Suppl 2):88–92.
Stocchi F, Quinn NP, Barbato L, et al. Comparison between a fast and a slow release preparation of levodopa and a combination of the two: a clinical and pharmacokinetic study. Clin Neuropharmacol. 1994;17:38–44.
Hauser RA. IPX066: a novel carbidopa–levodopa extended-release formulation. Expert Rev Neurother. 2012;12:133–40.
Hauser RA, Ellenbogen AL, Metman LV, et al. Crossover comparison of IPX066 and a standard levodopa formulation in advanced Parkinson’s disease. Mov Disord. 2011;26:2246–52.
Pahwa R, Lyons KE, Hauser RA, et al. Randomized trial of IPX066, carbidopa/levodopa extended release, in early Parkinson’s disease. Parkinsonism Relat Disord. 2014;20:142–8.
Hauser RA, Hsu A, Kell S, et al. Extended-release carbidopa–levodopa (IPX066) compared with immediate-release carbidopa–levodopa in patients with Parkinson’s disease and motor fluctuations: a phase 3 randomised, double-blind trial. Lancet Neurol. 2013;12:346–56.
Azilect prescribing information. 2014. http://www.azilect.com/Resources/pdf/PrescribingInformation.pdf. Accessed 2 Oct 2014.
IMPAX Laboratories, Inc. An open label extension study of the safety and clinical utility of IPX066 in subjects with Parkinson’s disease [ClinicalTrials.gov identifier NCT01096186]. US National Institutes of Health, ClinicalTrials.gov. http://www.clinicaltrials.gov. Accessed 24 Mar 2015.
Connolly BS, Lang AE. Pharmacological treatment of Parkinson disease: a review. JAMA. 2014;311:1670–83.
Fernandez HH, Vanagunas A, Odin P, et al. Levodopa–carbidopa intestinal gel in advanced Parkinson’s disease open-label study: interim results. Parkinsonism Relat Disord. 2013;19:339–45.
Olanow CW, Kieburtz K, Odin P, et al. Continuous intrajejunal infusion of levodopa–carbidopa intestinal gel for patients with advanced Parkinson’s disease: a randomised, controlled, double-blind, double-dummy study. Lancet Neurol. 2014;13:141–9.
Whone AL, Watts RL, Stoessl AJ, et al. Slower progression of Parkinson’s disease with ropinirole versus levodopa: the REAL-PET study. Ann Neurol. 2003;54:93–101.
Hauser RA, Rascol O, Korczyn AD, et al. Ten-year follow-up of Parkinson’s disease patients randomized to initial therapy with ropinirole or levodopa. Mov Disord. 2007;22:2409–17.
Katzenschlager R, Head J, Schrag A, et al. Fourteen-year final report of the randomized PDRG-UK trial comparing three initial treatments in PD. Neurology. 2008;71:474–80.
Parkinson Study Group. Entacapone improves motor fluctuations in levodopa-treated Parkinson’s disease patients. Ann Neurol. 1997;42:747–55.
Acknowledgments
This study was funded by Impax Laboratories, Inc. Impax participated in the study design; data collection, interpretation, and analysis; writing and editing the report; and reviewing and approving the manuscript for submission. Medical writing support (in the form of grammatical editing, copyediting, styling, and illustration preparation) was provided by Michael Feirtag of The Curry Rockefeller Group, LLC, funded by Impax. Cheryl Waters has been an investigator in Impax-sponsored clinical trials and has received honoraria for speaking engagements from UCB and Teva Pharmaceuticals. Paul Nausieda has received honoraria from Impax laboratories, Inc. for consulting services and as an investigator. He has spoken on behalf of Novartis, UCB, Inc., and Teva Pharmaceuticals and has held stock in the following companies: Abbott Laboratories, Bristol-Myers Squibb, Celgene, Dow Chemical, Dupont, Durata Therapeutics, Eli Lilly, Gilead, GlaxoSmithKline, Humana, Impax Laboratories, Inc., Johnson and Johnson, Neogen, Roche Holding, Sigma-Aldrich, and Teva Neuroscience. He received financial support from Adamas Pharmaceuticals, Aurora Health Care Foundation, Biotie Therapies, Greater Milwaukee Foundation, Helen Bader Foundation, Icon Clinical Research, Impax Laboratories, Inc., Milwaukee County Department of Family Care, Pharmanet LLC, PRA International, Quintiles Inc., Schwarz Biosciences/UCB, Wisconsin Parkinson Association, and XenoPort. Lyudmila Dzyak has been an investigator in Impax-sponsored clinical trials. Joerg Spiegel has been an investigator in Impax-sponsored clinical trials. Monika Rudinska has been an investigator in Impax-sponsored clinical trials. Dee Silver has nothing to declare. Elena Tsurkalenko has participated in Impax-sponsored clinical trials. Sherron Kell, Sarita Khanna, and Suneel Gupta are employees of Impax Laboratories and own Impax stock and/or stock options. Ann Hsu was an employee of Impax Laboratories when the studies were conducted and owns Impax stock.
Ethical standards
The study was conducted in accordance with ethical principles outlined in the International Committee on Harmonisation (ICH) Good Clinical Practice (GCP) guidelines and in the Declaration of Helsinki. Before study initiation, the study protocol was reviewed by the relevant Institutional Review Boards or Independent Ethics Committees, and written approval was obtained. Written informed consent was obtained from each patient before enrollment into the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial registration: ClinicalTrials.gov NCT01096186.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Waters, C.H., Nausieda, P., Dzyak, L. et al. Long-Term Treatment with Extended-Release Carbidopa–Levodopa (IPX066) in Early and Advanced Parkinson’s Disease: A 9-Month Open-Label Extension Trial. CNS Drugs 29, 341–350 (2015). https://doi.org/10.1007/s40263-015-0242-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-015-0242-2