Abstract
Background
Pressure ulcers are a major cause of mortality, morbidity, and increased healthcare cost. Nutritional support may reduce the incidence of pressure ulcers in hospitalised patients who are at risk of pressure ulcer and malnutrition.
Objectives
To evaluate the cost-effectiveness of nutritional support in preventing pressure ulcers in high-risk hospitalised patients, and to assess the value of further research to inform the decision to implement this intervention using value of information analysis (VOI).
Methods
The analysis was from the perspective of Queensland Health, Australia using a decision model with evidence derived from a systematic review and meta-analysis. Resources were valued using 2014 prices and the time horizon of the analysis was one year. Monte Carlo simulation was used to estimate net monetary benefits (NB) and to calculate VOI measures.
Results
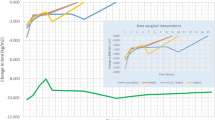
Compared with standard hospital diet, nutritional support was cost saving at AU$425 per patient, and more effective with an average 0.005 quality-adjusted life years (QALY) gained. At a willingness-to-pay of AU$50,000 per QALY, the incremental NB was AU$675 per patient, with a probability of 87 % that nutritional support is cost-effective. The expected value of perfect information was AU$5 million and the expected value of perfect parameter information was highest for the relative risk of developing a pressure ulcer at AU$2.5 million. For a future trial investigating the relative effectiveness of the interventions, the expected net benefit of research would be maximised at AU$100,000 with 1,200 patients in each arm if nutritional support was perfectly implemented. The opportunity cost of withholding the decision to implement the intervention until the results of the future study are available would be AU$14 million.
Conclusions
Nutritional support is cost-effective in preventing pressure ulcers in high-risk hospitalised patients compared with standard diet. Future research to reduce decision uncertainty is worthwhile; however, given the opportunity losses associated with delaying the implementation, “implement and research” is the approach recommended for this intervention.






Similar content being viewed by others
References
National Pressure Ulcer Advisory Panel (NPUAP) and European Pressure Ulcer Advisory Panel (EPUAP), prevention and treatment of pressure ulcers: clinical practice guideline. Washington, DC: NPUAP; 2009.
Australian Wound Management Association. Pan pacific clinical practice guidelines for the prevention and management of pressure injuries. Osborne Park: Cambridge Media; 2012.
Cuddigan J, Berlowitz D, Ayello EA. Pressure ulcers in America: prevalence, incidence, and implications for the future: an executive summary of the national pressure ulcer advisory panel monograph. Adv Skin Wound Care. 2001;14:208–15
VanGilder C, Amlung S, Harrison P, Meyer S. Results of the 2008–2009 International Pressure Ulcer Prevalence Survey and a 3-year, acute care, unit-specific analysis. Ostomy Wound Manage. 2009;55:39–45.
Graves N, Zheng H. The prevalence and incidence of chronic wounds:a literature review. Wound Pract Res. 2014, 22:4–19.
Padula WV, Mishra MK, Makic MB, Sullivan PW. Improving the quality of pressure ulcer care with prevention: a cost-effectiveness analysis. Med Care. 2011;49:385–92.
Dealey C, Posnett J, Walker A. The cost of pressure ulcers in the United Kingdom. J Wound Care. 2012, 21:261–262, 264, 266.
Graves N, Birrell FA, Whitby M. Modeling the economic losses from pressure ulcers among hospitalized patients in Australia. Wound Repair Regen. 2005;13:462–7.
National Institute for Health and Clinical Excellence. Pressure ulcer prevention: the prevention and management of pressure ulcers in primary and secondary care (CG179). London: The National Institute for Health and Care Excellence; 2014.
Banks M, Bauer J, Graves N, Ash S. Malnutrition and pressure ulcer risk in adults in Australian health care facilities. Nutrition. 2010;26:896–901.
Stratton RGC, Elia M. Disease-related malnutrition: an evidence-based approach to treatment. Wallingford: CABI Publishing; 2003.
Delmi M, Rapin CH, Bengoa JM, Delmas PD, Vasey H, Bonjour JP. Dietary supplementation in elderly patients with fractured neck of the femur. Lancet. 1990;335:1013–6.
Ek AC, Unosson M, Larsson J, Von Schenck H, Bjurulf P. The development and healing of pressure sores related to the nutritional state. Clin Nutr. 1991;10:245–50.
Bourdel-Marchasson I, Barateau M, Rondeau V, Dequae-Merchadou L, Salles-Montaudon N, Emeriau JP, Manciet G, Dartigues JF. A multi-center trial of the effects of oral nutritional supplementation in critically ill older inpatients. GAGE Group. Groupe Aquitain Geriatrique d’Evaluation. Nutrition. 2000;16:1–5.
Houwing RH, Rozendaal M, Wouters-Wesseling W, Beulens JW, Buskens E, Haalboom JR. A randomised, double-blind assessment of the effect of nutritional supplementation on the prevention of pressure ulcers in hip-fracture patients. Clin Nutr. 2003;22:401–5.
Claxton K. Exploring uncertainty in cost-effectiveness analysis. Pharmacoeconomics. 2008;26:781–98.
Eckermann S, Willan AR. Time and expected value of sample information wait for no patient. Value Health. 2008;11:522–6.
Tuffaha HW, Gordon LG, Scuffham PA. Value of information analysis in healthcare: a review of principles and applications.J. Med Econ. 2014;17:377–83.
Eckermann S, Karnon J, Willan AR. The value of value of information best informing research design and prioritization using current methods. Pharmacoeconomics. 2010;28:699–709.
Briggs AH, Goeree R, Blackhouse G, O’Brien BJ: Probabilistic analysis of cost-effectiveness models: choosing between treatment strategies for gastroesophageal reflux disease. Med Decis Mak 2002, 22:290–308.
Stinnett AA, Mullahy J: Net health benefits: A new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Mak 1998, 18:S68–S80.
Harris AH, Hill SR, Chin G, Li JJ, Walkom E. The role of value for money in public insurance coverage decisions for drugs in Australia: a retrospective analysis 1994–2004. Med Decis Making. 2008;28:713–22.
Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, Jeejeebhoy KN. What is subjective global assessment of nutritional status? 1987. Classical article. Nutr Hosp. 2008;23:400–7.
Stratton RJ, Ek AC, Engfer M, Moore Z, Rigby P, Wolfe R, Elia M. Enteral nutritional support in prevention and treatment of pressure ulcers: a systematic review and meta-analysis. Ageing Res Rev. 2005;4:422–50.
Banks MD, Graves N, Bauer JD, Ash S. Cost effectiveness of nutrition support in the prevention of pressure ulcer in hospitals. Eur J Clin Nutr. 2013;67:42–6.
Olofsson B, Stenvall M, Lundstrom M, Svensson O, Gustafson Y. Malnutrition in hip fracture patients: an intervention study. J Clin Nurs. 2007;16:2027–38.
Clemens S, Begum N, Harper C, Whitty JA, Scuffham PA. A comparison of EQ-5D-3L population norms in Queensland, Australia, estimated using utility value sets from Australia, the UK and USA. Qual Life Res. 2014;23(8):2375–81
Hawthorne G, Richardson J, Day NA. A comparison of the Assessment of Quality of Life (AQoL) with four other generic utility instruments. Ann Med. 2001;33:358–70.
Essex HN, Clark M, Sims J, Warriner A, Cullum N. Health-related quality of life in hospital inpatients with pressure ulceration: assessment using generic health-related quality of life measures. Wound Repair Regen. 2009;17:797–805.
Shemilt I. CCEMG-EPPI-Centre cost converter; Version 1.4. The Campbell and Cochrane Economics Methods Group (CCEMG) and the Evidence for Policy and Practice Information and Coordinating Centre (EPPI-Centre). http://eppi.ioe.ac.uk/costconversion/default.aspx. Acessed July 2014.
Australian hospital statistics 2011–12. Australian Institute of Health and Welfare Canberra. 2013. http://www.aihwgovau/WorkArea/DownloadAssetaspx?id=60129543146. Accessed May 2013.
Claxton K. Bayesian approaches to the value of information: implications for the regulation of new pharmaceuticals. Health Econ. 1999;8:269–74.
Ades AE, Lu G, Claxton K. Expected value of sample information calculations in medical decision modeling. Med Decis Mak. 2004, 24:207–227.
Groot Koerkamp B, Myriam Hunink MG, Stijnen T, Weinstein MC. Identifying key parameters in cost-effectiveness analysis using value of information: a comparison of methods. Health Economics. 2006, 15:383–392.
Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ. 1999;18:341–64.
Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52:1263–70.
Claxton KP, Sculpher MJ. Using value of information analysis to prioritise health research: some lessons from recent UK experience. Pharmacoeconomics. 2006;24:1055–68.
Claxton K, Posnett J. An economic approach to clinical trial design and research priority-setting. Health Economics. 1996;5:513–24.
Soares MO, Dumville JC, Ashby RL, Iglesias CP, Bojke L, Adderley U, McGinnis E, Stubbs N, Torgerson DJ, Claxton K, Cullum N. Methods to assess cost-effectiveness and value of further research when data are sparse: negative-pressure wound therapy for severe pressure ulcers. Med Decis Making. 2013;33:415–36.
Claxton K, Palmer S, Longworth L, Bojke L, Griffin S, McKenna C, Soares M, Spackman E, Youn J. Informing a decision framework for when NICE should recommend the use of health technologies only in the context of an appropriately designed programme of evidence development. Health Technol Assess. 2012;16:1–323.
Reddy M, Gill SS, Kalkar SR, Wu W, Anderson PJ, Rochon PA. Treatment of pressure ulcers: a systematic review. JAMA. 2008;300:2647–62.
Pham B, Stern A, Chen W, Sander B, John-Baptiste A, Thein HH, Gomes T, Wodchis WP, Bayoumi A, Machado M, et al. Preventing pressure ulcers in long-term care: a cost-effectiveness analysis. Arch Intern Med. 2011;171:1839–47.
McKenna C, Claxton K. Addressing adoption and research design decisions simultaneously: the role of value of sample information analysis. Med Decis Mak. 2011; 31:853–865.
Eckermann S, Willan AR. Expected value of information and decision making in HTA. Health Econ. 2007;16:195–209.
Grutters JP, van Asselt MB, Chalkidou K, Joore MA. Healthy decisions: towards uncertainty tolerance in healthcare policy. Pharmacoeconomics. 2014;33(1):1–4. doi:10.1007/s40273-014-0201-7
Dias S, Sutton AJ, Welton NJ, Ades AE. Evidence synthesis for decision making 3: heterogeneity–subgroups, meta-regression, bias, and bias-adjustment. Med Decis Making. 2013;33:618–40.
Willan AR, Eckermann S. Optimal clinical trial design using value of information methods with imperfect implementation. Health Econ. 2010;19:549–61.
Allman RM, Goode PS, Burst N, Bartolucci AA, Thomas DR. Pressure ulcers, hospital complications, and disease severity: impact on hospital costs and length of stay. Adv Wound Care. 1999;12:22–30.
Scott IA, Brand CA, Phelps GE, Barker AL, Cameron PA. Using hospital standardised mortality ratios to assess quality of care–proceed with extreme caution. Med J Aust. 2011;194:645–8.
Isaia G, Bo M, Tibaldi V, Scarafiotti C, Ruatta C, Michelis G. The experience of a geriatric hospital at home service for acutely ill elderly patients with pressure ulcers. Wounds. 2010;22:121–6.
Brandeis GH, Morris JN, Nash DJ, Lipsitz LA. The epidemiology and natural history of pressure ulcers in elderly nursing home residents. JAMA. 1990;264:2905–9.
Acknowledgments
The authors would like to thank Professor Karl Claxton for his advice regarding EVSI calculations. Haitham Tuffaha is supported by a National Health and Medical Research Council PhD scholarship through the Centre for Research Excellence in Nursing Interventions for Hospitalised Patients. The authors declare no conflict of interest.
Author contributions
Shelly Roberts and Wendy Chaboyer contributed to the development of the model structure and advised the clinical component of the study. Haitham Tuffaha, Louisa Gordon and Paul Scuffham conducted the cost-effectiveness and value of information analyses. All authors contributed to the writing and revision of the manuscript. Haitham Tuffaha is the guarantor for the overall content of the paper.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
EVPI [34]
-
1.
Assigned probability distributions to the input parameters in the mode as summarised in Table 1 in the main text.
-
2.
Sampled random values k times (eg, k = 10,000) from the distributions described above for each intervention.
-
3.
Calculated the mean NB for each intervention across all simulations, and identified the preferred baseline decision, that is, the intervention with the maximum expected mean NB (\( \max_{i} E_{\theta } {\text{NB}}\left( {i,\theta } \right) \)).
-
4.
Calculated the NB for each intervention and identified the optimal intervention at each simulation.
-
5.
Averaged the NBs from the identified optimal interventions in Step 4 (\( E_{\theta } \max_{i} {\text{NB}}\left( {i,\theta } \right) \)).
-
6.
EVPI per-patient is the difference between the average NBs in steps 5 and 3.
EVPPI [34]
Steps 1–3 as in EVPI algorithm detailed above, then:
-
4.
Sampled θ I once from its joint prior distribution (outer-level simulation).
-
5.
Fixed θ I at their sampled values θ Ik and simulate the other remaining uncertain parameters θ Cjk (eg, j = 1,000 times), allowing them to vary according to their conditional probability distribution on θ I at its sampled value θ Ik (inner-level simulation).
-
6.
Calculated the conditional expected NB of each intervention by evaluating the NB at each (θ Cjk, θ Ik) and averaging (\( E_{{\left( {\theta_{C} |\theta_{I} } \right)}} {\text{NB}}\left( {i,\theta_{I} ,\theta_{C} } \right) \)).
-
7.
Identified the intervention that has the highest estimated expected NB given the sampled value for the parameters of interest (θ Ik) from step 6.
-
8.
Repeated steps 4–7 k times (eg, k = 1,000) and calculate the average NB of the preferred interventions identified in step 7 (\( E_{{\theta_{I} }} \max_{i} E_{{\left( {\theta_{C} |\theta_{I} } \right)}} {\text{NB}}\left( {i,\theta_{I} ,\theta_{C} } \right) \)
-
9.
EVPPI is the difference between the average NBs in Steps 8 and 3.
EVSI
To estimate the EVSI for the relative risk (RR) of pressure ulcer with nutritional support (NS) compared to standard care (SC), we assumed that parameters θ NS and θ SC represent the probability of pressure ulcers with nutritional support and standard care, respectively. We followed the algorithm adapted from the algorithm reported in Ades 2004 [33].
Steps 0–3 as in EVPI algorithm above, then:
-
4.
Simulated the variety of possible results of proposed data collection:
-
4.1
Drew a sample from the prior distribution of the RR. The logRR ~Normal (μ 0, τ 0) where μ 0 is logRR in the meta-analysis and τ 0 is its variance.
-
4.2
Drew a sample baseline parameter θ SC from its prior distribution: θ SC~ beta (a, b) where a is the number of patients who developed pressure ulcers and b is the number of patients who did not develop pressure ulcers in the control arm of the meta-analysis.
-
4.3
Transformed back to obtain an implied prior for θ NS : θ NS = θ SCexp(logRR)
-
4.1
-
5.
-
5.1
Drew a sample sufficient statistic D, in this case a Binominal numerator, for each arm in the future trialwith size n, assuming equal size arms: r SC ~ Binomial(θ SC, n) and r NS ~ Binomial(θ NS, n)
-
5.2
Converted the sufficient statistics to a mean andvariance using the normal approximation:
μ D = log[r NS × n/r SC × n],
τ D = [(n − r SC)/(r SC × n) + (n − r NS)/(r NS × n)]−1
-
5.1
-
6.
Updated the prior with the new simulated data to obtain parameters of the posterior distribution:
logRR|D ~ Normal((μ 0 × τ 0 + μ D ,τ D )/(τ 0 + τ D ), τ 0 + τ D )
To allow EVSI calculation using TreeAge software, steps 4–6 were performed using Microsoft Excel and repeated 1,000 times generating a ‘coda’ of updated distributions (outer loop). This coda was then transferred to TreeAge for sampling:
-
7.
Carried out a nested Monte Carlo simulation (inner loop) drawing 1,000 samples from each posterior distribution of the parameters logRR|D in the Excel coda and from the prior distributions of θ c, and identified the intervention that has the highest estimated expected NB.
-
8.
Calculated the average NB of the preferred interventions identified in Step 7.
-
9.
The EVSI is the difference between the average NBs in Steps 8 and 3.
Rights and permissions
About this article
Cite this article
Tuffaha, H.W., Roberts, S., Chaboyer, W. et al. Cost-Effectiveness and Value of Information Analysis of Nutritional Support for Preventing Pressure Ulcers in High-risk Patients: Implement Now, Research Later. Appl Health Econ Health Policy 13, 167–179 (2015). https://doi.org/10.1007/s40258-015-0152-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-015-0152-y