Abstract
Introduction
Antibiotic stewardship programs (ASP) improve appropriate antibiotic use. Data are limited on the clinical benefit of ASPs in children’s hospitals. This study’s objective was to determine the impact of an ASP on length of stay (LOS) and readmission rate among patients admitted to children’s hospitals.
Methods
Data from a prospective-audit-with-feedback ASP were used to examine the ASP review characteristics, including antibiotic(s) prescribed, clinical indication, recommendations made by the ASP, and agreement with recommendations. Propensity score analysis was utilized to determine the impact of the ASP on LOS and 30-day readmission based on whether the patient received an ASP recommendation and if the clinician agreed with recommendations. Patients were stratified on if they had a complex chronic condition status (CCC) and their service line, medical or surgical.
Results
Of the 8038 reviews included, 1362 (16.9%) resulted in a recommendation that was agreed with in 1116 (81%) cases. Propensity score analysis demonstrated a significantly longer LOS for the non-CCC medicine group who received an ASP recommendation (80.9 vs. 67.6 h, p < 0.001). However, for CCC medicine patients that agreed with the ASP recommendation, a clinically relevant decrease in LOS (158.1 vs. 180.3 h, p = 0.095) was observed. The 30-day readmission rate was significantly greater in CCC medicine patients when comparing those who did not receive a recommendation versus those who did receive a recommendation (7.3% vs 4.2%, respectively; p = 0.005).
Conclusion
Children without a CCC who received an ASP recommendation had a longer length of stay. For children with CCCs, the ASP appeared to decrease LOS and significantly reduce 30-day readmission rates. Overall, this study demonstrate that ASPs offer meaningful clinical benefit justifying resource allocation needed to develop and maintain ASP programs.
Similar content being viewed by others
Introduction
Antibiotic resistant bacteria kill 23,000 Americans and infect another 2 million annually [1]. Compounding this problem is the lack of new antibiotics targeted against the most highly resistant bacteria such as carbapenem-resistant Enterobacteriaceae (CRE). Antibiotic stewardship programs have been implemented in hospitals to improve the use of antibiotics and limit the unnecessary antibiotic pressure that contributes to antibiotic resistance.
Antibiotic stewardship programs (ASP) have been valuable in children’s hospitals. Many pediatric ASPs have significantly reduced the overall use of antibiotics without a reported increase in patient harm or antibiotic resistance [2, 3]. Furthermore, these programs have been associated with an up to US$200,000 reduction in antibiotic acquisition costs [4]. Finally, pediatric clinicians impacted by ASPs believe these programs improve the overall care of patients and provide knowledge about the appropriate use of antibiotics [5].
Nevertheless, data are limited on whether a pediatric ASP results in a clinical benefit for hospitalized children. Among adult hospital ASPs, studies have demonstrated a decrease in the length of stay in the medical ICU, a reduction in Clostridium difficile rates, and an improvement in antibiotic susceptibilities of common pathogens [6–8]. The objective of this study was to determine the impact of a children’s hospital ASP on hospital length of stay (LOS) and rate of readmission.
Methods
Study Design, Setting and Data Sources
A single-center cohort study was performed at a quaternary care freestanding 354-bed children’s hospital. On March 3, 2008 a prospective-audit-with-feedback ASP was implemented, focused on delineating appropriateness of antibiotic use in children who had received a defined group of antibiotics (Supplemental Table 1) for two calendar days [3, 5]. An infectious diseases (ID) pharmacist and ID physician reviewed the clinical data and provided recommendations that were categorized into four areas: (1) stop therapy, (2) modify the antibiotic type, (3) modify the antibiotic dosage and/or duration and (4) obtain an ID consultation [9].
The ASP repository was utilized to capture the data collected on each patient review including: antibiotic(s) prescribed, antibiotic indication, dose of antibiotic(s), clinical indication, length of therapy, and recommendations made by the ASP. After verbal feedback to the provider, agreement or disagreement with recommendations was confirmed and, for those who agreed, compliance and follow through with recommendations was documented. Since a patient could be reviewed by the ASP more than once during an admission, each patient encounter was referred to as a review. Patients’ demographic data as well as the length of hospitalization was obtained from the electronic health record. Data from the ASP repository was merged with the corresponding hospital data in Pediatric Health Information System (PHIS) database in order to obtain additional data elements.
The PHIS database was utilized to identify patients with complex chronic care condition(s) (CCC) ICD9 discharge diagnosis codes [10] and to determine the prevalence of 30-day readmission for the same all-patient refined diagnosis-related groups (APR-DRG). PHIS is an administrative database that contains inpatient, emergency department, ambulatory surgery and observation data from 48 not-for-profit, tertiary care pediatric hospitals in the United States. These hospitals are affiliated with the Children’s Hospital Association (Mission, KS, USA). Data quality and reliability are assured through a joint effort between the Children’s Hospital Association and participating hospitals. The data warehouse function for the PHIS database is managed by Truven Health Analytics (Ann Arbor, MI, USA). For the purposes of external benchmarking, participating hospitals provide discharge/encounter data including demographics, diagnoses, and procedures. Nearly all of these hospitals also submit resource utilization data (e.g., pharmaceuticals, imaging, and laboratory) into PHIS. Data are de-identified at the time of data submission and data are subjected to a number of reliability and validity checks before being included in the database. Using internal patient identifiers, the repository data was merged with the data obtained from PHIS.
Compliance with Ethics Guidelines
This article does not contain any new studies with human or animal subjects performed by any of the authors. This study was approved by Children’s Mercy Hospital’s institutional review board.
Study Population
The study population included all individuals with a single ASP review from March 3, 2008 to March 2, 2014. Data were analyzed related to the APR-DRG medical or surgical category, and the presence of a CCC ICD9 code. Children admitted to the pediatric intensive care unit, neonatal intensive care unit, hematology/oncology unit, those who died, and those with more than one ASP review during their hospitalization were excluded from the analysis.
Outcomes
The primary outcomes were hospital LOS and 30-day hospital readmission rates. Length of stay was calculated as the number of hours between the patients’ admission and discharge from the hospital. A patient was included in the 30-day readmission rate if PHIS assessed data confirmed they were readmitted as an inpatient to the hospital within 30 days of the prior discharge with the same APR-DRG as the prior hospitalization.
Statistical Analysis
First, unadjusted differences in LOS and readmission based on two separate “treatment” indicators were calculated. The first indicator was whether the ASP provider gave a recommendation related to the patient’s antibiotic regimen. The second indicator focused on those receiving a recommendation, related to agreement or disagreement with the recommendations. Both treatment indicators were modeled as binary indicators.
Adjusted differences in the primary outcomes were then calculated using inverse probability-weighted (IPW) estimates as a means to control for possible confounding. The propensity score was calculated using multiple factors that were hypothesized to be related to an ASP recommendation: (1) patient’s age and sex, (2) year since the ASP program was implemented, (3) clinical indication for antibiotic treatment, (4) the prescribed antibiotic(s), (5) patient’s CCC status, and 6) the clinical service line. In an effort to increase statistical efficiency, we utilized stabilized IPWs [11–13]. We hypothesized that LOS and readmission would be significantly related to the patient’s clinical service and the underlying chronic conditions. Consequently, we stratified all analysis by four distinct categories: (1) CCC Surgical, (2) Non-CCC Surgical, (3) Non-CCC Medicine and (4) CCC Medicine.
All analyses were completed with Stata software (v.13.1; StataCorp, College Station, TX, USA). For the unadjusted analysis, the median LOS was calculated and the Wilcoxon Rank-Sum test used to determine statistical significance, while the prevalence of readmission was compared using Fisher’s exact test. A p value <0.05 was used to determine statistical significance. Quintile and logistic regression models were used for calculating IPW estimates. We report the difference in median LOS and difference in proportion readmitted. List-wise deletion was done for instances where agreement status was not documented.
Results
ASP providers performed 17,422 reviews during the study period. Patients admitted to the PICU (n = 1707), the NICU (n = 1893), or the hematology/oncology service (n = 3460), who had more than one review (n = 2038), who had incomplete data for analysis (n = 261) or who died (n = 25) were excluded, resulting in 8038 total reviews for analysis. Among the total 8038 reviews, 1362 (16.9%) resulted in a recommendation which was agreed with in 1116 (81.9%) cases.
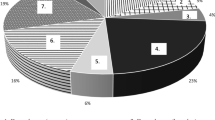
Table 1 shows the demographic/clinical characteristics by the four CCC categories that were included in this study. Patients classified as CCC surgical had the highest percentage of recommendations (28.1%) while non-CCC surgical had the lowest (8.9%). Disagreement with recommendations was highest in patients who were classified as having a CCC (Fig. 1).
Suspected sepsis was the most frequently identified indication for antibiotics among non-CCC medicine children (n = 1060) and ceftriaxone was the most common ASP monitored-antibiotic prescribed in those patients (Supplemental Fig. 1, 2). An ASP-monitored drug plus concurrent metronidazole was most commonly identified among surgical patients. Patients with CCCs most commonly received an ASP-monitored drug plus concurrent clindamycin; additionally, this group of patients often had two or more indications for antibiotics being prescribed. Overall, those with community-acquired pneumonia had the highest percentage of recommendations (35.8%; Supplemental Fig. 2).
Outcomes
The unadjusted median LOS between children receiving a recommendation versus no recommendation was similar in 2 of the 4 groups (Table 2). Non-CCC medicine children who received an ASP recommendation had a significantly longer median LOS than children who did not receive a recommendation (81.5 vs. 66.4 h, p < 0.001). A significantly longer LOS was also observed for the non-CCC surgery group (difference of 5 h, p = 0.015). Differences in length of stay were not statistically significant when evaluating based upon agreement with the ASP recommendations (Table 3). When disagreement with ASP recommendations was documented in the CCC-medicine group, a 28 h longer hospitalization was observed (p = 0.101).
After performing the IPW analysis, the LOS remained significantly longer for the non-CCC medicine group who received a recommendation (Table 2; 80.9 vs. 67.6 h, p < 0.001). Differences in median LOS remained non-significant for all four groups when comparing agreement status. The median LOS was longer for CCC medicine patients when there was disagreement with recommendations versus agreement; however, this was not determined to be statistically significant (180.3 vs. 158.1, p = 0.095).
Differences in the unadjusted 30-day readmission rate were non-significant for all 4 groups (Tables 4, 5). After performing IPW analysis, the readmission rate was significantly greater in children on a medicine service with a CCC that did not receive a recommendation versus those who did receive a recommendation (7.3% vs 4.2%, p = 0.005). The readmission rates for CCC surgery patients without a recommendation was 1.7% higher than those who received a recommendation, though that difference was not statistically significant (p = 0.078). No statistically significant differences in readmission rates were observed based upon agreement status in either the unadjusted or IPW analyses.
Discussion
We present the largest study to date evaluating the impact of an ASP on length of stay and readmission rates in patients hospitalized at a children’s hospital. Length of stay was observed to be longer for non-CCC children admitted to a medical service who received an ASP recommendation, regardless of acceptance. In contrast, a shorter LOS (22 h) was identified in children with CCCs hospitalized on a medicine service when providers agreed with the ASP recommendation. Readmissions were more common for all patients that did not generate an ASP recommendation.
As hospitals continue to develop and implement ASPs, studies evaluating both positive clinical benefits and possible negative outcomes are necessary. In this study, we hypothesized a significant positive clinical benefit would be observed through a decrease in LOS and decrease in 30-day readmission rate. In a previous study, we demonstrated that among patients admitted to a hospitalist service LOS was longer for patients having an ASP recommendation that was agreed upon by the hospitalist service [14]. In this study, which evaluated patients admitted to hospitalist and general pediatric services, the LOS was increased for non-CCC medicine patients receiving an ASP recommendation but was not increased when comparing whether the provider agreed or disagreed with the ASP recommendation. The increase in LOS seen among patients receiving a recommendation by the ASP and not based upon agreement status could be the result of the patients requiring a recommendation having a more serious illness that we were unable to account for in our analysis.
Children with a CCC on a medicine service had almost a 1-day decrease in LOS when a provider agreed with the ASP. Previously, we identified stopping antibiotics as the most common ASP recommendation and demonstrated that disagreements with ASP recommendations most often occurred related to narrowing use of broad-spectrum antibiotics (e.g., linezolid, carbapenems) and among diagnoses such as tracheitis [3, 9]. Similar disagreements in the CCC patients identified in this study may have led to longer durations of these broad-spectrum antimicrobial therapies and longer lengths of stay.
In addition to a reduction in LOS, children with CCCs in whom an ASP recommendation was made experienced a 3% decrease in 30-day readmission rates. Preventable readmissions among children with CCCs provide an excess burden to families and patients and are associated with significant avoidable hospital costs. In previous years, children’s hospitals have seen an increase in admissions among children with CCCs [15]. Data have shown that children with CCCs are often readmitted and the greater number of CCCs a child has increases the risk [16]. Many factors impact the care of these complex children, but our data suggest that input from ASP providers can positively impact the care for these children and may result in significant cost savings. The findings from this study also support that enforcing the judicious use of antimicrobials did not have undesired implications such as an increase in readmission rates.
This study has several limitations. First, we did not include all patients reviewed by our ASP. This could result in underestimating the impact of the ASP as data have shown that intensive care unit lengths of stay have been significantly reduced by the presence of ASPs [6]. Second, this study was done at one institution with an ASP that focuses on the use of prospective-audit with feedback. Other ASPs utilizing different strategies potentially could find similar to greater success in the reduction of LOS and readmission rates. Finally, while we tried to account for severity of illness within our comparison groups by performing IPW analyses, we recognize that there are unmeasured confounders that may have impacted our propensity score calculations and potentially affected the exchangeability of treatment groups.
Conclusion
This study demonstrates the clinical impact that is realized when a formal ASP is implemented in a children’s hospital. For hospitalized children with CCCs whose care resulted in an ASP intervention, shorter hospital stays and less readmissions were confirmed. As health care models for reimbursement continue to change toward a bundled payment model, the presence of a formal ASP in a hospital is essential to ensure optimal care for patients, and especially for those with special healthcare needs. Future research is needed to understand the impact on specific patient populations (e.g., PICU, NICU, hematology-oncology) for which ASPs might have the greatest clinical impact and to add support for the resources necessary for development and implementation of these important hospital programs.
References
Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013/. Accessed Oct 18, 2016.
Di Pentima MC, Chan S, Hossain J. Benefits of a pediatric antimicrobial stewardship program at a children’s hospital. Pediatrics. 2011;128:1062–70.
Newland JG, Stach LM, De Lurgio SA, Hedican E, Yu D, Herigon JC, Prasad PA, Jackson MA, Myers AL, Zaoutis TE. Impact of a prospective-audit-with-feedback antimicrobial stewardship program at a children’s hospital. J Pediatric Infect Dis Soc. 2012;1:179–86.
Metjian TA, Prasad PA, Kogon A, Coffin SE, Zaoutis TE. Evaluation of an antimicrobial stewardship program at a pediatric teaching hospital. Pediatr Infect Dis J. 2008;27:106–11.
Stach LM, Hedican EB, Herigon JC, Jackson MA, Newland JG. Clinicians’ attitudes towards an antimicrobial stewardship program at a children’s hospital. J Pediatric Infect Dis Soc. 2012;1:190–7.
Gentry CA, Greenfield RA, Slater LN, Wack M, Huycke MM. Outcomes of an antimicrobial control program in a teaching hospital. Am J Health Syst Pharm. 2000;57:268–74.
Sarma JB, Marshall B, Cleeve V, Tate D, Oswald T, Woolfrey S. Effects of fluoroquinolone restriction (from 2007 to 2012) on Clostridium difficile infections: interrupted time-series analysis. J Hosp Infect. 2015;91:74–80.
Kaki R, Elligsen M, Walker S, Simor A, Palmay L, Daneman N. Impact of antimicrobial stewardship in critical care: a systematic review. J Antimicrob Chemother. 2011;66:1223–30.
Goldman JL, Lee BR, Hersh AL, Yu D, Stach LM, Myers AL, Jackson MA, Day JC, McCulloh RJ, Newland JG. Clinical diagnoses and antimicrobials predictive of pediatric antimicrobial stewardship recommendations: a program evaluation. Infect Control Hosp Epidemiol. 2015;36:673–80.
Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980–1997. Pediatrics. 2000;106:205–9.
Hernan MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11:561–70.
Hernan MA, Robins JM. Estimating causal effects from epidemiological data. J Epidemiol Community Health. 2006;60:578–86.
Cole SR, Hernan MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168:656–64.
McCulloh RJ, Queen MA, Lee B, Yu D, Stach L, Goldman J, Myers A, Pate B, Newland JG. Clinical impact of an antimicrobial stewardship program on pediatric hospitalist practice, a 5-year retrospective analysis. Hosp Pediatr. 2015;5:520–7.
Berry JG, Hall M, Hall DE, Kuo DZ, Cohen E, Agrawal R, Mandl KD, Clifton H, Neff J. Inpatient growth and resource use in 28 children’s hospitals: a longitudinal, multi-institutional study. JAMA Pediatr. 2013;167:170–7.
Berry JG, Hall DE, Kuo DZ, Cohen E, Agrawal R, Feudtner C, Hall M, Kueser J, Kaplan W, Neff J. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305:682–90.
Acknowledgements
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. Selected results from this study were presented as an oral presentation at ID Week in Philadelphia on October 8, 2014.
Disclosures
Brian R. Lee has had grant funding for antimicrobial stewardship from Pfizer. Jason G. Newland has had grant funding for antimicrobial stewardship from Pfizer. Jennifer L. Goldman, Diana Yu, Angela L. Myers, Leslie M. Stach, Erin Hedican, Mary Anne Jackson declare no conflicts of interests relevant to this article.
Compliance with Ethics Guidelines
This article does not contain any new studies with human or animal subjects performed by any of the authors. This study was approved by Children’s Mercy Hospital’s institutional review board.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to.
Electronic supplementary material
Below is the link to the electronic supplementary material.
40121_2016_139_MOESM1_ESM.jpg
Supplementary material 1 (JPEG 899 kb) Supplemental Fig. 1. The proportion of a specific antibiotic or antibiotic combination receiving a recommendation from the ASP by each of the 4 categories
40121_2016_139_MOESM2_ESM.jpg
Supplementary material 2 (JPEG 913 kb) Supplemental Fig. 2. The proportion of a specific diagnosis receiving a recommendation from the ASP by each of the 4 patient categories
40121_2016_139_MOESM3_ESM.docx
Supplementary material 3 (DOCX 14 kb) Supplemental Table 1: Antimicrobials monitored by our Antimicrobial Stewardship Program
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lee, B.R., Goldman, J.L., Yu, D. et al. Clinical Impact of an Antibiotic Stewardship Program at a Children’s Hospital. Infect Dis Ther 6, 103–113 (2017). https://doi.org/10.1007/s40121-016-0139-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-016-0139-5