Abstract
Several continuous cardiac output (CO) monitoring systems have been developed. None are ideal for use in anaesthesia or critical care. They all lack precision as shown by Bland–Altman studies. However, some provide reliable CO trending, which is useful for guiding fluid optimization protocols. The key issue is which systems are reliable, and this has not been helped by a lack of understanding of validation statistics in the literature. Recent studies suggest that none of the current intra-arterial pulse contour systems trend CO reliably. Stroke volume variability may provide a reliable alternative. Strangely, Nexfin finger plethysmography did reliably trend CO during routine surgery, but not during critical care. BioReactance also appears to trend CO acceptably, but its performance is affected by certain types of surgery that alter the pathways of electrical flux. Oesophageal Doppler is now well established for guiding goal-directed fluid regimens, and its trending of CO changes seems reliable.
Similar content being viewed by others
Introduction
Measuring cardiac output (CO) provides a wealth of circulatory information about the patient that is not provided by standard heart rate, blood pressure and pulse oximetry recordings alone. Insights into the patient’s peripheral circulation (i.e., systemic vascular resistance) and oxygen delivery are just two of the important hemodynamic parameters that can be determined. However, towards the goal of achieving reliable continuous CO, slow progress has been made since the first continuous CO monitor, the BoMed, was introduced in the late 1980s [1]. The aim of this article is to summarize what is known about the reliability of continuous CO technology available today and provide an insight into its use, but first one needs to be provided with some background information as to the shortcomings of studies aimed at evaluating this technology.
Historical Perspective
Any article that reviews continuous CO monitoring should mention the BoMed, because its introduction into clinical practice highlighted many of the inherent problems we face today with developing reliable continuous CO monitoring systems [2]. The BoMed was an electrical impedance device. It was used by placing ten ECG electrodes on the patient’s neck and chest. It measured resistance changes across the thorax during the cardiac cycle, which it used as a surrogate of blood flow. Therefore, it did not measure blood flow directly. It still is not totally agreed upon what the BoMed actually measured, but probably cyclical expansions of the aorta due to changing blood pressure [3]. The BoMed was the first automated device that measured CO on a beat-to-beat basis at the bedside. Thus, it was the first commercially available continuous CO monitor. Previously, CO was measured intermittently over several cardiac cycles using manually performed techniques such as injecting cold saline when performing thermodilution measurement. The BoMed was much more simple and convenient to use. Unfortunately, the BoMed was never accepted into clinical practice because it proved to be too inaccurate and unreliable. Its calibration required calculating the volume of the electrical flux that passed across the thorax, and this measurement was too imprecise and led to inaccuracies [4]. Furthermore, changes in its measurements could occur due to accumulation of lung water, changes in peripheral resistance and surgery within the upper abdomen [5–7].
The introduction of the BoMed also coincided with the arrival of the Bland–Altman method to assess bias and precision in clinical measurement studies, and replaced the commonly misinterpreted regression and correlation method [8]. All these shortcomings of the BoMed, (a) surrogate measurements, (b) poor calibration, (c) influenced by secondary factors and (d) use of Bland–Altman statistics, still affect us today in our search for a reliable, simple to use, point-of-care continuous CO monitor.
The last two decades have witnessed the introduction of a number of new CO technologies: (a) Doppler ultrasound, (b) pulse contour analysis, (c) bioreactance and (d) modified Fick or partial carbon dioxide rebreathing method, (e) pulse transit time analysis and (f) modifications of the single bolus thermodilution method using the pulmonary artery catheter [9∙∙]. None of these new technologies have proved to be totally satisfactory, but are supported by medical equipment companies who market commercially available devices based on these technologies (Table 1).
The only truly reliable continuous CO monitor is an aortic flow probe, as it measures CO directly from the vessel as blood leaves the heart. Modern day probes detects blood flow using an ultrasonic beam which transverses the vessel. The same technology is used to measure flow in silicon pipes. However, flow probes are far from the ideal CO monitor because surgery is required to place the probe around the aorta, so its use is restricted to animal research [10].
Shortcomings of Evaluation Studies
Reliable evaluation studies are an important part of the process of determining whether a new healthcare device will be a success. One of the main obstacles to reliable evaluation of continuous CO technology has been the lack of a reliable reference method and this has created a degree of uncertainty when interpreting the outcomes of CO evaluation studies. Single bolus thermodilution using a pulmonary artery catheter has been regarded for many years as the gold standard in clinical CO measurement and thus is the reference method of choice. However, single bolus thermodilution does not measure CO continuously, and its readings are not sufficiently accurate to provide a truly reliable evaluation. The precision (i.e., 95 % confidence intervals) of thermodilution measurements is quoted as ±20 % [11] and recent data suggests these limits could be even wider [12]. A true gold standard like the aortic flow probe has a precision of less than ±5 %. Although the pulmonary artery catheter is made to a high degree of precision, when placed in vivo its readings are susceptible to further and unpredictable errors because of uncertainty about correct positioning within the pulmonary circulation, poor injection technique, dead space effects and calculating the area under the thermodilution curve [13]. Furthermore, different monitoring systems introduce different degrees of error [14]. Stated simply, we currently do not have a reliable method of measuring CO in the clinical setting against which we can evaluate our new and emerging CO technology.
A further limitation of many CO validation studies has been the tendency to limit analysis to Bland–Altman comparisons. Although Bland–Altman analysis provides information about the accuracy of readings, it provides very little information about the devices ability to follow changes in CO consistently, or trending ability, which is the key attribute needed for continuous CO monitoring. The statistical methods needed to properly assess trending ability have only very recently been described in the literature [15], and as a result trending had only been assessed in a small proportion of CO validation studies [16∙∙]. To assess trending ability, one needs to collect serial CO data from the new and reference methods as CO changes. Fluid or vasopressor challenges can be used to create CO changes. A new variable that shows the change in value is generated, ∆CO, and statistical comparisons are performed using ∆CO plotted on the four quadrant graph with calculation of the concordance rate.
As a consequence of these shortcomings, many continuous CO monitors have been marketed using data that failed to support their clinical reliability.
Current Statistical Benchmarks
The main statistical method used to validate CO monitors is comparison with single bolus thermodilution by Bland–Altman and calculating the percentage error, a parameter calculated from the limits of agreement of the analysis over the mean CO which is expressed as a percentage. Percentage error was described first by the principal author of this review in 1999 [11]. Assuming that thermodilution has a precision of ±20 %, to equal or better this by the new method, it is now widely agreed that the percentage error should be <30 %. There has been much recent debate about the 30 % benchmark in the CO monitoring literature as many validation studies have provided percentage errors way above 30 % [12, 17].
However, percentage error only addresses accuracy and provides no assessment of trending ability, which is essential information for evaluating continuous CO monitoring. The author’s group has recently published a review of the literature on assessment of CO trending [16∙∙]. The conclusion and generally accepted consensus was that serial CO data should be collected and plotted as ∆CO on a four quadrant plot. After exclusion of central zone data, or statistical noise, the concordance rate should be calculated (i.e., percentage of ∆CO pairs that agree in direction of change). The authors recommended using a benchmark of > 92 % for recommending good trending ability. This methodology has now been adopted in many recent publications on the topic.
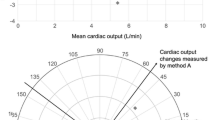
Using directional change as a determinant of good trending ability does have limitations, as important information about the magnitude of change in CO is lost. The author’s group has recently suggested converting the data to polar coordinates and showing the comparisons on a polar diagram [18]. The statistical background and methods for analyzing CO validation data have recently been published by the author as a chapter in an open access book [19].
Review of Available Systems
The main continuous CO systems being used today can be categorized into (a) the multifunction advanced pulmonary artery catheter; (b) the arterial pulse contour analysis system of which there are several, including a subset of noninvasive methods; (c) the bioimpedance method and its hybrids, including bioreactance; and (d) the Doppler ultrasound method, which is semi-continuous because of need for frequent refocusing (Table 1). The partial carbon dioxide rebreathing method (i.e., NICO) is now seldom used or reported.
Multifunction Thermodilution Catheters
A pulmonary artery catheter that used a heated wire wrapped around its intra cardiac section and upstream of the thermistor was developed in the 1990s, and provided continuous CO readings as opposed to single bolus [20]. Edwards and a few other catheter manufacturers now sell multifunction pulmonary artery catheters that provide this type of continuous CO monitoring, as well as mixed venous saturation monitoring, amongst other functions. Edwards sell the Vigilance II system (Edwards Lifesciences, Irvine, CA, USA). The clinical performance of the continuous CO catheter system has been evaluated in the past, and its accuracy was close to that of single bolus thermodilution [13]. The main limitation has been its slow response time, taking over 5 min to calculate CO, and thus has proved not to be that useful when used to detect dynamic changes in CO [21]. With its associated risks, the need for intra cardiac placement limits use to ultra-major surgery and critical care settings.
Pulse Contour Analysis
The concept of measuring continuous CO from an arterial line trace is simple and thus attractive. It first became clinically possible in the 1990s. Algorithms were developed that converted blood pressure to flow and several commercial systems were developed (Table 1). Sun et al. [22] described nine different CO equations, which included: (a) area under the arterial pressure waveform (i.e., PiCCO), (b) pulse pressure (i.e., FloTrac/Vigileo), (c) power or RMS (i.e., root mean squared) (i.e., LiDCO), (d) Windkessel model (i.e., Finapres) [23] and (e) inclusions of decay or extrapolated diastolic flow (i.e., PRAM). Sun et al. [22] favoured the Liljestrand–Zander formula, which is not used by any of the more popular systems. The pulse contour systems available today all use different algorithms and thus vary in their performance. However, none of these systems have yet been shown to be sufficiently reliable when clinical conditions change. The main difficulty has been adjusting for peripheral resistance changes. Although early validation studies in cardiac surgery patients supported the use of pulse contour technology, a number of more recent studies, such as in liver transplant patients with cirrhosis [15, 24] and response to vasopressors [25∙], have shown pulse contour analysis to be unreliable when challenged by major circulatory effects. However, the inability of validation studies to comprehensively evaluate these monitors’ performance has largely covered up the issue.
FloTrac/Vigileo
The most widely investigated pulse contour monitoring system has been the FloTrac/Vigileo (Edwards LifeSciences, Irvine, CA, USA), reflecting the heavy investment policy of Edwards to market the system [26]. However, two notable studies by Biais et al. [24] and then by Biancofiore et al. [15] subsequently revealed a lack of reliability of the FloTrac/Vigileo when peripheral vascular tone changed. As a result, the software was upgraded from version 1.10–3.02 (i.e., Dynamic Tone Technology). However, although version 3.02 performed better in a second, very similar in design study by Biancofiore et al. [27] that compared it to single bolus thermodilution in liver transplant patients, validation data still did not support its clinical use. Data from validation studies performed since continue to fall short of the benchmark [26]. FloTrac/Vigileo technology might still play a useful clinical role to guide fluid optimization during surgery or in critically ill patients using stroke volume variation (SVV) measurement with positive pressure ventilation [28].
LiDCO System
Lithium dilution was introduced as an alternative to thermodilution for measuring CO, and it does provide accurate and reliable CO readings [29]. It has become the main reference standard used in veterinary research and clearly has a market in this area [30]. An arterial pulse contour analysis system based on pulse power was combined with lithium dilution to provide continuous CO measurement for clinical use in a device called the LiDCO–PulseCO (LiDCO Group PLC., London, England). The system was initially designed to be calibrated by lithium or thermo dilution CO, but this proved too complicated for routine clinical use, and a self-calibrating system, the LiDCO-rapid was developed. The available data validating clinical use of the LiDCO-rapid is very limited. Hadian et al. [31] compared the three main pulse contour systems, LiDCO, PiCCO and FloTrac/Vigileo, to thermodilution in 17 post-cardiac surgery patients. Although the percentage error between the LiDCO-rapid and thermodilution was within the accepted benchmark of 29 %, the system had been initially calibrated by thermodilution, so statistical coupling was present, which reduces the magnitude of the percentage error. The other two systems had percentage errors against thermodilution of 41 % (n.b. also initially calibrated against thermodilution) and 59 %, respectively. Trending of the LiDCO-rapid against thermodilution was also poor, with a concordance rate of 74 % (i.e., below the 92 % benchmark). Also of concern was the wide disparity in agreement and trending that was found between these three pulse contour methods. Davies et al. [32] recently compared the LiDCO-rapid performance to the FloTrac/Vigileo and oesophageal Doppler in 20 high-risk surgery patients receiving goal-directed fluid therapy. Neither of two pulse contour systems showed any meaningful agreement with oesophageal Doppler as stroke volume increased. Only the stroke volume variability (i.e., SVV) from the LiDCO had any clinical utility. However, despite the lack of validation data that confirms its reliability—and in truth the LiDCO-rapid is no different from the FloTrac/Vigileo in terms of reliability—the LiDCO is one of the technologies together with oesophageal Doppler that is now being recommended by NICE in the UK to guide fluid therapy in high-risk surgery patients [33].
PRAM-MostCare
The pressure recording analytical method (PRAM) was developed in the mid 2000s in Italy [34]. It is marketed as the MostCare (Vytech Health, Padova, Italy), and is the latest of arterial line trace systems to be introduced. It differs from the other pulse contour systems, because it (a) measures and utilizes the diastolic part of the arterial pressure wave, and (b) it does not requiring any start-up information to calibrate the system. Its validation has provided mixed results. Franchi et al. [35] compared the MostCare to thermodilution in 30 septic shock patients, raising the blood pressure with noradrenaline, and found a percentage error of 25 % and concordance rate of 100 %, which indicated excellent agreement and trending abilities. However, other authors have found much less favourable agreement. Also in septic patients, Gopal et al. [36] reported a percentage error of 64 % and Paarmaan et al. reported a percentage error of 87 % in cardiac surgery patients. Thus, the verdict is still out on the reliability of the MostCare.
PiCCO System
The PiCCO system (Pulsion Medical Systems, Munich, Germany) is used differently compared to the other three pulse contour systems discussed so far. The PiCCO was developed from the Cold system for measuring blood volumes and lung water. It uses a femoral arterial catheter that doubles up as a transpulmonary thermodilution CO catheter. Thus, it can be periodically recalibrated using thermodilution, and in between calibrations it runs in continuous CO mode, estimating CO from the femoral artery trace. Therefore, accuracy against thermodilution is less of an issue. A study by Yamashita et al. [37] in 20 cardiac surgery patients in whom the vasodilator prostaglandin E1 was infused, and that compared uncalibrated PiCCO to thermodilution, showed that PiCCO lacked reliability when systemic vascular resistance decreased. Therefore, the PiCCO needs recalibration against thermodilution whenever the peripheral circulatory conditions are changed. A more recent comparison by Bendjelid et al. [38] of the FloTrac/Vigileo as part of the new VolumeView/EV1000 system (Edwards LifeSciences, Irvine, CA, USA) and the PiCCO system against transpulmonary thermodilution showed the VolumeView to be more accurate in Bland–Altman comparisons, 29 versus 37 % respectively, and trended CO changes, though both concordance rates, 81 and 77 % respectively, were well below the 92 % benchmark. Thus, the PiCCO needs frequent recalibration with thermodilution and does not accurately trend CO in adverse conditions. However, it is the pulse contour method that is most established in the critical care setting, and its ability to recalibrate using thermodilution CO greatly improves its reliability and utility.
Noninvasive Pulse Contour Monitoring
Nexfin
Pulse contour analysis CO can also be performed noninvasively using a finger cuff, rather than directly from an intra-arterial catheter and transducer. A cuff pneumatically clamps the blood flow in the finger using a photocell servo-system, and tracks blood pressure changes in the digital artery [39, 40]. The method was developed in the late 1980s and was marketed as the Ohmeda Finapres BP monitor (TNO Biomedical Instruments, the Netherlands). Cardiac output monitoring was later added using a method called model flow [22]. A range of portable (i.e., the Portapres) and bedside (i.e., the Finometer) versions was later produced by the marketing company BMEYE. The most recent version of this technology is the Nexfin, which was recently acquired by Edwards LifeSciences.
Several recent and well-designed clinical studies comparing the Nexfin to thermodilution or Doppler CO have been published. Thus, lessons were learned from the deficiencies of past validation studies. Trending was assessed by fluid challenge or vasopressor administration (i.e., phenylephrine). Chen et al. [41] compared the Nexfin to oesophageal Doppler in 25 abdominal or orthopaedic surgery patients and found a poor percentage error of 37 %, but a good concordance rate following phenylephedrine of 94 % with convincing polar plots that also showed trending. Hofhuizen et al. [42] compared the Nexfin to transpulmonary thermodilution in 20 post cardiac surgery patients and found a poor percentage error of 39 %, but good concordance rate following fluid challenge of 100 %. Bubenek-Turconi et al. [43] compared the Nexfin to single bolus thermodilution in 22 post cardiac surgery patients and found a percentage error of 38 % and concordance rate following fluid challenge or passive leg raise of 100 %, also with convincing polar plots. These three studies suggest that despite the Nexfin having poor agreement with the reference method (i.e., percentage error of 37–39 % and above the 30 % benchmark), the Nexfin did follow changes in CO reliably (i.e., concordance rates above the 92 % benchmark and convincing polar plots), but it should be noted that all these three studies were limited to intraoperative use. Potentially, based on these recent results that show reliable trending, the Nexfin could have a future role in monitoring the response of CO to fluid and vasopressor therapy during surgery. However, in the critical care setting, recent studies show that the Nexfin does not trend CO reliably [44, 45]. In the Monnet et al. [44] study, the concordance rate was 84 % . Volume responsiveness was also assessed using receiver operator characteristic (ROC) curve analysis. In the Taton et al. [45] study, trend analysis was based purely on volume responsiveness and ROC curves. It is also noteworthy that in several patients from these studies, the Nexfin failed to function properly and data could not be collected. Thus, the quality of figure cuff tracings from some critically ill patients may affect the performance of the Nexfin. The finger plethysmography method that the Nexfin uses detects the blood pressure waveform from a more distal part of the arterial tree compared to intra-arterial blood pressure CO monitoring (i.e., radial and femoral artery sites). As arterial tone is determined by the arterioles that lie between these central arteries and the periphery, and these arterioles are the main determinant of systemic vascular resistance, the better reliability of trending found in studies investigating the finger cuff method is of some note. If true, the finger may prove to be a better site from which to model the circulation and measure continuous CO, at least during anaesthesia.
CNAP Monitor 500
CNSystems also produce a noninvasive finger cuff continuous blood pressure monitor, the CNAP Monitor 500 (CNSystems, Graz, Austria), which is currently being promoted. It also provides continuous pulse wave CO monitoring. Previously, the company had based its continuous CO monitoring on a bioimpedance method (i.e., the Task Force Monitor). The authors are unaware of any published work to date having evaluated the CNAP monitor 500.
Bioimpedance Technology
BioReactance
BioReactance is a hybrid of bioimpedance that uses frequency modulation or phase shift to improve its reliability and performance. Four sets of surface electrodes are used to detect the bioreactance signal generated within the thorax. The method is currently utilised by a continuous CO monitor called the NICOM (Cheetah Medical, Tel Aviv, Israel). It was developed just over 5 years ago and received Food and Drug Administration (FDA) approval in 2008. Several animal and human studies were performed between 2006 and 2007 to confirm that the method worked [46–48]. In a joint animal ( nine pigs) and human (27 postoperative patients) study by Keren et al., the NICOM was shown to have good correlation (r = 0.87) against flow probe over CO ranging from 1 to 5 L/min and trending on time and four-quadrant plots. Results in humans against thermodilution (r = 0.9) were equally good [46]. More recently in five beagle dogs, Heerdt et al. [49] have also shown good trending against flow probe, albeit with a 30-second time lag for data averaging.
What has yet to be shown is whether these encouraging trend data results from animal studies translate to the clinical setting, such as patients undergoing major surgery and receiving anaesthetic care. Recent, yet to be published data by the authors of this review comparing the NICOM to Doppler CO intra-operatively show that Bioreactance does track changes in CO reliably during surgery, but with one major caveat: provided that the geometry of the patient's thorax and upper abdomen, and thus the pathways of electrical flux, are not affected by; (a) surgical incisions, (b) placement of metal retractors or (c) the diaphragm being displaced up into the chest by abdominal distention during laparoscopy, as significant but predictable shifts in the calibration occur that alter trending. Similar effects were reported when using the BoMed intra-operatively [7]. An observational study by Conway et al. [50] comparing bioreactance (i.e., NICOM) and oeosophageal Doppler (i.e., CardioQ) readings in 21 major abdominal surgery patients reported a poor precision error of 57 % and a marginal concordance rate of 90.5 % following fluid challenge. What was most interesting about the paper was its Fig. 1, which plotted stroke volume against time from one case. After 14 min, there was clear shift in bias of 30 ml between the two CO devices. We repeatedly found this pattern when surgical manoeuvers that clearly would affect the electrical flux pathways of the NICOM were performed. Thus, the NICOM may prove to be a viable intra-operative continuous CO monitor, providing that the intra-operative surgical factors that alter its calibration are fully recognized, and their effects on bioreactance measurements understood.
Other bioimpedance devices are also marketed, but are less often encountered in anaesthesia and critical care settings. The BioZ (CardioDynamics, San Diego, CA, USA), a digitalized continuation of BoMed technology, is still being produced and has FDA approval. The Aesculon and Icon (Osypka Medical, San Diego, CA, USA) are bedside and portable hybrid bioimpedance continuous CO monitors, respectively. They use the acceleration rather than flow derivatives of the impedance signal. Clinical validation studies are not available, but data testing the methodology in the animal laboratory is available [51]. Like all emerging continuous CO technologies, these devices also target a use in fluid optimization intra-operatively or in critical care.
Pulse Wave Transit Time
Cardiac output can also be estimated from the pulse wave measured peripherally by pulse oximetry. The size of the pulse wave varies with changes in stroke volume. The transit time for the pulse wave to reach the periphery is also used, as it varies with arterial tone and thus can be used to adjust for peripheral resistance. By integrating the ECG and pulse oximetry signal, the transit time can be determined. A Japanese technology known as estimated continuous cardiac output (esCCO) has been developed which measures continuous CO by this method [52]. The technology has recently been marketed by Nihon Kohden (Nihon Kohden Corporation, Tokyo, Japan) and has been incorporated into their new multifunction cardiac monitor.
All the original published work on developing esCCO system can be attributed to Ishihara and colleagues from Japan [52]. These authors have also performed the only multicentre (seven centres) validation study to date comparing esCCO to single bolus thermodilution [53]. In 139 intensive care and 74 operating room patients, the percentage error was 54 %, which was no better in respect to accuracy than the other CO systems discussed in this review (Table 1). A polar plot analysis of their data was later performed, and this also did not support good trending ability [54]. Very recently Tsutsui et al. [55] published data from 31 partial hepatectomy patients. Although the percentage error was absent from the article, these authors did show reasonable trending between esCCO and thermodilution following fluid boluses and vasopressor administration, their concordance rate being 96 %. Whether using transit time improves the ability of pulse wave analysis to cope with variations in the system vascular resistance has yet to be determined. Despite the poor results from some studies, esCCO technology is currently being promoted by Nihon Kohden.
Doppler Ultrasound Devices
Doppler CO can be measured either externally via the anterior chest wall or by a probe place in the oesophagus and aimed at the descending aorta. Echocardiography, whether transthoracic or oesophageal, can be used to measure CO with Doppler mode, but it does not measure CO continuously and performing repeated measurements of CO is not very convenient. However, there are two Doppler devices currently marketed that are designed for the job and use continuous wave Doppler. They are the CardioQ (Deltex Medical Ltd., Chichester, England) and the USCOM (USCOM Ltd., Sydney, Australia). Neither device is truly continuous in nature. The CardioQ has an oesophageal probe that needs to be periodically refocused [56]. The USCOM is used intermittently by focusing a handheld probe on the aortic or pulmonary valve. Reading are saved and displayed on a time plot that shows trends over time [57]. Neither device can be set up at the bedside to monitor CO continuously, but they can be used guide fluid and vasopressor therapies by performing frequent measurements.
The CardioQ, like all the current continuous technologies, does not measure true CO accurately. Most of its validation data pre-date percentage error, and in Dark and Singer’s meta-analysis, a statistic called “percentage of clinical agreement” (PCA) based on the number of data pairs that were within ±15 % of mean bias was used [58]. Re-evaluation of data from this paper using mean CO and limits of agreement shows that the percentage error for many of these oesophageal Doppler studies was 40–50 %. However, the CardioQ does seem to track changes in CO, although there is little published data other than that found in a study by Valtier et al. [59]. These authors found good trending ability with a concordance rate on the four quadrants plot against bolus thermodilution of 93 %.
The USCOM also does not measure true CO accurately. Clinical validation data for the USCOM is more recent than the CardioQ and most studies are Bland–Altman in design. A recent meta-analysis by Chong and Peyton of USCOM validation studies found an overall percentage error of 43 %, which is similar to that of the CardioQ [60]. However, trending ability has been only confirmed in animal studies against an aortic flow probe [61].
Unlike the arterial pulse contour methods where modeling the circulation is required to produce an algorithm that converts pressure changes to blood flow, ultrasound measures blood flow directly. Therefore, providing that the quality of readings is acceptable, Doppler should faithfully reflect changes in CO, whereas pulse contour analysis can be distorted by changes in peripheral. Therefore, one would expect more stable and reliable CO trend data from these two Doppler systems.
Goal Directed Therapy
CO-driven goal directed therapy is being promoted in both anaesthesia and critical care. Oesophageal Doppler is currently being promoted to drive goal-directed fluid therapy protocols in high-risk surgery cases [33]. Changes in stroke volume are mainly used to drive protocols based on Doppler. However, similar protocols using pulse contour or bioreactance systems have been less successful. As a result, the focus has changed when using the non-Doppler CO technologies to measuring stroke volume variation (i.e., SVV) and pulse pressure variation (i.e., PPV), which are also reliant on intermittent positive pressure ventilation of the lungs. The stability of arterial pressure and bioreactance-based recording systems facilitates the measurement of SVV, which appears to be very robust. In contrast, Doppler methods that rely on handheld probes or regular refocusing of an oesophageal probe produce much less reliable SVV data, and their SVV should not be used to guide therapy.
Conclusions
None of the currently available continuous CO monitors are accurate, or precise. However, some do reliably trend CO changes in studies, and thus can be used to optimise fluid and vasopressor therapy. The most promising technologies are Doppler and possibly bioreactance and the Nexfin, though understanding where and when they can be used is paramount. Alternative measures such as stroke volume variation (SVV) also offer a solution to using some of these monitors successfully.
References
Papers of particular interest, published recently, have been highlighted as: ∙ Of importance ∙∙ Of major importance
Bernstein DP. Continuous noninvasive real-time monitoring of stroke volume and cardiac output by thoracic electrical bioimpedance. Crit Care Med. 1986;14(10):898–901.
Critchley LA. Evaluation of a cardiac output monitor (chapter 14). In: Cannesson M, Pearse R, editors. Perioperative hemodynamic monitoring and goal directed therapy. Cambridge: Cambridge University Press; 2014. p. 120–131
Kubicek WG. On the source of peak first time derivative (dZ/dt) during impedance cardiography. Ann Biomed Eng. 1989;17(5):459–62.
Critchley LA. Impedance cardiography. The impact of new technology. Anaesthesia. 1998;53(7):677–84.
Peng ZY, Critchley LA, Fok BS. An investigation to show the effect of lung fluid on impedance cardiac output in the anaesthetized dog. Br J Anaesth. 2005;95(4):458–64.
Critchley LA, et al. The effect of peripheral resistance on impedance cardiography measurements in the anesthetized dog. Anesth Analg. 2005;100(6):1708–12.
Critchley LA, Leung DH, Short TG. Abdominal surgery alters the calibration of bioimpedance cardiac output measurement. Int J Clin Monit Comput. 1996;13(1):1–8.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
∙∙ Marik, P.E., Noninvasive cardiac output monitors: a state-of the-art review. J Cardiothorac Vasc Anesth. 2013;27(1):121–34. This article provides an excellent review of the CO technology.
Peng Z, Critchley L, James A. Comparison of blunt versus surgical dissection for aortic flow probe placement in the dog. Scand J Lab Anim Sci. 2006;33(4):227–35.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15(2):85–91.
Peyton PJ, Chong SW. Minimally invasive measurement of cardiac output during surgery and critical care: a meta-analysis of accuracy and precision. Anesthesiology. 2010;113(5):1220–35.
Reuter DA, et al. Cardiac output monitoring using indicator-dilution techniques: basics, limits, and perspectives. Anesth Analg. 2010;110(3):799–811.
Yang XX, Critchley LA, Joynt GM. Determination of the precision error of the pulmonary artery thermodilution catheter using an in vitro continuous flow test rig. Anesth Analg. 2011;112(1):70–7.
Biancofiore G, et al. Evaluation of an uncalibrated arterial pulse contour cardiac output monitoring system in cirrhotic patients undergoing liver surgery. Br J Anaesth. 2009;102(1):47–54.
∙∙ Critchley, L.A., A. Lee, and A.M. Ho, A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111(5):1180–92. This article outlines the study design and statistics needed to show trending ability of a CO monitor.
Michard F. Thinking outside the (cardiac output) box. Crit Care Med. 2012;40(4):1361–2.
Critchley LA, Yang XX, Lee A. Assessment of trending ability of cardiac output monitors by polar plot methodology. J Cardiothorac Vasc Anesth. 2011;25(3):536–46.
Critchley LA. Minimally invasive cardiac output monitoring in the Year 2012 (chapter 4). In: Aronow WS, editor. Arterial bypass. Rijeka, Croatia: InTech; 2013. p. 45–80.
Yelderman M. Continuous measurement of cardiac output with the use of stochastic system identification techniques. J Clin Monit. 1990;6(4):322–32.
Mihm FG, et al. A multicenter evaluation of a new continuous cardiac output pulmonary artery catheter system. Crit Care Med. 1998;26(8):1346–50.
Sun JX, et al. The cardiac output from blood pressure algorithms trial. Crit Care Med. 2009;37(1):72–80.
Wesseling KH, et al. Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol (1985). 1993;74(5):2566–73.
Biais M, et al. Cardiac output measurement in patients undergoing liver transplantation: pulmonary artery catheter versus uncalibrated arterial pressure waveform analysis. Anesth Analg. 2008;106(5):1480–6 table of contents.
∙ Meng L, et al. The impact of phenylephrine, ephedrine, and increased preload on third-generation Vigileo-FloTrac and esophageal doppler cardiac output measurements. Anesth Analg. 2011;113(4):751–7. This article very nicely showed how vasopressors adversely affected FloTrac readings.
Slagt C, Malagon I, Groeneveld AB. Systematic review of uncalibrated arterial pressure waveform analysis to determine cardiac output and stroke volume variation. Br J Anaesth. 2014;112(4):626–37.
Biancofiore G, et al. Evaluation of a new software version of the FloTrac/Vigileo (version 3.02) and a comparison with previous data in cirrhotic patients undergoing liver transplant surgery. Anesth Analg. 2011;113(3):515–22.
Scheeren TW, et al. Goal-directed intraoperative fluid therapy guided by stroke volume and its variation in high-risk surgical patients: a prospective randomized multicentre study. J Clin Monit Comput. 2013;27(3):225–33.
Linton R, et al. Lithium dilution cardiac output measurement: a comparison with thermodilution. Crit Care Med. 1997;25(11):1796–800.
Axiak Flammer SM, et al. Reliability of lithium dilution cardiac output in anaesthetized sheep. Br J Anaesth. 2013;111(5):833–9.
Hadian M, et al. Cross-comparison of cardiac output trending accuracy of LiDCO, PiCCO, FloTrac and pulmonary artery catheters. Crit Care. 2010;14(6):R212.
Davies SJ, et al. Comparison of stroke volume and fluid responsiveness measurements in commonly used technologies for goal-directed therapy. J Clin Anesth. 2013;25(6):466–74.
National Institute for Health and Clinical Excellence. Medical technologies guidance MTG3: CardioQ-ODM oesophageal Doppler monitor. http://www.nice.org.uk/MTG3. Accessed March 2011.
Scolletta S, et al. Pressure recording analytical method (PRAM) for measurement of cardiac output during various haemodynamic states. Br J Anaesth. 2005;95(2):159–65.
Franchi F, et al. Comparison between an uncalibrated pulse contour method and thermodilution technique for cardiac output estimation in septic patients. Br J Anaesth. 2011;107(2):202–8.
Gopal S, et al. Validation of cardiac output studies from the Mostcare compared to a pulmonary artery catheter in septic patients. Minerva Anestesiol. 2014;80(3):314–23.
Yamashita K, et al. The effects of vasodilation on cardiac output measured by PiCCO. J Cardiothorac Vasc Anesth. 2008;22(5):688–92.
Bendjelid K, et al. Performance of a new pulse contour method for continuous cardiac output monitoring: validation in critically ill patients. Br J Anaesth. 2013;111(4):573–9.
Penaz J. Photoelectric measurement of blood pressure, volume and flow in the finger. In: Digest of the 10th international conference on medical and biological engineering, Dresden; 1973.
Imholz BP, et al. Continuous non-invasive blood pressure monitoring: reliability of Finapres device during the Valsalva manoeuvre. Cardiovasc Res. 1988;22(6):390–7.
Chen G, et al. Comparison of noninvasive cardiac output measurements using the Nexfin monitoring device and the esophageal Doppler. J Clin Anesth. 2012;24(4):275–83.
Hofhuizen C, et al. Validation of noninvasive pulse contour cardiac output using finger arterial pressure in cardiac surgery patients requiring fluid therapy. J Crit Care. 2014;29(1):161–5.
Bubenek-Turconi SI, et al. Noninvasive continuous cardiac output by the Nexfin before and after preload-modifying maneuvers: a comparison with intermittent thermodilution cardiac output. Anesth Analg. 2013;117(2):366–72.
Monnet X, et al. The estimation of cardiac output by the Nexfin device is of poor reliability for tracking the effects of a fluid challenge. Crit Care. 2012;16(5):R212.
Taton O, et al. Evaluation of cardiac output in intensive care using a non-invasive arterial pulse contour technique (Nexfin((R))) compared with echocardiography. Anaesthesia. 2013;68(9):917–23.
Keren H, Burkhoff D, Squara P. Evaluation of a noninvasive continuous cardiac output monitoring system based on thoracic bioreactance. Am J Physiol Heart Circ Physiol. 2007;293(1):H583–9.
Raval NY, et al. Multicenter evaluation of noninvasive cardiac output measurement by bioreactance technique. J Clin Monit Comput. 2008;22(2):113–9.
Squara P, et al. Noninvasive cardiac output monitoring (NICOM): a clinical validation. Intensive Care Med. 2007;33(7):1191–4.
Heerdt PM, et al. Noninvasive cardiac output monitoring with bioreactance as an alternative to invasive instrumentation for preclinical drug evaluation in beagles. J Pharmacol Toxicol Methods. 2011;64(2):111–8.
Conway DH, Hussain OA, Gall I. A comparison of noninvasive bioreactance with oesophageal Doppler estimation of stroke volume during open abdominal surgery: an observational study. Eur J Anaesthesiol. 2013;30(8):501–8.
Osthaus WA, et al. Comparison of electrical velocimetry and transpulmonary thermodilution for measuring cardiac output in piglets. Paediatr Anaesth. 2007;17(8):749–55.
Ishihara H, et al. A new non-invasive continuous cardiac output trend solely utilizing routine cardiovascular monitors. J Clin Monit Comput. 2004;18(5–6):313–20.
Yamada T, et al. Multicenter study verifying a method of noninvasive continuous cardiac output measurement using pulse wave transit time: a comparison with intermittent bolus thermodilution cardiac output. Anesth Analg. 2012;115(1):82–7.
Ishihara H, et al. The ability of a new continuous cardiac output monitor to measure trends in cardiac output following implementation of a patient information calibration and an automated exclusion algorithm. J Clin Monit Comput. 2012;26(6):465–71.
Tsutsui M, et al. Pulse wave transit time measurements of cardiac output in patients undergoing partial hepatectomy: a comparison of the esCCO system with thermodilution. Anesth Analg. 2013;117(6):1307–12.
Singer M, Clarke J, Bennett ED. Continuous hemodynamic monitoring by esophageal Doppler. Crit Care Med. 1989;17(5):447–52.
Critchley LA, Huang L. USCOM-window to the circulation: utility of supra-sternal Doppler in an elderly anaesthetized patient for a robotic cystectomy. J Clin Monit Comput. 2014;28(1):83–93.
Dark PM, Singer M. The validity of trans-esophageal Doppler ultrasonography as a measure of cardiac output in critically ill adults. Intensive Care Med. 2004;30(11):2060–6.
Valtier B, et al. Noninvasive monitoring of cardiac output in critically ill patients using transesophageal Doppler. Am J Respir Crit Care Med. 1998;158(1):77–83.
Chong SW, Peyton PJ. A meta-analysis of the accuracy and precision of the ultrasonic cardiac output monitor (USCOM). Anaesthesia. 2012;67(11):1266–71.
Critchley LA, et al. Testing the reliability of a new ultrasonic cardiac output monitor, the USCOM, by using aortic flowprobes in anesthetized dogs. Anesth Analg. 2005;100(3):748–53.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Critchley, L.A.H., Huang, L. & Zhang, J. Continuous Cardiac Output Monitoring: What Do Validation Studies Tell Us?. Curr Anesthesiol Rep 4, 242–250 (2014). https://doi.org/10.1007/s40140-014-0062-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-014-0062-9