Abstract
Introduction
The aim of this study was to evaluate the effect of short-term oral valproic acid (VPA) on the vision and visual fields of patients with retinitis pigmentosa (RP).
Methods
In this prospective, nonrandomized trial, 10 patients (20 eyes) with established RP were treated with oral VPA 500 mg/day for 3 months. Visual acuity was monitored using the Snellen chart and values were converted into Early Treatment Diabetic Retinopathy Study chart and logarithm of the minimum angle of resolution (logMAR) equivalents. Visual field changes were evaluated using the Humphrey visual field analyzer (30-2 SITA standard test protocol).
Results
Mean visual acuity was significantly improved from a pretreatment value of 20/72 (logMAR 0.560 ± 0.488) to 20/65 (logMAR 0.513 ± 0.422) after 3 months of treatment (P = 0.006). Vision improved by at least one line or more than one line in 10 eyes, and remained stable in the other 10 eyes. Visual field improvement was noted in nine eyes (P < 0.05, χ2 test), nine showing no significant field change and in two visual fields could not be recorded due to poor vision.
Conclusion
Short-term (3-month) treatment with VPA improves the vision and visual field of patients with RP.
Similar content being viewed by others
Introduction
Retinitis pigmentosa (RP) is an unrelentingly progressive disease of the retinal photoreceptors that results in loss of visual field in the early stages and subsequently loss of visual acuity. There are currently no therapeutic agents that slow the progression of this disease, and certainly none that can restore vision in patients with RP.
Contrary to our present understanding of the incurable nature of RP, treatment with valproic acid (VPA) has recently been claimed to be beneficial in maintaining and improving the vision and visual fields of patients with this disease, based on results from a small pilot study [1]. However, the scientific rationale for using VPA to treat RP and the methodology of the study have subsequently been questioned [2, 3]. Here we report the results from a short-term study evaluating oral VPA for the treatment of RP. The authors hypothesize that VPA acts as a chaperon and stabilizes the retinal function thereby preventing further deterioration in visual field and acuity.
Materials and Methods
In this prospective, nonrandomized trial, 10 patients (20 eyes) with established RP received VPA 500 mg/day (Dicorate ER 500, Sun Pharmaceuticals, India; equivalent to 500 mg of divalproex sodium) for the duration of the study, which is still ongoing. The study was approved by the institution’s ethics committee and conducted in accordance with the Declaration of Helsinki and good clinical practice guidelines. Informed consent was obtained from each patient before initiating therapy. The study was conducted at a single center. Baseline investigations before the initiation of treatment included complete blood count, liver function tests, blood urea and serum creatinine estimation, and abdominal ultrasound in female patients to rule out polycystic ovarian disease.
Patients male or female above the age of 16 years were included in the study. Patients with other ocular diseases, or other concomitant retinal diseases that could influence treatment outcome, and patients who had undergone any ocular surgery in the previous 6 months were excluded from study entry. In addition, patients with liver or renal dysfunction, as indicated by laboratory investigations, patients with neurological disease, and pregnant or lactating women were excluded. Female patients were specifically asked to practice birth control methods if they were of reproductive age and were informed of the potential teratogenic effect of VPA.
Best-corrected visual acuity was recorded using the Snellen visual acuity chart at baseline and at 3 months of follow-up. An improvement in visual acuity of at least one line was considered to be an improvement; no change denoted stable vision and loss of one line denoted visual deterioration. Visual acuity was converted into Early Treatment Diabetic Retinopathy Study (ETDRS) chart and logarithm of the minimum angle of resolution (logMAR) equivalents using standard conversion tables [4]. Visual field was recorded using the Humphrey visual field analyzer (HVF) (Humphrey visual analyzer II; Carl Zeiss, Dublin, USA) in patients with at least 20/400 vision. The 30-2 SITA standard test protocol was performed at baseline and at the third month of follow-up.
On the HVF glaucoma change probability analysis (GCPA) print-out, conversion of a location flagged initially with a black square in HVF, indicating a complete scotoma (equivalent to P = 0.05), which converted follow-up to a seeing area was sought and counted (opposite to the glaucoma progression analysis). The following criteria defined the visual field improvement with GCPA as significant (adapted from the Early Manifest Glaucoma Trial) [5–7]: presence of three or more test locations, not necessarily contiguous, that converted from complete scotoma to a completely visible area at last follow-up. Visual field analysis was performed as detailed above, carefully noting the points for improvement. The presence of three or more locations that converted from complete scotoma to a completely visible area on the 30-2 SITA standard test at 3 months was counted. No adverse events were recorded.
Statistical Analysis
Separate statistical analysis is not presented as it is not a comparative study. In the Results section the authors have reported the P value for the visual acuity and fiields assessment separately. The paired t test and χ2 test have also been reported.
Results
Patients either male or female in the age group 16 years and above were included in the study. The duration and the extent of RP were not considered for the inclusion of patients in the study. None of the patients had taken any treatment before this study.
Visual Acuity
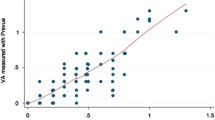
The mean pretreatment visual acuity was 20/72 (logMAR 0.560 ± 0.488) and the mean posttreatment visual acuity at 3 months improved to 20/65 (logMAR 0.513 ± 0.422). The mean change in logMAR across all eyes was a decrease of 0.047. This corresponded to a positive change of five letters or one line in the ETDRS chart at the third month of follow up, which was statistically significant (P = 0.006) compared to baseline.
Vision improved by at least one line or more than one line in 10 eyes. Two eyes showed a one-line improvement, one eye a two-line improvement and four eyes a three-line improvement. In three eyes, vision improved substantially from light perception to 20/200 vision, from count fingers close to face to 20/40 vision and from 20/600 to 20/200 vision (Table 1). Six eyes (three patients) had 20/20 vision pretreatment and this remained stable at 3 months. One patient had 20/200 vision in both eyes and did not show any significant change at the end of the study. A further two eyes from two different patients had a visual acuity of light perception, and this remained unchanged at the end of follow-up. The right eye of patient no. 1 who had only 20/240 vision in her right eye improved to 20/200 at 3 months after starting treatment (Fig. 1a, b).
Visual Fields
Visual field improvement was noted in nine eyes (P < 0.05, χ2 test). Nine eyes showed a significant field change, while in two eyes visual field could not be recorded at baseline or at 3 months due to poor vision (Table 1). Three eyes, left eye of patients 1 (Fig. 2) and 5 (Fig. 3), and right eye of patient 10 (Fig. 4a, b) in which baseline fields could not be assessed due to low vision pretreatment had recordable visual fields at the end of 3 months.
Discussion
Any pharmacological agent with even minimal therapeutic potential for the treatment of RP generates interest because of the lack of confirmed treatment and the inexorable progression to blindness that occurs in patients with the disease. However, newer therapies also invite considerable criticism, and it is essential to gather as much information as possible about them. Therefore, the authors share the results of their short-term study in this report.
Looking into the results of the present study, the role of VPA in stabilizing the visual field and acuity cannot be ignored. The hypothesis of it working as a chaperon and preventing the further loss of functional retina can be well noted.
While the mechanism of action of VPA in RP still remains unclear, the short-term visual gain achieved with the drug in this subset of patients is encouraging. It is unlikely that the considerable improvement in visual and documented retinal sensitivity on visual field examination are solely due to a placebo effect, particularly with the persistent and progressive visual loss as noted in most of the studies [8, 9].
It has been postulated that VPA acts as a pharmacological chaperon to increase the yield of properly folded RP mutant rhodopsins, inhibit levels of histone deacetylase, and inhibit the inflammatory response pathway by the apoptosis of microglial cells [10, 11]. In addition, VPA downregulates complement proteins and increases the level of various neurotrophic factors. Together, these properties of VPA possibly result in the rescue of some of the borderline photoreceptors (damaged or yet to be damaged), thereby improving the visual field.
In a similar pilot study to this, reported by Clemson et al. [1], Goldmann visual field improvement was analyzed in 13 eyes, 9 eyes had improved visual fields, while 2 eyes lost visual field area and 2 eyes had no change in the visual field. The authors reported that a few patients experienced further vision loss during their 3-month follow-up; however, this was not observed in our patient series. Assuming typical loss in the visual field in RP [8, 9, 12], any improvement in the visual field should be considered clinically significant.
While the results presented here are promising, this study has several limitations: only 10 patients were analyzed and the length of follow-up was brief (an average of 3 months). Furthermore, the patients were not genetically characterized nor was their type of RP, due to the potential role they may play in the therapeutic response.
Conclusion
This case series adds to the emerging knowledge on the role of VPA in the treatment of RP, meriting further study in larger groups of patients and for longer treatment periods.
References
Clemson CM, Tzekov R, Krebs M, et al. Therapeutic potential of valproic acid for retinitis pigmentosa. Br J Ophthalmol. 2011;95:89–93.
Van Schooneveld MJ, van den Born LI, van Genderen M, et al. The conclusions of Clemson et al. concerning valproic acid are premature. Br J Ophthalmol. 2011;95:153.
Sandberg MA, Rosner B, Weigel-DiFranco C, et al. Lack of scientific rationale for use of valproic acid for retinitis pigmentosa. Br J Ophthalmol. 2011;95:744.
Holladay JT. Proper method of calculating average visual acuity. J Refract Surg. 1997;13:388–91.
Heijl A, Lindgren G, Olsson J, Asman P. Visual field interpretation with empiric probability maps. Arch Ophthalmol. 1989;107:204–8.
Leske MC, Heijl A, Hyman L, et al. Early Manifest Glaucoma Trial: design and baseline data. Ophthalmology. 1999;106:2144–53.
Heijl A, Leske MC, Bengtsson B, et al. Measuring visual field progression in the Early Manifest Glaucoma Trial. Acta Ophthalmol Scand. 2003;81:286–93.
Merin S, Obolensky A, Farber MD, et al. A pilot study of topical treatment with an alpha2-agonist in patients with retinal dystrophies. J Ocul Pharmacol Ther. 2008;24:80–6.
Berson EL, Rosner B, Weigel-DiFranco C, et al. Disease progression in patients with dominant retinitis pigmentosa and rhodopsin mutations. Invest Ophthalmol Vis Sci. 2002;43:3027–36.
Noorwez SM, Ostrov DA, McDowell JH, et al. A high-throughput screening method for small-molecule pharmacologic chaperones of misfolded rhodopsin. Invest Ophthalmol Vis Sci. 2008;49:3224–30.
Göttlicher M, Minucci S, Zhu P, et al. Valproic acid defines a novel class of HDAC inhibitors inducing differentiation of transformed cells. EMBO J. 2001;20:6969–78.
Massof R, Dagnelie G, Benzschawel T, et al. First order dynamics of visual field loss in retinitis pigmentosa. Clin Vision Sci. 1990;5:1–26.
Acknowledgments
C. K. Minija is the guarantor for this article, and takes responsibility for the integrity of the work as a whole.
Conflict of interest
The authors declare that they have no conflicts of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Shanmugam, P.M., Minija, C.K., Ramanjulu, R. et al. Effect of Short-Term Oral Valproic Acid on Vision and Visual Field in Retinitis Pigmentosa. Ophthalmol Ther 1, 6 (2012). https://doi.org/10.1007/s40123-012-0006-8
Received:
Published:
DOI: https://doi.org/10.1007/s40123-012-0006-8