Abstract
Background and Objective
The microbial susceptibility of many antibiotics has been affected by prescribing patterns and their extensive use. The purpose of this evaluation was to assess how these changes could affect the initial efficacy of ertapenem and piperacillin/tazobactam in the treatment of complicated intra-abdominal infections (IAIs) acquired in the community and the potential consequences this may have in healthcare costs in Spain.
Methods
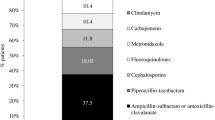
The Initial efficacy of ertapenem and piperacillin/tazobactam for patients with APACHE (Acute Physiology and Chronic Health Evaluation) II scores <10 was extracted from a multicenter randomized study and were combined with the current microbial susceptibilities obtained from the SMART study, a multinational surveillance program. Country-specific pathogens distribution was extracted from a national study in patients with community-acquired IAI. The estimated effectiveness was used in a decision-analytic model to compare total costs between ertapenem and piperacillin/tazobactam in the treatment of complicated IAI. The model performs extensive one-way and probabilistic sensitivity analyses.
Results
The model suggested a savings of €209 (year 2012 values) per patient when complicated IAIs acquired in the community (APACHE II <10) were treated with ertapenem instead of piperacillin/tazobactam. One-way sensitivity analyses showed length of stay as the key driver parameter. Further analysis of this parameter and probabilistic sensitivity analysis confirmed the robustness of our evaluation, with a 58 % likelihood of ertapenem being dominant.
Conclusions
Ertapenem appears to be a cost-saving strategy over piperacillin/tazobactam for the treatment of patients with complicated IAIs acquired in the community in Spain.






Similar content being viewed by others
References
Christou NV, Turgeon P, Wassef R, et al. Management of intra-abdominal infections. The case for intraoperative cultures and comprehensive broad-spectrum antibiotic coverage. Arch Surg. 1996;131:1193–201.
Tellado JM, Sen SS, Caloto MT, et al. Consequences of inappropriate initial empiric parenteral antibiotic therapy among patients with community-acquired intra-abdominal infections in Spain. Scand J Infect Dis. 2007;39(11–12):947–55.
Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(2):133–64.
Guirao X, Arias J, Badía JM, García-Rodríguez JA, Mensa J, Alvarez-Lerma F, et al. Recommendations in the empiric anti-infective agents of intra-abdominal infection. Cir Esp. 2010;87(2):63–81.
Gin A, Dilay L, Karlowsky JA, et al. Piperacillin-tazobactam: a beta-lactam/beta-lactamase inhibitor combination. Expert Rev Anti Infect Ther. 2007;5(3):365–83.
Solomkin JS, Yellin AE, Rotstein OD, Protocol 017 Study Group, et al. Ertapenem versus piperacillin/tazobactam in the treatment of complicated intra-abdominal infections: results of a double-blind, randomized comparative phase III trial. Ann Surg. 2003;237(2):235–45.
Hawser SP, Bouchillon SK, Hoban DJ, et al. Epidemiologic trends, occurrence of extended-spectrum beta-lactamase production, and performance of ertapenem and comparators in patients with intra-abdominal infections: analysis of global trend data from 2002–2007 from the SMART study. Surg Infect (Larchmt). 2010;11(4):371–8.
Cantón R, Loza E, Aznar J, SMART-Spain Working Group, et al. Antimicrobial susceptibility of Gram-negative organisms from intra-abdominal infections and evolution of isolates with extended spectrum β-lactamases in the SMART study in Spain (2002–2010). Rev Esp Quimioter. 2011;24(4):223–32.
Qvist N, Warren B, Leister-Tebbe H, et al. Efficacy of tigecycline versus ceftriaxone plus metronidazole for the treatment of complicated intra-abdominal infections: results from a randomized, controlled trial. Surg Infect (Larchmt). 2012;13(2):102–9.
Prasad P, Sun J, Danner RL, et al. Excess deaths associated with tigecycline after approval based on non-inferiority trials. Clin Infect Dis. 2012;54(12):1699–709.
EMA. Questions and answers on the review of Tygacil (tigecycline). Outcome of a renewal procedure. 2011. http://www.ema.europa.eu/docs/en_GB/document_library/Medicine_QA/human/000644/WC500102228.pdf. Accessed 25 June 2013.
FDA. Drug Safety Communication. Increased risk of death with Tygacil (tigecycline) compared to other antibiotics used to treat similar infections. 2010. http://www.fda.gov/Drugs/DrugSafety/ucm224370.htm. Accessed 25 June 2013.
Dietrich ES, Schubert B, Ebner W, et al. Cost efficacy of tazobactam/piperacillin versus imipenem/cilastatin in the treatment of intra-abdominal infection. Pharmacoeconomics. 2001;19(1):79–94.
Tubau F, Liñares J, Rodríguez MD, et al. Susceptibility to tigecycline of isolates from samples collected in hospitalized patients with secondary peritonitis undergoing surgery. Diagn Microbiol Infect Dis. 2010;66(3):308–13.
Gobernado M, Sanz-Rodríguez C, Villanueva R, et al. In vitro activity of ertapenem against clinical bacterial isolates in 69 Spanish medical centers (E-test study). Rev Esp Quimioter. 2007;20(4):395–408.
Mayne D, Dowzicky MJ. In vitro activity of tigecycline and comparators against organisms associated with intra-abdominal infections collected as part of TEST (2004–2009). Diagn Microbiol Infect Dis. 2012;74(2):151–7.
Joly-Guillou ML, Kempf M, Cavallo JD, et al. Comparative in vitro activity of Meropenem, Imipenem and Piperacillin/tazobactam against 1071 clinical isolates using 2 different methods: a French multicentre study. BMC Infect Dis. 2010;10:72.
Cuevas O, Cercenado E, Goyanes MJ, et al. Staphylococcus spp. in Spain: present situation and evolution of antimicrobial resistance (1986–2006) [in Spanish]. Enferm Infecc Microbiol Clin. 2008;26(5):269–77.
Treviño M, Areses P, Peñalver MD, et al. Susceptibility trends of Bacteroides fragilis group and characterization of carbapenemase-producing strains by automated REP-PCR and MALDI TOF. Anaerobe. 2012;18(1):37–43.
Seifert H, Dalhoff A, PRISMA Study Group. German multicentre survey of the antibiotic susceptibility of Bacteroides fragilis group and Prevotella species isolated from intra-abdominal infections: results from the PRISMA study. J Antimicrob Chemother. 2010;65(11):2405–10.
Jansen JP, Kumar R, Carmeli Y. Cost-effectiveness evaluation of ertapenem versus piperacillin/tazobactam in the treatment of complicated intra-abdominal infections accounting for antibiotic resistance. Value Health. 2009;12(2):234–44.
Jansen JP, Kumar R, Carmeli Y. Accounting for the development of antibacterial resistance in the cost effectiveness of ertapenem versus piperacillin/tazobactam in the treatment of diabetic foot infections in the UK. Pharmacoeconomics. 2009;27(12):1045–56.
Krobot K, Yin D, Zhang Q, et al. Effect of inappropriate initial empiric antibiotic therapy on outcome of patients with community-acquired intra-abdominal infections requiring surgery. Eur J Clin Microbiol Infect Dis. 2004;23(9):682–7.
Sauerland S, Lefering R, Neugebauer EAM. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2004;(4):CD001546. doi:10.1002/14651858.CD001546.pub2.
Spanish Ministry of Health, Social Policy and Equality, Institute for Health Information. CMBD Minimum Basis Data Set. 2011. http://pestadistico.msc.es. Accessed 25 June 2013.
Spanish Ministry of Health, Social Policy and Equality. Institute for Health Information. Diagnosis Related Group costs in Spain. http://www.msssi.gob.es/estadEstudios/estadisticas/docs/SNS2011_PESOS_COSTES_AP27_DEF.pdf. Accessed 25 June 2013.
Spanish General Council of Official Colleges of Pharmacists. Bot PLUS 2.0. https://botplusweb.portalfarma.com/. Accessed 25 June 2013.
Royal decree-law 8/2010, of May 20, on extraordinary measures to reduce Government deficit (RDL 8/2010). http://www.boe.es/boe/dias/2010/05/24/pdfs/BOE-A-2010-8228.pdf. Accessed 25 June 2013.
Doern GV, Brecher SM. The clinical predictive value (or lack thereof) of the results of in vitro antimicrobial susceptibility tests. J Clin Microbiol. 2011;49(9):S11–4.
Fortaleza CM, Freire MP, FilhoDde C, et al. Risk factors for recovery of imipenem- or ceftazidime-resistant pseudomonas aeruginosa among patients admitted to a teaching hospital in Brazil. Infect Control Hosp Epidemiol. 2006;27(9):901–6.
Goldstein EJ, Citron DM, Peraino V, et al. Introduction of ertapenem into a hospital formulary: effect on antimicrobial usage and improved in vitro susceptibility of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2009;53(12):5122–6.
Dinubile MJ, Friedland I, Chan CY, et al. Bowel colonization with resistant gram-negative bacilli after antimicrobial therapy of intra-abdominal infections: observations from two randomized comparative clinical trials of ertapenem therapy. Eur J Clin Microbiol Infect Dis. 2005;24(7):443–9.
Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000;31(Suppl 4):S131–8.
Sáez-Castillo AJ, Olmo-Jiménez MJ, Pérez Sánchez JM, et al. Bayesian analysis of nosocomial infection risk and length of stay in a department of general and digestive surgery. Value Health. 2010;13(4):431–9.
Koperna T, Semmler D, Marian F. Risk stratification in emergency surgical patients: is the APACHE II score a reliable marker of physiological impairment? Arch Surg. 2001;136(1):55–9.
Namias N, Solomkin JS, Jensen EH, et al. Randomized, multicenter, double-blind study of efficacy, safety, and tolerability of intravenous ertapenem versus piperacillin/tazobactam in treatment of complicated intra-abdominal infections in hospitalized adults. Surg Infect (Larchmt). 2007;8(1):15–28.
Acknowledgments
The study described in this article was sponsored by Merck & Co., Inc. The study sponsor played a significant role in the analysis and interpretation of data. Pharmacoeconomics and Outcomes Research Iberia (PORIB), a consultant company specialized in economic evaluation of health interventions, was hired by Merck & Co., Inc. to collect the data, conduct the analysis, and write the manuscript. S. Grau, V. Lozano, A. Valladares, and R. Cavanillas have participated in acquisition, analysis, and interpretation of data and have been involved in drafting and reviewing the manuscript. G. Nocea has participated in the study design and interpretation of data and has been involved in reviewing the manuscript. Y. Xie has participated in the study design and has reviewed the manuscript. The final version submitted for publication was approved by all authors. A. Valladares acts as guarantor for the overall content. The authors thank Miguel Ángel Casado (PhD; medical writer) and Itziar Oyagüez (BA; medical writer), employees of PORIB, for their assistance with the preparation of this manuscript.
Conflict of interest
S. Grau has received honoraria for speaking at symposia organized on behalf of Pfizer, Astellas, Merck Sharp & Dohme, and Novartis. V. Lozano has served as an external consultant for Merck Sharp & Dohme. A. Valladares, R. Cavanillas, Y. Xie, and G. Nocea are current employees of Merck Sharp & Dohme.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grau, S., Lozano, V., Valladares, A. et al. Impact of a Dynamic Microbiological Environment on the Clinical Efficacy of Ertapenem and Piperacillin/Tazobactam in the Treatment of Complicated Community-Acquired Intra-Abdominal Infection in Spain: A Cost-Consequence Analysis. Appl Health Econ Health Policy 13, 369–379 (2015). https://doi.org/10.1007/s40258-015-0162-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-015-0162-9