Abstract
Cardiovascular diseases are the leading cause of death in the world. Coronary artery diseases, atrial fibrillation or hypertensive heart disease, are among the most important cardiovascular disorders. Hypertension represents a significant risk factor for cardiovascular mortality; thus, control of high blood pressure has become a priority to prevent major complications. Although the choice of drugs for treating hypertension remains controversial, extensive clinical evidences point to calcium channel blockers as first-line agents. Diltiazem, a non-dihydropyridine calcium channel blocker, is an effective and safe antihypertensive drug, alone or in combination with other agents. Diltiazem lowers myocardial oxygen demand through a reduction in heart rate, blood pressure, and cardiac contractility, representing also a good alternative for the treatment of stable chronic angina. Furthermore, diltiazem reduces conduction in atrioventricular node, which is also useful for heart rate control in patients with atrial fibrillation. In this review, clinical experts highlight studies on diltiazem effectiveness and safety for the treatment of several cardiovascular diseases and make evidence-based recommendations regarding the management of diltiazem in the clinical practice.
Funding
Lacer Spain.
Similar content being viewed by others
Introduction
Calcium channel blockers (CCBs) or calcium antagonists reduce the influx of calcium into the cells. Inhibition of calcium channels in the vessels results in vasodilation and, consequently, a lowering of the blood pressure. In the heart, this blockage reduces cardiac contractility and slows atrioventricular conduction velocities [1]. Thus, CCBs are used to treat high blood pressure, alone or in combination with other drugs. All guideline committees consider CCBs an option for first-line treatment of hypertension [2]. In addition, some CCBs are also indicated for the treatment of chronic stable angina or atrial arrhythmias, such as diltiazem [3–5].
Extensive comparative trials have analyzed diltiazem in patients with hypertension, chronic angina, or atrial arrhythmias. The results demonstrated that diltiazem is an effective and safe antihypertensive agent [3]. Diltiazem also reduces the frequency of angina episodes and increases exercise tolerance [4, 5]. The extended-release formulation of diltiazem allows its administration once daily, optimizing antihypertensive and antianginal therapies. Diltiazem belongs to the non-dihydropyridine CCBs. This subclass presents more negative chronotropic and inotropic effects than the dihydropyridine subclass and induces a significant reduction of atrioventricular conduction rate; all of these make non-dihydropyridines useful for acute and chronic treatment as well as for prevention of atrial arrhythmias [6].
The authors of this review, who are clinical experts in cardiovascular diseases: (1) highlight studies on the effectiveness and safety of diltiazem for the treatment of hypertension, stable chronic angina, and atrial arrhythmias; and (2) make evidence-based recommendations regarding the management of diltiazem in the clinical practice, with specific description of the dose most frequently used in each clinical indication. This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Diltiazem in the Treatment of Hypertension
Hypertension or high blood pressure is a chronic condition in which the blood force against the arteries walls is persistently elevated. Untreated hypertension is a major risk factor for a number of cardiovascular disorders. In this regard, calcium antagonists are a first-line treatment for hypertension [2]. Many studies have demonstrated the effectiveness of diltiazem for the treatment of high blood pressure. Diltiazem can be used as monotherapy or in association with other antihypertensive drugs. The usual starting doses are 120–240 mg/day, and it may be increased up to 540 mg/day based on individual patient needs. The dosage range studied in clinical trials was 120–540 mg/day, although current clinical experience with the 540 mg dose is limited [24].
Thus, two independent multicenter studies assessed the safety and efficacy of various once-daily doses of diltiazem in patients with mild-to-moderate hypertension [7]. In one study, patients were randomly treated with once-daily diltiazem (120, 240, 360, or 480 mg) or placebo for 4 weeks, and in the second study, patients were assigned to escalating dosages (180 mg/day for 2 weeks, 360 mg/day for 2 weeks, and then 540 mg/day for 2 weeks). The data demonstrated that once-daily doses higher than 120 mg significantly lower systolic and diastolic blood pressure compared to placebo. Additionally, adverse events were mild and with an incidence similar to placebo.
A later study analyzed the effects of graded-release diltiazem versus ramipril on early morning blood pressure and heart rate in patients with hypertension [8]. The results showed that evening administration of diltiazem (240 mg titrated to 360 mg and to 540 mg) significantly reduced morning blood pressure and heart rate compared to ramipril. Diltiazem also led to a greater reduction in diastolic blood pressure over the 24-h interval after bedtime dosage. However, no difference was found in 24-h systolic blood pressure reduction among the two groups. Therefore, the authors demonstrated diltiazem superiority compared to ramipril and emphasized the importance of managing high blood pressure in the morning, when cardiovascular events occur more frequently.
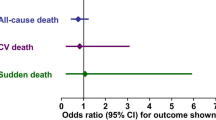
The NORDIL study [3], which enrolled 10,881 patients with diastolic blood pressure of 100 mmHg or more, analyzed the effectiveness of diltiazem in reducing cardiovascular morbidity and mortality. Patients were randomized to receive diltiazem or diuretics, beta-blockers, or both (diuretic/beta-blocker). The combined primary endpoint was fatal and non-fatal stroke, myocardial infarction, and other cardiovascular death. Systolic and diastolic blood pressure was effectively reduced in the diltiazem group and diuretic/beta-blocker groups (reduction: 20.3/18.7 vs. 23.3/18.7 mmHg, respectively; difference in systolic reduction P < 0.001). The incidence of the primary endpoint was similar for the diltiazem group and the diuretic and beta-blocker groups (relative risk: 1.00; 95% confidence interval [CI] 0.87–1.15; P = 0.97). These results indicate that 180–360 mg of diltiazem reduced blood pressure and prevented myocardial infarction to the same extend than diuretics, beta-blockers or both. However, fatal and non-fatal stroke was reduced by 25% in the diltiazem group (relative risk: 0.80; 95% CI 0.65–0.99; P = 0.04). Although the authors argue that this finding may be attributable to chance, they also suggest that it may indicate a novel role of diltiazem in preventing cerebral stroke in hypertensive patients. Similar results were found in the diabetic subgroup.
A meta-analysis of 13 studies with 103,793 patients with hypertension found a decrease in the risk of stroke among the CCB-treated group compared to other antihypertensive drugs (odds ratio 0.90; 95% CI 0.84–0.96; P = 0.002). Whereas dihydropyridine CBBs presented a lower risk of stroke, non-dihydropyridine CCBs did not achieve significance. Thus, the authors concluded that CBBs should be considered in patients with hypertension with increased risk of stroke [9].
Diltiazem in the Treatment of Chronic Stable Angina
A number of studies have analyzed the effects of diltiazem in stable and acute angina. It has been shown that diltiazem increases tolerance to exercise, likely due to its potent dilator effect on coronary arteries, leading to reduction in both heart rate and systemic blood pressure at submaximal and maximal workloads [23].
Although it is known that the risk of adverse cardiovascular and cerebrovascular events is higher during the morning hours, some controversy exists in the literature regarding the greater beneficial effect of diltiazem administration in the evening. In this regard, some authors have shown that once-daily graded-release diltiazem dosed overnight effectively increases exercise tolerance in patients with angina pectoris. In a multicenter, randomized, double blind, placebo-controlled trial, the efficacy and safety of once-daily diltiazem (180, 360 and 420 mg) dosed at 10 pm was compared with placebo, and with diltiazem 360 mg dosed once-daily at 8 am [10]. A total of 311 patients with stable angina pectoris were subjected to a treadmill stress test (standard Bruce protocol) at baseline and at the end of the trial between 6 pm and 8 pm (for evening doses) and between 7 am and 11 am (for morning doses). The results showed that all evening diltiazem doses increased total duration of exercise compared to placebo (P ≤ 0.0201). Diltiazem 360 mg dosed in the evening presented the greatest increase in exercise tolerance, whereas the same dose administered in the morning was not different from placebo. The authors concluded that bedtime diltiazem significantly increases exercise tolerance in patients with angina pectoris over the 24-h dosing interval. The greatest improvement occurred in the morning between 7 am and 11 am, which is the highest cardiovascular risk period. Additionally, diltiazem was safe and well tolerated. However, other authors have found that 480 mg/day of diltiazem administered in the AM or the PM to patients with stable angina was equally effective in suppressing episodes of ambulatory myocardial ischemia [11].
Several studies have evaluated the antianginal effectiveness of diltiazem alone or in combination with beta-blockers or other CCBs. In a double-blind, randomized, placebo-controlled study, patients were treated four-times daily with 90 mg of diltiazem, 60 mg of propranolol, or a combination of 90 mg of diltiazem and 60 mg of propranolol [12]. The results indicated that diltiazem was more effective in improving exercise tolerance (assessed by exercise-stress test and left ventricular ejection fraction) than propranolol or the combination of both [12]. Another study compared the effects of propranolol, propranolol-verapamil, propranolol-nifedipine, and propranolol-diltiazem in patients with chronic angina pectoris [13]. Although the three combinations equally reduced the incidence of angina attacks and decreased ST-segment depression, propranolol-diltiazem presented the lower incidence of adverse clinical effects. Therefore, the authors reported that propranolol-diltiazem should be considered the first-choice combination when beta- and CCB therapy is recommended [13]. Similarly, in a placebo, randomized, double-blind protocol, patients with stable angina pectoris received diltiazem (180–360 mg/day) or nifedipine (30–120 mg/day) for 2 weeks [14]. Patients who remained symptomatic on both drugs during the monotherapy were treated with a combination of diltiazem and nifedipine. Although both drugs alone reduced the frequency of angina and amount of nitroglycerin treatment compared to placebo, diltiazem was significantly more effective in reducing the episodes of ST-segment depression than nifedipine. Additionally, diltiazem alone was better tolerated than nifedipine alone at maximal effective doses. The combination of the two calcium blockers appeared to be beneficial; however, an increase in side effects was detected.
Diltiazem and Atrial Arrhythmias
Calcium channel blockers are used to slow the heart rate and reduce the strength of the cardiac cell contraction in patients with atrial fibrillation or supraventricular tachycardia [15]. This statement is based on studies that analyzed efficacy and safety of diltiazem for heart rate control in patients with permanent atrial fibrillation. One study compared the effect of four daily single-drug regimens (diltiazem 360 mg, verapamil 240 mg, metoprolol 100 mg, and carvedilol 25 mg) on reducing ventricular heart rate and arrhythmia-related symptoms in patients with permanent atrial fibrillation. Whereas diltiazem and verapamil reduced arrhythmia-related symptoms, no effect was observed with the beta-blockers. The results demonstrated that diltiazem 360 mg/day was the most effective treatment for reducing heart rate. [16]. However, other authors have found that 360 mg/day of diltiazem was associated with side effects in 75% of the patients with chronic atrial fibrillation [17], suggesting 240 mg/day diltiazem combined with digoxin as an effective and safe regimen for the treatment of atrial fibrillation. This discrepancy could be due to the low number of patients included in both studies. Additionally, a number of studies have proposed the use of an intravenous bolus followed by a continuous infusion of diltiazem to control the ventricular response during atrial fibrillation [6, 18].
Catheter ablation is the first choice of treatment for supraventricular tachycardia when episodes occur frequently and affect patient’s quality of life [18]. However, long-term preventive pharmacotherapy is an alternative approach for some patients. In this regard, some authors have proposed diltiazem as a potential agent for supraventricular tachycardia prophylaxis, after analyzing the effect of diltiazem 270 mg every 8 h in 36 patients. The results showed that oral diltiazem prevented induction and sustenance of paroxysmal supraventricular tachycardia in most of the patients [19]. In another study, the efficacy and safety of flecaine and the combination of diltiazem and propranolol, were evaluated in the management of supraventricular tachycardia [20]. The data demonstrated that both treatments were successful in 80% of patients, as all the arrhythmic episodes were interrupted out-of-hospital within 2 h. The authors concluded that this therapeutic strategy minimizes emergency assistance during tachycardia recurrences.
A retrospective study evaluated 77 patients with supraventricular tachycardia treated with oral adenosine or intravenous diltiazem in the emergency department [21]. The results demonstrated that 71.9% of the patients returned to normal sinus rhythm after the higher dose of adenosine, whereas the percentage of patients increased to 95% after diltiazem (0.25 mg/kg). Therefore, diltiazem may be a first-choice treatment in patients with narrow-complex supraventricular tachycardia.
Expert Recommendations
According to the 2013 European guidelines for the management of arterial hypertension [22], the primary goal of treatment in these patients is to achieve maximum reduction in the long-term total risk of cardiovascular diseases. The choice of a specific drug or combination among the major antihypertensive drug classes should take into account the patient’s previous history and the presence of other disorders or conditions. Thus, the existence of angina pectoris, hypertension, and supraventricular tachycardia would favor the use of diltiazem versus other agents.
In consonance with a number of studies that have analyzed the effect of diltiazem in specific cardiovascular diseases, and based on their own clinical practice, the authors outline some recommendations regarding the dosing of diltiazem in the clinical practice.
For the treatment of high blood pressure, the experts recommend that diltiazem dosage should be at least 120 mg every 12 h, with 240 and 300 mg/day being the two most prescribed antihypertensive doses (66.6% and 83.3% of the experts, respectively). This recommendation is based on the studies showing a larger effect of these particular doses on the treatment of hypertension; nevertheless, lower doses (60–90 mg every 8 or 12 h) are indicated at initiation of treatment or in patients with mild blood pressure elevation, as well as in patients with lower heart rates where the bradycardic effect of diltiazem may limit its beneficial action in reducing blood pressure.
Additionally, a number of studies have confirmed diltiazem effectiveness in reducing the frequency of angina episodes and increasing exercise tolerance; however, non-dihydropyridine CBBs should not be used when there is a high risk for heart failure due to reduced left ventricular function. For the treatment of angina pectoris, 83.3% of the experts consider 120 mg every 12 h as the most common dose of diltiazem that achieves efficacy in patients with angina, followed by a dose of 300 mg/day (50% of the experts) and 240 mg/day (33% of the experts). The conclusion is based on personal experience and clinical trial results that have showed a better efficacy of those doses in controlling chest pain. As previously stated, the 60- or 90-mg doses administered every 8 or 12 h could also be useful for some patients, particularly in patients with lower heart rate or blood pressure, since both conditions restrict diltiazem titration to higher doses.
In the treatment of atrial arrhythmias, diltiazem is considered an effective rate-control drug. The authors’ recommendation for patients with atrial fibrillation or supraventricular tachycardia is 120 mg every 12 h (66.6% of the experts) as the proper dose for reducing the heart rate. However, in older patients and in those with mild arrhythmias, lower doses of diltiazem (60 or 90 mg every 8 or 12 h) could be useful. In the treatment of atrial fibrillation, the dose may be increased to achieve the target heart rate, usually between 60 and100 bpm, taking into account the drug’s effect on blood pressure, which can limit dose titration. To prevent supraventricular tachycardia, the dose should be between 90 and 120 mg every 12 h, depending on the patient’s clinical response and blood pressure.
References
Abernethy DR, Schwartz JB. Calcium-antagonist drugs. N Engl J Med. 1999;341:1447–57.
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure. National High Blood Pressure Education Program Coordinating Committee. Hypertension. 2003;42:1206–52.
Hansson L, Hedner T, Lund-Johansen P, et al. Randomised trial of effects of calcium antagonists compared with diuretics and beta-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) study. Lancet. 2000;356:359–65.
Claas SA, Glasser SP. Long-acting diltiazem HCl for the chronotherapeutic treatment of hypertension and chronic stable angina pectoris. Expert Opin Pharmacother. 2005;6:765–76.
Ulimoen SR, Enger S, Carlson J, et al. Comparison of four single-drug regimens on ventricular rate and arrhythmia-related symptoms in patients with permanent atrial fibrillation. Am J Cardiol. 2013;111:225–30.
Ellenbogen KA, Dias VC, Cardello FP, et al. Safety and efficacy of intravenous diltiazem in atrial fibrillation or atrial flutter. Am J Cardiol. 1995;75:45–9.
Graney WF. Clinical experience with a once-daily, extended-release formulation of diltiazem in the treatment of hypertension. Am J Med. 1992;93:56S–64S.
White WB, Lacourciere Y, Gana T, Pascual MG, Smith DH, Albert KS. Effects of graded-release diltiazem versus ramipril, dosed at bedtime, on early morning blood pressure, heart rate, and the rate-pressure product. Am Heart J. 2004;148:628–34.
Angeli F, Verdecchia P, Reboldi GP, et al. Calcium channel blockade to prevent stroke in hypertension: a meta-analysis of 13 studies with 103,793 subjects. Am J Hypertens. 2004;17:817–22.
Glasser SP, Gana TJ, Pascual LG, Albert KS. Efficacy and safety of a once-daily graded-release diltiazem formulation dosed at bedtime compared to placebo and to morning dosing in chronic stable angina pectoris. Am Heart J. 2005;149:e1–9.
Deedwania PC, Pool PE, Thadani U, Eff J. Effect of morning versus evening dosing of diltiazem on myocardial ischemia detected by ambulatory electrocardiographic monitoring in chronic stable angina pectoris. Dilacor XR Ambulatory Ischemia Study Group. Am J Cardiol. 1997;80:421–5.
Schroeder JS, Hung J, Lamb IH, Connolly SJ, Jutzy KR, Goris ML. Diltiazem and propranolol, alone and in combination, on exercise performance and left ventricular function in patients with stable effort angina: a double-blind, randomized, and placebo-controlled study. Acta Pharmacol Toxicol (Copenh). 1985;2:55–60.
Johnston DL, Lesoway R, Humen DP, Kostuk WJ. Clinical and hemodynamic evaluation of propranolol in combination with verapamil, nifedipine and diltiazem in exertional angina pectoris: a placebo-controlled, double-blind, randomized, crossover study. Am J Cardiol. 1985;55:680–7.
Frishman W, Charlap S, Kimmel B, et al. Diltiazem, nifedipine, and their combination in patients with stable angina pectoris: effects on angina, exercise tolerance, and the ambulatory electrocardiographic ST segment. Circulation. 1988;77:774–86.
Ulimoen SR, Enger S, Carlson J, et al. Comparison of four single-drug regimens on ventricular rate and arrhythmia-related symptoms in patients with permanent atrial fibrillation. Am J Cardiol. 2013;11:225–30.
Roth A, Harrison E, Milani G, Cohen J, Rahimtoola SH, Elkayam U. Efficacy and safety of medium- and high-dose diltiazem alone and in combination with digoxin for control of heart rate at rest and during exercise in patients with chronic atrial fibrillation. Circulation. 1986;73:316–24.
Hung JS, Yeh SJ, Lin FC, Fu M, Lee YS, Wu D. Usefulness of intravenous diltiazem in predicting subsequent electrophysiologic and clinical responses to oral diltiazem. Am J Cardiol. 1984;54:1259–62.
Medi C, Kalman JM, Freedman SB. Supraventricular tachycardia. Med J Aust. 2009;190:255–60.
Yeh SJ, Kou HC, Lin FC, Hung JS, Wu D. Effects of oral diltiazem in paroxysmal supraventricular tachycardia. Am J Cardiol. 1983;52:271–8.
Alboni P, Tomasi C, Menozzi C, et al. Efficacy and safety of out-of-hospital self-administered single-dose oral drug treatment in the management of infrequent, well-tolerated paroxysmal supraventricular tachycardia. J Am Coll Cardiol. 2001;37:548–53.
Dogan H, Ozucelik DN, Aciksari K, et al. To decide medical therapy according to ECG criteria in patients with supraventricular tachycardia in emergency department: adenosine or diltiazem. Int J Clin Exp Med. 2015;8:9692–9.
Mancia G, Fagard R, Narkiewicz K, et al. 2013 Guidelines for the Management of Arterial Hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Drugs.com. Diltiazem. http://www.drugs.com/pro/diltiazem.html. Accessed Feb 3, 2016.
American Heart Association. http://www.heart.org. Accessed Feb 3, 2016.
Acknowledgments
Sponsorship for this review and the article processing charges was funded by Lacer Spain. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. Writing assistance in the preparation of this manuscript was provided by Patricia Rodriguez, PhD, and editorial assistance was provided by Springer Healthcare. Support for this assistance was funded by Lacer Spain.
Disclosures
Luis Rodríguez Padial has received a payment for writing a monograph on diltiazem in coronary heart disease from Lacer Spain. Gonzalo Baron-Esquivias, Antonio Hernández Madrid, Domingo Marzal Martín, Vicente Pallarés-Carratalá, and Alejandro de la Sierra declare that they have no conflict of interest.
Compliance with ethics guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content To view enhanced content for this article go to www.medengine.com/Redeem/B884F0600FC78158.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rodríguez Padial, L., Barón-Esquivias, G., Hernández Madrid, A. et al. Clinical Experience with Diltiazem in the Treatment of Cardiovascular Diseases. Cardiol Ther 5, 75–82 (2016). https://doi.org/10.1007/s40119-016-0059-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-016-0059-1