Abstract
Worldwide, 200 million adults undergo major noncardiac surgery every year, and approximately 8 million of these patients will suffer a myocardial injury after noncardiac surgery (MINS). MINS is defined as a prognostically relevant myocardial injury due to ischemia that occurs during or within 30 days after noncardiac surgery. The diagnostic criterion for MINS is an elevated troponin measurement resulting from myocardial ischemia. MINS is an independent predictor of 30-day and 1-year mortality. Without troponin monitoring, the majority of MINS events will go undetected because >80 % of patients suffering from MINS do not experience ischemic symptoms. Guideline committees have recently recommended monitoring perioperative troponin measurements in high-risk patients having noncardiac surgery. Risk-adjusted observational data suggest aspirin and a statin can reduce the risk of 30-day mortality in patients who have experienced MINS.
Similar content being viewed by others
Introduction
Noncardiac surgery has the potential to dramatically improve a patient’s quality of life (e.g., arthroplasty) and prolong life (e.g., oncological surgery). The number of patients undergoing noncardiac surgery has substantially increased throughout the last few decades because of surgical advances, the shift toward advanced care for the elderly, and the increase in life expectancy. Worldwide, 200 million adults have major noncardiac surgery every year [1]. Despite the benefits of noncardiac surgery, patients having surgery are at risk of serious complications. Myocardial injury is one of the more common and serious perioperative complications. In this article, we explore the prognostic impact of an elevated perioperative troponin measurement and the concept of myocardial injury after noncardiac surgery (MINS).
Prognostic Impact of an Elevated Troponin Measurement after Noncardiac Surgery on 30-Day and 1-Year Outcomes
The VISION study was a large international prospective cohort study of 40,000 patients undergoing in-hospital noncardiac surgery assessing major complications after surgery. VISION was conducted in several countries, and the recruitment was completed in September 2013. Patients of at least 45 years of age and undergoing major noncardiac surgery requiring hospital admission were enrolled. Patients having urgent, emergent, or elective surgeries occurring during weekdays and weekends were included. The primary outcome was all-cause mortality at 30 days after surgery. During the hospital admission, troponin T (TnT) levels were measured at 6–12 h and on days 1 through 3 after surgery. Throughout the trial, an experienced research team closely monitored the patients for major postoperative complications. Also, the research personnel contacted patients for follow-up at 30 days and at 1 year.
Analyses were performed on the first 15,133 patients in the VISION Study who had a fourth-generation TnT perioperative measurement [2••]. A Cox proportional hazard model was performed with mortality until 30 days as the dependent variable and 24 preoperative variables as independent variables. This model was repeated and included the peak fourth-generation TnT measurement during the first 3 days after surgery as an independent variable. A statistical approach was used to determine whether there was a threshold(s) at which TnT independently predicted 30-day mortality.
Peak TnT values of 0.01 ng/ml or less, 0.02, 0.03–0.29, and 0.3 ng/ml or more occurred in 88.4, 3.3, 7.4, and 0.9 % of the patients, respectively. The overall mortality at 30 days was 1.9 %. The peak TnT threshold values of 0.02, 0.03, and 0.30 ng/ml were independently associated with 30-day mortality. These analyses demonstrated that the strongest predictor of 30-day mortality after noncardiac surgery was an elevated TnT value after surgery. The population attributable risk analysis suggested that elevated TnT measurements after surgery may explain 41.8 % of the deaths. The incidence of 30-day mortality was 1.0, 4.0, 9.3, and 16.9 % in patients with peak TnT values of 0.01 or less, 0.02, 0.03 to 0.29, and 0.30 ng/ml or greater, respectively. Further, patients with TnT values independently associated with mortality revealed the following median times from the peak TnT measurements to death: 0.02 ng/ml [13.5 days; interquartile range (IQR), 8.5–20 days]; 0.03 to 0.29 ng/ml (9.0 days; IQR, 3.5–16 days); 0.30 ng/ml or greater (6.5 days; IQR, 1.5–15 days), P = 0.01 for differences among time to death.
Therefore, VISION clearly demonstrated that elevated TnT values after noncardiac surgery have strong prognostic capabilities in terms of 30-day mortality. Moreover, this study showed that the higher the peak troponin value is, the shorter median time to death.
Elevated troponin values after noncardiac surgery also impact 1-year mortality. In fact, Levy et al. [3•] undertook a systematic review and meta-analysis to evaluate the prognostic value of troponin and creatinine kinase-myocardial band measurement after noncardiac surgery. The analysis used 14 studies and included 3,318 patients and 459 deaths. Ten studies evaluating the impact of an increased troponin measurement on intermediate-term (≤12 months) mortality showed an OR = 6.7 (95 % CI 4.1–10.9). The relationship of an elevated perioperative troponin measurement to long-term (≥12 months) mortality was assessed in four studies and demonstrated an adjusted OR = 1.8 (95 % CI 1.42.3, I2 = 0 %). Hence, these findings demonstrate that an increased troponin measurement after noncardiac surgery is a strong predictor of 1-year mortality. Moreover, this systematic review also included five studies that evaluated the impact of an elevated troponin level after noncardiac surgery on major cardiovascular complications. All five studies demonstrated that an elevated troponin measurement after surgery was an independent predictor of a major cardiovascular event in the subsequent 6–18 months.
Myocardial Injury after Noncardiac Surgery (MINS)
Most noncardiac surgery studies interested in cardiovascular complications focus on perioperative myocardial infarction. Recently, the joint task force of the European Society of cardiology (ESC), American College of Cardiology (ACC) Foundation, American Heart Association (AHA), and World Heart Federation published the Third Universal definition and diagnostic criteria of myocardial infarction (MI). MI was defined as myocardial necrosis from myocardial ischemia, and the diagnostic criteria consist of troponin elevation with either cardiac symptoms or electrocardiography (ECG) changes suggestive of acute myocardial ischemia [4•, 5–7].
Diagnosing MI based on the universal definition may be a challenge in the perioperative setting. The majority of patients with perioperative MI do not experience ischemic cardiac symptoms, mainly because of analgesics. In POISE, only 34.7 % of patients with perioperative MI experienced an ischemic symptom [8]. Further, ischemic ECG changes after surgery are uncommon. Since no cardiac symptom is reported by patients, ECGs are not performed when cardiac ischemia is occurring. ECGs are typically done after troponin elevation, which can be several hours after the cardiac insult. Therefore, in patients with perioperative MI, a minority of ECGs will show ischemic changes [8]. Consequently, many patients with myocardial injury do not satisfy the diagnostic criteria for MI in the perioperative period [9].
Although the noncardiac surgery community has primarily focused on MI in the perioperative setting for compelling reasons (e.g., the universal definition is well known and referenced), some authors advocate moving to the concept of myocardial injury for several reasons [9]. First, the universal definition of MI excludes many prognostically relevant perioperative myocardial ischemic events [10••]. Then, some prognostically relevant perioperative myocardial insults may represent myocardial injury as opposed to myocardial necrosis (as required by the universal definition of MI) [2••, 11]. Lastly, a new diagnosis may minimize the risk that individuals will assume that what is known about nonoperative myocardial infractions (e.g., pathophysiology, treatment) automatically applies to these perioperative myocardial events.
For these reasons, the VISION investigators recently proposed a new definition of MINS [12••]. MINS is defined as the following: myocardial injury caused by ischemia (that may or may not result in necrosis), having prognostic relevance (i.e., independently impacts the risk of 30-day mortality), and occurring during or within 30 days after noncardiac surgery. The proposed definition of MINS is broader than the universal definition of myocardial infraction in that it includes other prognostically relevant perioperative myocardial injuries due to ischemia in addition to MI. MINS does not include perioperative myocardial injury due to a documented nonischemic etiology (e.g., pulmonary embolism, sepsis, cardioversion). Based on the statistical analyses performed on the VISION data, the diagnostic criterion for MINS is a peak TnT ≥ 0.03 ng/ml that is judged to be a result of myocardial ischemia without evidence of a nonischemic etiology causing the troponin elevation.
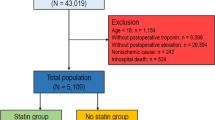
Two independent physicians adjudicated all troponin elevation measurements in VISION. They determined the timing of the troponin elevation (i.e., before or after the surgery), the presence of any ischemic symptoms or ischemic ECG changes, and the presence of a nonischemic etiology that could result in troponin elevation. Both adjudicators had to come to an agreement regarding whether there was any evidence supporting a nonischemic etiology for the troponin elevation. In VISION, 1,200 patients (8.0 %; 95 % CI, 7.5–8.4) ≥45 years of age who underwent noncardiac surgery fulfilled the MINS diagnostic criterion. Globally, it is estimated that 100 millions of adults over the age of 45 years undergo noncardiac surgery annually [1]. Accordingly, the VISION findings suggest that at least 8 million adults will suffer MINS on a yearly basis.
The VISION investigators also established predictors, characteristics, and 30-day outcomes of MINS. Independent preoperative predictors of MINS were identified in a multivariable regression analysis. Predictors included: age ≥ 75 years, male sex, current atrial fibrillation, history of diabetes, hypertension, congestive heart failure, coronary artery disease, high-risk coronary artery disease, peripheral vascular disease, stroke, a preoperative estimated glomerular filtration rate <60 ml/min/1.73 m2, and urgent/emergent surgery.
Characteristics of MINS were also described in VISION. The majority (87 %) of MINS occurred within the first 3 days after surgery. Among patients with MINS, only 15.8 % experienced ischemic cardiac symptoms. Therefore, without postoperative troponin monitoring, 84 % of the MINS events would go undetected. Furthermore, in VISION, all patients experiencing an elevated troponin measurement had an ECG. Only 34.9 % of the patients had ischemic ECG changes. The most common ischemic ECG findings were T waves inversion (23.3 %) and ST depression (16.4 %). As previously stated, ischemic ECG changes are most likely missed because of lack of cardiac symptoms and timing of the detected troponin elevation (i.e., troponin level increases several hours after the initial cardiac injury).
Given how infrequently cardiac symptoms and ischemic ECG changes are detected in patients suffering from MINS, only a minority (41.8 %) of patients experiencing MINS fulfill the universal definition of MI (Fig. 1), which requires ischemic symptoms or ECG findings in addition to an elevated troponin measurement. VISION established that MINS events that do not fulfill the universal definition of MI (i.e., 58.2 % of MINS patients) are not benign events. These events have an adjusted hazard ratio of 3.3 for 30-day mortality.
Based on VISION analysis, patients suffering from MINS have a 30-day mortality rate of 10 %, as opposed to 1 % in patients without MINS. Also, a multivariable analysis that took into account other perioperative complications suggests 34 % of the deaths during the first 30 days after surgery were due to MINS. Further, MINS not only increased 30-day mortality risk, but also impacted the 30-day risk of nonfatal cardiac arrest (odds ratio = 14.48), congestive heart failure (odds ratio = 10.34), and stroke (odds ratio = 4.66). Table 1 compares the incidence of major postoperative vascular events between patients with MINS and those without.
The VISION investigators have developed a scoring system to predict 30-day mortality in patients suffering from MINS. Multivariable analyses identified three independent predictors of mortality among MINS patients: age ≥ 75 years (1 point), ST elevation or new left bundle branch block (2 points), and an anterior ischemic electrocardiographic finding (1 point). Patients with a score of 0, 1, 2, 3, or 4 had an expected 30-day mortality rate of 5.2 % (95 % CI, 3.3–7.4), 10.2 % (95 % CI, 6.5–11.9), 19.0 % (95 % CI, 8.7–24.3), 32.5 % (95 %, 10.6–45.9), and 49.8 % (95 % CI, 12.0–65.5), respectively.
Based on these observations, we advocate assessing surgical patients for the diagnosis of MINS given its prognostic value. Although no randomized controlled trial (RCT) has established an effective treatment for patients suffering from MINS, the prognosis of these patients is likely modifiable.
What Can We Do about Perioperative Myocardial Ischemia
Although there is debate regarding the pathophysiology of MINS [13], evidence suggests that at least a substantial proportion of these events are due to coronary artery thrombus formation [14]. Surgery creates an ideal milieu for coronary thrombosis through many factors including inflammation and a hypercoagulability state. Mechanical tissue injury during surgery and the acute stress induce a hypercoagulable-inflammatory state that increases the risk of coronary thrombus formation [14]. Hypercoagulability is further promoted by sympathetic hyperactivity associated with surgery, which causes upregulation of coagulation and platelets and downregulation of fibrinolysis [15–17]. Sympathetic activation leads to catecholamine release, which is associated with an increase in coronary shear stress. This may trigger plaque fissuring and acute coronary thrombosis [18]. The risk of acute thrombosis is enhanced in the presence of endothelial dysfunction associated with coronary artery disease and in the presence of circulating catecholamines that induce a paradoxical vasoconstriction [18]. Inflammation associated with noncardiac surgery also results in an increase in tumor necrosis factor α (TNF-α), interleukin (IL)-6, and IL-8 [13]. These cytokines may have a direct role in initiating plaque fissuring and acute coronary thrombosis [13]. This evidence suggests that antithrombotic and antiinflammatory medications may benefit patients suffering from MINS.
Knowing this, it is also important to realize that patients suffering from MINS are almost universally underdiagnosed and undertreated, despite having a poor prognosis [10••, 19–22]. This difference in the intensity of treatment is likely influenced by several factors including: (1) a majority of patients suffering from MINS do not experience ischemic symptoms [10••, 23], potentially influencing physicians’ perception of the severity of the event; (2) there is debate about the pathophysiology of MINS [13] (although emerging evidence does suggest that coronary arterial thrombosis is an important mechanism of MINS) [14]; (3) no RCT has evaluated an intervention to manage MINS, and hence physicians are uncertain about the risk:benefit ratio of potential interventions (e.g., interventions that are effective in the management of nonoperative MI) [14].
In patients suffering from MINS in the POISE trial, some had an increase in their usage of cardiovascular drugs compared to their preoperative usage, but at hospital discharge only 65 % of patients were taking acetyl-salicylic acid, 18 % were taking clopidogrel or ticlopidine, 52 % were taking a statin, and 55 % were taking an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin-receptor blocker [10••]. Full-dose anticoagulation was also uncommon (11.8 %) among patients suffering from MINS. Further, a minority of patients suffering from MINS underwent coronary revascularization (7.9 %).
Multivariable analyses among patients suffering from MINS in the POISE Trial demonstrated that two drugs (i.e., ASA and a statin) were associated with a statistically significant, risk-adjusted reduction in 30-day mortality. Although these data are observational, several points suggest there is a high likelihood that these drugs will benefit patients suffering from MINS. First, there is overwhelming evidence regarding the benefits of ASA and a statin in secondary prevention including patients who have suffered a nonoperative MI. Second, a majority of MINS patients have atherosclerotic disease [24]. Third, it is usually the recurrent cardiac event that happens in the weeks after a MINS event that results in a patient’s demise, and it is highly probable that these recurrent events are thrombotic in nature.
Importantly, clinical trials are starting to evaluate methods to improve the outcome of patients suffering from MINS. One international trial (MANAGE) is currently evaluating the impact of an anticoagulant (i.e., dabigatran 110 mg BID) versus placebo; using a partial factorial design, this trial is also evaluating omeprazole 20 mg daily versus a placebo. More trials are needed.
Guidelines for Monitoring Troponins
In order to manage MINS, physicians must be able to appropriately identify patients who have suffered MINS. In most cases troponin elevation is in the only manifestation of MINS. Therefore, without troponin monitoring, most of these events would go undetected.
In line with this evidence, the Third Universal Definition of Myocardial Infarction now recommends perioperative troponin monitoring after noncardiac surgery. This expert consensus published by the ESC, ACC, AHA, and World Heart Foundation (WHF) Joint Task Force recommends routine monitoring of cardiac biomarkers in high-risk patients, both prior to and 48–72 h after major surgery [4•, 5–7]
UpToDate also recommends troponin monitoring as part of routine postoperative care for all patients at high cardiac risk [25]. They define high risk as patients undergoing high-risk surgery who have one or more additional risk factors on the revised cardiac risk index (i.e., history of ischemic heart disease, heart failure, or cerebrovascular disease, diabetes mellitus requiring treatment with insulin, and preoperative serum creatinine >2.0 mg/dl). In these high-risk patients, they suggest obtaining troponin at 6–12 h and days 1, 2, and 3 after surgery.
Conclusion
Myocardial injury is the most common major vascular complication after noncardiac surgery, and perioperative myocardial injury represents 15–20 % of all cases of MI in all settings. Many patients sustain myocardial injury in the perioperative period that will not satisfy the diagnostic criteria for MI. Recent evidence supports the introduction of a new diagnosis of MINS that may be useful to patients and clinicians.
Patients suffering from MINS are two times more likely to die within 30 days than those with nonoperative MI in the emergency room; paradoxically, its treatment is less intensive. This difference in the intensity of treatment is likely influenced by several factors including that a majority of patients suffering from MINS do not experience ischemic symptoms, potentially influencing physicians’ perception of the severity of the event. In the POISE cohort, only approximately half of the patients suffering from MINS were prescribed cardioprotective medication at discharge, including aspirin, a statin, and an ACE inhibitor. Despite the suboptimal prescribing of these medications, there is evidence that suggests aspirin and a statin are beneficial and can reduce the 30-day risk of mortality in patients who have suffered MINS.
Troponins are in many cases the only marker available to help us identify and manage these patients. Given recent evidence regarding the prognostic relevance of MINS and the knowledge that a majority of patients don’t experience ischemic symptoms, several guidelines now suggest postoperative troponin monitoring. Given the magnitude of the problem, we believe there is an urgent need for clinical trials to identify effective therapies to improve the outcomes of patients suffering from MINS.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372:139–44.
•• Devereaux PJ, Chan MT, Alonso-Coello P, et al. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA : the journal of the American Medical Association 2012;307:2295–304. In patients undergoing noncardiac surgery, peak troponin T in the 1st postoperative days is the strongest independent predictor of 30 -day mortality.
• Levy M, Heels-Ansdell D, Hiralal R, et al. Prognostic value of troponin and creatine kinase muscle and brain isoenzyme measurement after noncardiac surgery: a systematic review and meta-analysis. Anesthesiology 2011;114:796–806. Postoperative troponin elevation is associated with a six-fold increase in mortality risk during the 1st year after noncardiac surgery.
• Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Journal of the American College of Cardiology 2012;60:1581–98. Postoperative routine screening of troponin after noncardiac surgery is now recommanded in at-risk patients as part of the of the third universal definition of myocardial infarction.
Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–67.
Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–35.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Third universal definition of myocardial infarction. Nat Rev Cardiol. 2012;9:620–33.
Devereaux PJ, Yang H, Yusuf S, et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371:1839–47.
Ali ZA, Callaghan CJ, Ali AA, et al. Perioperative myocardial injury after elective open abdominal aortic aneurysm repair predicts outcome. Eur J Vasc Endovasc Surg. 2008;35:413–9.
•• Devereaux PJ, Xavier D, Pogue J, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Annals of internal medicine 2011;154:523–8. In patients who had an increase in troponin after noncardiac surgery, aspirin and statin therapy is associated with a significant risk reduction of 30-day mortality.
Hickman PE, Potter JM, Aroney C, et al. Cardiac troponin may be released by ischemia alone, without necrosis. Clin Chim Acta. 2010;411:318–23.
•• Botto F, Alonso-Coello P, Chan MT, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 2014;120:564–78. Introduction, implication, and prognostic relevance of a new diagnostic entity: myocardial injury after noncardiac surgery (MINS).
Devereaux PJ, Goldman L, Cook DJ, Gilbert K, Leslie K, Guyatt GH. Perioperative cardiac events in patients undergoing noncardiac surgery: a review of the magnitude of the problem, the pathophysiology of the events and methods to estimate and communicate risk. CMAJ. 2005;173:627–34.
Devereaux PJ, Chan M, Eikelboom J. Major vascular complications in patients undergoing noncardiac surgery: The magnitude of the problem, risk prediction, surveillance, and prevention. In: Yusuf S, Cairns JA, Camm AJ, Fallen EL, Gersh BJ, editors. Evidence based Cardiology. 3rd ed. London: BMJ Books; 2009. p. 47–62.
von Kanel R, Dimsdale JE. Effects of sympathetic activation by adrenergic infusions on hemostasis in vivo. Eur J Haematol. 2000;65:357–69.
von Kanel R, Mills PJ, Ziegler MG, Dimsdale JE. Effect of beta2-adrenergic receptor functioning and increased norepinephrine on the hypercoagulable state with mental stress. Am Heart J. 2002;144:68–72.
Yun AJ, Lee PY, Bazar KA. Can thromboembolism be the result, rather than the inciting cause, of acute vascular events such as stroke, pulmonary embolism, mesenteric ischemia, and venous thrombosis?: a maladaptation of the prehistoric trauma response. Med Hypotheses. 2005;64:706–16.
Priebe HJ. Triggers of perioperative myocardial ischaemia and infarction. Br J Anaesth. 2004;93:9–20.
Devereaux PJ, Chan MTV, Alonso-Coello P, et al. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2012;307:2295–304.
Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–65.
Mandelzweig L, Battler A, Boyko V, et al. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–93.
Jernberg T, Johanson P, Held C, Svennblad B, Lindback J, Wallentin L. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA. 2011;305:1677–84.
Devereaux PJ, Goldman L, Yusuf S, Gilbert K, Leslie K, Guyatt GH. Surveillance and prevention of major perioperative ischemic cardiac events in patients undergoing noncardiac surgery: a review. CMAJ. 2005;173:779–88.
Gualandro DM, Campos CA, Calderaro D, et al. Coronary plaque rupture in patients with myocardial infarction after noncardiac surgery: frequent and dangerous. Atherosclerosis. 2012;222:191–5.
http://www.uptodate.com/contents/perioperative-myocardial-infarction-after-noncardiac-surgery.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bessissow, A., Duceppe, E. & Devereaux, P.J. Addressing Perioperative Myocardial Ischemia. Curr Anesthesiol Rep 4, 107–112 (2014). https://doi.org/10.1007/s40140-014-0060-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-014-0060-y