Abstract
Introduction
The purpose of this study was to determine whether the outcomes following placement of a fluocinolone acetonide implant (Retisert®; Bausch & Lomb, Inc.) combined with an Ahmed™ glaucoma valve (New World Medical, Inc.) in eyes with uveitic glaucoma (UG Retisert) were different when compared to an Ahmed valve alone in eyes with uveitic glaucoma or primary open angle glaucoma (UG non-Retisert and POAG, respectively).
Methods
Retrospective, interventional study of consecutive uveitic and OAG eyes undergoing Ahmed valve (AV) implantation with or without combined Retisert insertion at a single academic center between 2009 and 2012. Surgical success was defined as intraocular pressure (IOP) between 5 and 18 mmHg and greater than 20% reduction of IOP at two consecutive visits without need for additional IOP-lowering medications or surgical procedures. Secondary outcome measures included IOP and number of glaucoma medications.
Results
Sixty eyes of 60 patients (22 UG Retisert, 16 UG non-Retisert, 22 POAG) were included. Mean ± standard deviation surgical success duration was significantly greater in UG Retisert eyes, 629 ± 53 days, compared to those with UG non-Retisert, 361 ± 37 days, and POAG, 472 ± 65 days (P = 0.034). At 24 months, the mean IOP was 11.7, 12.1, and 15.0 mmHg and the average patient was on 1.45, 0.71, and 2.00 medications in the UG Retisert, UG non-Retisert, and POAG valve groups, respectively.
Conclusion
Retisert implants when combined with AV in uveitic glaucoma had a longer duration of surgical success than uveitic or POAG treated with AV insertion alone.
Similar content being viewed by others
Introduction
Secondary glaucoma is a common problem in eyes with uveitis, and elevated intraocular pressure (IOP) occurs in 11–46% of eyes with chronic uveitis [1–4]. Uveitic glaucoma can be difficult to treat because of the relatively young mean patient age, diverse pathogenic factors, prolonged use of topical corticosteroids, and limited tolerance to medical therapies [5]. Accordingly, many patients ultimately require glaucoma surgery to achieve long-term stability [5, 6]. Glaucoma drainage devices are increasingly becoming the preferred procedure in these patients [7].
The sustained-release intravitreal fluocinolone acetonide implant (Retisert®; Bausch & Lomb, Inc., Rochester, NY, USA) was approved in 2005 by the US Food and Drug Administration on the basis of two prospective multicenter randomized pivotal trials to treat eyes with noninfectious posterior uveitis [8–10]. The Retisert implant produces sustained intraocular corticosteroid delivery for up to 36 months. However, 70% of the Retisert-implanted eyes showed susceptibility to steroid-induced increased IOP and 33.8% required surgery as reported recently [11]. In another study, the Retisert-implanted eyes had about a fourfold risk of developing IOP elevation of ≥10 mmHg and incident glaucomatous optic neuropathy compared with those assigned to systemic immunosuppressive therapy for uveitis [12].
Glaucoma drainage devices have been fairly effective in IOP control in eyes with uveitic glaucoma [5]. However, in eyes with uveitic glaucoma requiring treatment with simultaneous Retisert implant and glaucoma drainage devices, the long-term IOP control may be limited due to chronic steroid delivery. The purpose of this study was to determine the outcomes of Ahmed™ valve implant (New World Medical, Inc., Rancho Cucamonga, CA, USA) combined with a Retisert in eyes with uveitic glaucoma and compare that to results in eyes with uveitic glaucoma and primary open angle glaucoma (POAG) treated with an Ahmed valve implant alone.
Methods
This study was approved by the Duke University Institutional Review Board and adhered to the tenets of the declaration of Helsinki. A retrospective record review was conducted of consecutive patients with uveitic glaucoma evaluated at the Duke Eye Center between September 2009 and September 2012 in whom a Retisert implant and Ahmed valve were inserted at the same surgical session (‘UG Retisert’ group). Patients underwent Retisert implantation if either their uveitis was considered uncontrolled with topical and systemic immunosuppressive therapy by their respective surgeon or were intolerant of systemic immunosuppressive therapy. Of these eyes, those that had either uncontrolled IOP (>21 mmHg) on maximum tolerated medical therapy or had a history of a IOP spike following a previous steroid injection (intravitreal or posterior subtenon’s) were scheduled to undergo an Ahmed implant simultaneously. Similar data were collected from records of patients seen during the same period with uveitic glaucoma and POAG (denoted ‘UG non-Retisert’ and ‘POAG’ groups, respectively). The eyes in these two groups underwent an Ahmed implant if they had uncontrolled IOP on maximum tolerated medical therapy. For all groups, eyes were excluded if they had undergone previous surgery to place a glaucoma drainage device or trabeculectomy or if they had undergone previous or concurrent vitreoretinal surgery. None of the patients in any group had a pars plana tube. The only prior intraocular surgery acceptable for inclusion was cataract extraction.
Data Collection
Baseline and follow-up clinical and intraoperative data were recorded in an electronic database. Clinical data collected included age at surgery, gender, operative eye, Ahmed valve model, prior or concurrent cataract extraction, best-corrected Snellen visual acuity (VA), IOP by applanation tonometry [either Tono-Pen applanation (Reichert, Inc., Depew, NY, USA) or Goldmann applanation (Haag Streit International, Mason, OH, USA)], systemic immunosuppressive therapy, use of topical steroids during pre- and postoperative periods, and number of glaucoma medications. Measurement points included a preoperative visit, intraoperative data, postoperative month one, postoperative month six, postoperative year one and postoperative year two.
Statistical Analysis
The primary outcome measure was surgical success, defined as IOP between 5 and 18 mmHg and greater than 20% reduction of IOP at two consecutive visits without loss of light perception, need for additional IOP-lowering surgical procedure, or removal of Ahmed valve for any reason. Secondary outcome measures included the level of IOP, number of glaucoma medications and best-corrected VA (BCVA) converted to the logarithm of the minimum angle of resolution (logMAR) units.
Descriptive statistics were computed at each time point for IOP (mmHg), number of medications, and VA (logMAR). Differences in means among and between groups were assessed using analysis of variance and the unpaired t test, respectively. Changes from baseline to postoperative values were assessed using the paired t test. Surgical success duration was compared among the three groups using Kaplan–Meier curves and the log-rank test. Data analysis was completed using SAS Statistical Analysis, version 9.3 (Cary, NC, USA).
Results
Preoperative Characteristics
A total of 60 eyes of 60 patients were included in the study. Simultaneous combined Retisert implantation and Ahmed valve placement was performed on 22 uveitic eyes. Ahmed valve alone was performed on 16 uveitic eyes and 22 POAG eyes during the study period. Baseline demographics and implant model are presented in Table 1. Fifty-nine percent of UG Retisert eyes underwent simultaneous cataract extraction, compared to 25% and 14% in the UG non-Retisert and POAG groups, respectively. The Retisert implant was performed by three vitreoretinal surgeons and the Ahmed implants were performed by four glaucoma surgeons. Of note, there was a significant difference in mean ages in the three groups (P < 0.001) and all pair-wise comparisons of age between groups were also significantly different (P < 0.006). Of the eyes in the UG Retisert group, 11 were on no systemic immunotherapy. Of the remaining 11 eyes that were on systemic immunosuppressive therapy, 7 stopped such therapy following the Retisert implant and 4 were continued on such therapy for systemic reasons. Such therapy included medications such as methotrexate, oral prednisone, hydroxychloroquine, etanercept, and mycophenolate mofetil. Only one of the eyes of the UG non-Retisert group was being treated with oral immunosuppressive therapy, which was continued postoperatively. All the eyes in both the UG Retisert and UG non-Retisert groups were on varying doses of topical prednisolone prior to surgery and were continued on a slow tapering schedule till discontinuation 8–10 weeks after the surgery. Six eyes of each of these groups remained on either once or twice a day of chronic postoperative topical prednisolone therapy. However, none of the eyes of the POAG group received steroids preoperatively and all stopped topical steroids 4–5 weeks post-surgery. The mean preoperative IOP was significantly higher in the UG non-Retisert group (32.5 mmHg) compared to the POAG group (29.2 mmHg, P = 0.024). Preoperative IOP was similar in the UG non-Retisert and UG Retisert (26.7 mm Hg) groups (P = 0.643). All eyes were typically on three glaucoma medications prior to surgery in all groups. The mean logMAR preoperative BCVA was significantly worse in the UG Retisert group (−1.17) as compared to both the uveitic valve and POAG valve groups (−0.63 and −0.76, respectively; P = 0.005 and P = 0.017, respectively).
Surgical Success
By Kaplan–Meier survival analysis, there was a significant difference in the duration of surgical success among the UG Retisert compared to both the UG non-Retisert and POAG groups (P = 0.034). The mean surgical success duration was greater in the UG Retisert group (629 ± 53 days) compared to the UG non-Retisert (361 ± 37 days) and the POAG valve (472 ± 65 days) groups. The cumulative probability of success at 1 year was 84%, 63%, and 61% for the UG Retisert, UG non-Retisert, and POAG groups, respectively. The cumulative probability of success at 2 years was 67%, 54%, and 27% in the UG Retisert, UG non-Retisert, and POAG groups, respectively (Fig. 1). The predominant cause of failure in all groups was inadequate IOP control due to an IOP >18 mmHg or less than 20% reduction in IOP (Table 2). Success duration was not significantly different among different models of the Ahmed valve (FP7, M4, S2, or S3; P = 0.633, log-rank test). No complications associated with Retisert implantation were noted in this study.
Postoperative Intraocular Pressure
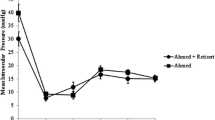
At 24 months postoperatively, the average IOP was 11.7, 12.1, and 15.0 in the UG Retisert, UG non-Retisert, and POAG groups, respectively. There was a trend towards significance when comparing the UG Retisert and POAG groups (P = 0.076) and achieving significance between the UG non-Retisert and POAG groups (P = 0.020). The difference in postoperative IOP between the two uveitic groups was not significant. In all three groups, the mean IOPs at all postoperative visits were significantly reduced compared to the preoperative IOP (P < 0.01 at all time points). The difference in IOP change between the two uveitic groups was not significant (Fig. 2). There was no significant difference in IOP or change in IOP when comparing uveitis anatomical location or etiology (P = 0.161–0.923).
Medications
The number of glaucoma medications decreased significantly from baseline in all groups at all postoperative visits (P < 0.018 at all points), with the exception of the POAG group at 24 months (P = 0.1). At 24 months, the average patient was on 1.45, 0.71, and 2.00 medications in the UG Retisert, UG non-Retisert, and POAG groups, respectively. There were fewer medications administered to eyes in the UG non-Retisert group as compared to the POAG group at 12 and 24 months postoperatively (P = 0.033, 0.058, respectively). There were no significant differences in the number of medications used in the UG non-Retisert and UG Retisert groups (P = 0.542 and 0.626 at 12 and 24 months; Fig. 3).
Visual Acuity
There were no significant changes in postoperative visual acuities in the UG non-Retisert and POAG groups at the postoperative visits as compared to baseline. However, the UG Retisert group obtained a significant improvement in VA at all time points (P < 0.037) likely due to the fact that 59% of UG Retisert eyes underwent simultaneous cataract extraction, compared to 25% and 14% in the UG non-Retisert and POAG groups, respectively.
Discussion
This study was designed as a retrospective series to evaluate the outcomes of Ahmed valve with or without combined simultaneous Retisert implantation in eyes with uveitic glaucoma and to compare the results to Ahmed valve in eyes with POAG. We found that (1) Retisert combined with simultaneous Ahmed valve implantation led to significantly longer success compared to Ahmed valve alone in eyes with uveitis or POAG; (2) Retisert combined with Ahmed valve did not lead to significant worsening of glaucoma control as suspected due to prolonged steroid release in uveitic eyes; and (3) eyes with uveitis had significantly better IOP control and needed fewer glaucoma medications following Ahmed valve than eyes with POAG.
Topical corticosteroids are well known to improve success in trabeculectomy surgery because they inhibit fibroblast proliferation, phagocytosis, and vascular permeability, and suppress the release of cytotoxic enzymes, growth, and chemotactic factors [13]. Several smaller series also suggest positive results with either preoperative or intraoperative subconjunctival steroid injection during trabeculectomy [14–16]. However, the role of steroids in the management of glaucoma drainage devices has not been well evaluated. In one study, intravitreal injection of triamcinolone acetonide in neovascular glaucoma did not improve the long-term success of the Ahmed valve [17]. In another recent small prospective randomized controlled trial, patients received intracameral triamcinolone at the end of either a trabeculectomy or glaucoma drainage device surgery [18]. The authors did not find any significant differences in IOP between groups at 6 months nor any differences in failure rate. However, the authors included three different types of glaucoma drainage devices in the study and did not analyze the drains separately from trabeculectomy. Further, the authors did not provide specific data on enrolled secondary glaucoma patients, including those with uveitic glaucoma.
Retisert implantation as a sole procedure has been well known to lead to elevated IOP as a complication [11, 12, 19]. However, we hypothesized that when combined with a glaucoma drainage device, the corticosteroids released by the Retisert into the vitreous cavity transit into the anterior chamber and through the glaucoma tube implant, thereby internally modifying the capsule surrounding the glaucoma implant plate and improving the surgical success rate. This could be due to a very low dose of sustained steroid delivery that perfuses the tissue around the plate, thus preventing the formation of a dense collagenous impervious capsule (which likely contributes to the hypertensive phase or failure of the Ahmed valve). Some small case series have also indicated that results are favorable in eyes with concurrent placement of glaucoma tube shunts and Retisert implants [20, 21]. The results of our study further support the role of combined Retisert and glaucoma tube implantation in selected eyes with uveitic glaucoma.
The literature supports the success of glaucoma drainage devices in uveitic glaucoma, with cumulative probability of success of 77–94.4% at 1 year and 50–80% at 2–4 years following Ahmed valve implantation, as assessed by Kaplan–Meier analysis [5, 22, 23]. The probability of success in our study was 84% at 1 year and 63% at 2 years in the UG Retisert and 63% at 1 year and 54% at 2 years in the UG non-Retisert groups. Though our results are similar to the reported series, there is no standard definition of success and different criteria have been used. The definition used in the current study combined both IOP reduction and complications. There are also reports of other types of glaucoma drainage devices in uveitic glaucoma, including four small series evaluating Molteno® implants (Molteno Ophthalmic Limited, Dunedin, New Zealand) in uveitic patients that found survival estimates between 80% and 95% at 27–48 months of follow-up [24–27]. A small retrospective study of Baerveldt® implantation (Abbott Laboratories Inc. Abbott Park, IL, USA) in uveitic eyes found cumulative life-table success rates were 95.8% at 3 months and 91.7% at 6–24 months [28]. However, another retrospective series evaluating the IOP results following Ahmed valve placement in uveitic as compared to POAG patients found significantly lower IOP in the uveitic group at 1 and 2 months, but no difference at 3–24 months; there was no significant difference in the cumulative success rates between the groups [29].
There are some possible explanations for the finding that uveitic eyes had lower IOP and fewer medications following glaucoma tube implant than those with POAG. Endogenous prostaglandin release plays a complex and poorly understood role in both uveitis and IOP [30], and may facilitate some of the success. It is also possible that uveitic eyes have long-term postoperative reduced aqueous production, although no known confirmatory literature exists.
The preoperative logMar BCVA was significantly worse in the UG Retisert group as compared to the other two, owing largely to the relative degree of media opacity and macular cystoid edema in this group. Fifty-nine percent of eyes in this group underwent simultaneous cataract extraction thus explaining the significantly improved BCVA postoperatively. Limited published data on cataract extraction in uveitic glaucoma patients or patients with prior tube shunts suggest possible short-term influence on IOP but no difference at 1–2 years [31, 32].
This study has several important limitations. It is retrospective, not randomized, and covers a relatively short study period. Since the Retisert implant typically releases steroid for approximately 3 years [20, 33], a longer term study that lasts 5 years might provide significant additional information. Uveitic glaucoma is a heterogeneous group of many inflammatory glaucoma etiologies and anatomic locations, which limits direct comparison among and between groups. There was a preoperative significant difference in IOP between the UG non-Retisert and POAG groups, representing a limitation in sample size. The choice to insert a Retisert implant was at the surgeon’s discretion, creating the potential for selection bias. Systemic immunosuppressive therapy was used preoperatively in the treatment of half the eyes in the UG Retisert group (11/22 eyes), which may have had an influence on the overall outcome of this group; however, only four eyes were exposed to systemic immunosuppressive therapy postoperatively.
Conclusions
This retrospective study found that Retisert combined with Ahmed valve in eyes with uveitic glaucoma resulted in longer surgical success compared to eyes with uveitic glaucoma or POAG treated with Ahmed valve insertion alone. Eyes with uveitic glaucoma had better IOP control and were on fewer medications following Ahmed valve placement than eyes with POAG. These data should compel further investigation to elucidate a reason for the differential response between groups, and if validated, would support prospective trials evaluating the expanded use of steroid implants in selected uveitic glaucomatous eyes undergoing drainage device placement.
References
Panek WC, Holland GN, Lee DA, Christensen RE. Glaucoma in patients with uveitis. Br J Ophthalmol. 1990;74:223–7.
Herbert HM, Viswanathan A, Jackson H, Lightman SL. Risk factors for elevated intraocular pressure in uveitis. J Glaucoma. 2004;13:96–9.
Neri P, Azuara-Blanco A, Forrester JV. Incidence of glaucoma in patients with uveitis. J Glaucoma. 2004;13:461–5.
Takahasi T, Ohtani S, Miyata K, et al. A clinical evaluation of uveitis-associated secondary glaucoma. Jpn J Ophthalmol. 2002;46:556–62.
Papadaki TG, Zacharopoulos IP, Pasquale LR, et al. Long-term results of Ahmed glaucoma valve implantation for uveitic glaucoma. Am J Ophthalmol. 2007;144:62–9.
Ansari H, Kempen JH. Proof of concept for combined insertion of fluocinolone acetonide and glaucoma drainage implants for eyes with uveitis and glaucoma. Am J Ophthalmol. 2010;149:699–700.
Landers J, Martin K, Sarkies N, et al. A twenty-year follow-up study of trabeculectomy: risk factors and outcomes. Ophthalmology. 2012;119:694–702.
Jaffe GJ, Ben-Nun J, Guo H, et al. Fluocinolone acetonide sustained drug delivery device to treat severe uveitis. Ophthalmology. 2000;107:2024–33.
Callanan DG, Jaffe GJ, Martin DF, et al. Treatment of posterior uveitis with a fluocinolone acetonide implant: three-year clinical trial results. Arch Ophthalmol. 2008;126:1191–201.
Pavesio C, Zierhut M, Bairi K, Fluocinolone Acetonide Study Group, et al. Evaluation of an intravitreal fluocinolone acetonide implant versus standard systemic therapy in noninfectious posterior uveitis. Ophthalmology. 2010;117:567–75.
Campochiaro PA, Nguyen QD, Hafiz G, et al. Aqueous levels of fluocinolone acetonide after administration of fluocinolone acetonide inserts or fluocinolone acetonide implants. Ophthalmology. 2013;120:583–7.
Friedman DS, Holbrook JT, Ansari H, MUST Research Group, et al. Risk of elevated intraocular pressure and glaucoma in patients with uveitis: results of the multicenter uveitis steroid treatment trial. Ophthalmology. 2013;120:1571–9.
Araujo SV, Spaeth GL, Roth SM, Starita RJ. A 10-year follow-up on a prospective, randomized trial of postoperative corticosteroids after trabeculectomy. Ophthalmology. 1995;102:1753–9.
Yuki K, Shiba D, Kimura I, et al. Trabeculectomy with or without sub-Tenon injection of triamcinolone acetonide in treating secondary glaucoma. Am J Ophthalmol. 2009;147:1055–60.
Giangiacomo J, Dueker DK, Adelstein E. The effect of preoperative subconjunctival triamcinolone administration on glaucoma filtration. I. Trabeculectomy following subconjunctival triamcinolone. Arch Ophthalmol. 1986;104:838–41.
Tham CC, Li FC, Leung DY, et al. Intrableb triamcinolone acetonide injection after bleb-forming filtration surgery (trabeculectomy, phacotrabeculectomy, and trabeculectomy revision by needling): a pilot study. Eye. 2006;20:1484–6.
Teixeira SH, Doi LM, Freitas Silva AL, et al. Silicone Ahmed glaucoma valve with and without intravitreal triamcinolone acetonide for neovascular glaucoma: randomized clinical trial. J Glaucoma. 2012;21:342–8.
Koval MS, Moster MR, Freidl KB. Intracameral triamcinolone acetonide in glaucoma surgery: a prospective randomized controlled trial. Am J Ophthalmol. 2014;158:395–401.
Kempen JH, Altaweel MM, Holbrook JT, Multicenter Uveitis Steroid Treatment (MUST) Trial Research Group, et al. Randomized comparison of systemic anti-inflammatory therapy versus fluocinolone acetonide implant for intermediate, posterior, and panuveitis: the multicenter uveitis steroid treatment trial. Ophthalmology. 2011;118:1916–28.
Malone PE, Herndon LW, Muir KW, Jaffe GJ. Combined fluocinolone acetonide intravitreal insertion and glaucoma drainage device placement for chronic uveitis and glaucoma. Am J Ophthalmol. 2010;149:800–6.
Ahmad ZM, Hughes BA, Abrams GW, Mahmoud TH. Combined posterior chamber intraocular lens, vitrectomy, retisert and pars plana tube in noninfectious uveitis. Arch Ophthalmol. 2012;130:908–13.
Da Mata A, Burk S, Netland PA, et al. Management of uveitic glaucoma with the use of Ahmed valve. Ophthalmology. 1999;106:2168–72.
Ozdal PC, Vianna RNG, Deschenes J. Ahmed valve implantation in glaucoma secondary to chronic uveitis. Eye. 2006;20:178–83.
Vuori ML. Molteno aqueous shunt as a primary surgical intervention for uveitic glaucoma: long-term results. Acta Ophthalmol. 2010;88:33–6.
Broadway DC, Iester M, Schulzer M, Douglas GR. Survival analysis for success of Molteno tube implants. Br J Ophthalmol. 2001;85:689–95.
Molteno AC, Sayawat N, Herbison P. Otago glaucoma surgery outcome study: long-term results of uveitis with secondary glaucoma drained by Molteno implants. Ophthalmology. 2001;108:605–13.
Valimaki J, Airaksinen PJ, Tuulonen A. Molteno implantation for secondary glaucoma in juvenile rheumatoid arthritis. Arch Ophthalmol. 1997;115:1253–6.
Ceballos EM, Parrish RK 2nd, Schiffman JC. Outcome of Baerveldt glaucoma drainage implants for the treatment of uveitic glaucoma. Ophthalmology. 2002;109:2256–60.
Rachmiel R, Trope GE, Buys YM, et al. Ahmed glaucoma valve implantation in uveitic glaucoma versus open-angle glaucoma patients. Can J Ophthalmol. 2008;43:462–7.
Moorthy RS, Mermoud A, Baerveldt G, et al. Glaucoma associated with uveitis. Surv Ophthalmol. 1997;41:361–94.
Patel HY, Danesh-Meyer HV. Incidence and management of cataract after glaucoma surgery. Curr Opin Ophthalmol. 2013;24:15–20.
Erie JC, Baratz KH, Mahr MA, Johnson DH. Phacoemulsification in patients with Baerveldt tube shunts. J Cataract Refract Surg. 2006;32:1489–91.
Jaffe GJ. Reimplantation of a fluocinolone acetonide sustained drug delivery implant for chronic uveitis. Am J Ophthalmol. 2008;145:667–75.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Disclosures
Daniel Moore, Sandra Stinnett, Glenn Jaffe, and Sanjay Asrani declare that they have no conflict of interest.
Compliance with ethics guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in this study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Moore, D.B., Stinnett, S., Jaffe, G.J. et al. Improved Surgical Success of Combined Glaucoma Tube Shunt and Retisert® Implantation in Uveitic Eyes: A Retrospective Study. Ophthalmol Ther 4, 103–113 (2015). https://doi.org/10.1007/s40123-015-0041-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-015-0041-3