Abstract
Purpose
The burden of extended-spectrum beta-lactamase (ESBL)-positive Enterobacteriaceae (ESBL-E) is growing worldwide. We aimed to determine the financial disease burden attributable to ESBL-positive species in cases of bloodstream infection (BSI) due to K. pneumoniae and E. coli.
Methods
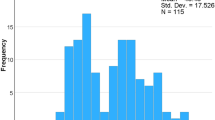
We conducted a cohort study on patients with BSI due to K. pneumoniae or E. coli between 2008 and 2011 in our institution. Data were collected on true hospital costs, length of stay (LOS), basic demographic parameters, underlying diseases as Charlson comorbidity index (CCI) and ESBL positivity of the pathogens. Multivariable regression analysis on hospital costs and length of stay was performed.
Results
Overall we found 1,851 consecutive cases of ESBL-E BSI, 352 (19.0 %) cases of K. pneumoniae BSI and 1,499 (81.0 %) cases of E. coli BSI. Sixty-six of E. coli BSI (18.8 %) and 178 of K. pneumoniae BSI (11.9 %) cases were due to ESBL-positive isolates, respectively (p = 0.001). 830 (44.8 %) cases were hospital-onset, 215 (61.1 %) of the K. pneumoniae and 615 (41.0 %) of the E. coli cases (p < 0.001). In-hospital mortality was overall 19.8, 25.0 % in K. pneumoniae cases and 18.5 % in E. coli cases (p = 0.006). Increased hospital costs and length of stay were significantly associated to BSI with ESBL-positive K. pneumoniae.
Conclusion
In contrast to BSI due to ESBL-positive E. coli, cases of ESBL-positive K. pneumoniae BSI were associated with significantly increased costs and length of stay. Infection prevention measures should differentiate between both pathogens.


Similar content being viewed by others
References
European Centre for Disease Prevention and Control (ECDC). Antimicrobial resistance surveillance in Europe 2013. Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net) Stockholm: ECDC. 2013.
Savard P, Perl TM. A call for action: managing the emergence of multidrug-resistant Enterobacteriaceae in the acute care settings. Curr Opin Infect Dis. 2012;25:371–7.
Goddard S, Muller MP. The efficacy of infection control interventions in reducing the incidence of extended-spectrum beta-lactamase-positive Enterobacteriaceae in the nonoutbreak setting: a systematic review. Am J Infect Control. 2011;39:599–601.
Tacconelli E, Cataldo MA, Dancer SJ, De Angelis G, Falcone M, Frank U, et al. ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug-resistant Gram-negative bacteria in hospitalized patients. Clin Microbiol Infect. 2014;20:1–55.
Tumbarello M, Spanu T, Di Bidino R, Marchetti M, Ruggeri M, Trecarichi EM, et al. Costs of bloodstream infections caused by E. coli and influence of extended-spectrum-beta-lactamase positivity and inadequate initial antibiotic therapy. Antimicrob Agents Chemother. 2010;54:4085–91.
Stewardson A, Fankhauser C, De Angelis G, Rohner P, Safran E, Schrenzel J, et al. Burden of bloodstream infection caused by extended-spectrum beta-lactamase-positive Enterobacteriaceae determined using multistate modeling at a Swiss University Hospital and a nationwide predictive model. Infect Control Hosp Epidemiol. 2013;34:133–43.
Leistner R, Bloch A, Sakellariou C, Gastmeier P, Schwab F. Costs and length of stay associated with extended-spectrum β-lactamase positivity in cases of E. coli bloodstream infection. J Glob Antimicrob Resist. 2014.
Schwaber MJ, Navon-Venezia S, Kaye KS, Ben-Ami R, Schwartz D, Carmeli Y. Clinical and economic impact of bacteremia with extended- spectrum-beta-lactamase-positive Enterobacteriaceae. Antimicrob Agents Chemother. 2006;50:1257–62.
Hilty M, Betsch BY, Bogli-Stuber K, Heiniger N, Stadler M, Kuffer M, et al. Transmission dynamics of extended-spectrum beta-lactamase-positive Enterobacteriaceae in the tertiary care hospital and the household setting. Clin Infect Dis. 2012;55:967–75.
Tschudin-Sutter S, Frei R, Dangel M, Stranden A, Widmer AF. Rate of transmission of extended-spectrum beta-lactamase-positive Enterobacteriaceae without contact isolation. Clin Infect Dis. 2012;55:1505–11.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sorensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:83.
Clinical and Laboratorical Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. Clinical and Laboratorical Standards Institute (CLSI), Wayne, PA, USA [serial on the Internet]. 2012; Twenty-second Informational Supplement M100–S22.
Hu B, Ye H, Xu Y, Ni Y, Hu Y, Yu Y, et al. Clinical and economic outcomes associated with community-acquired intra-abdominal infections caused by extended spectrum beta-lactamase (ESBL) positive bacteria in China. Curr Med Res Opin. 2010;26:1443–9.
Lee SY, Kotapati S, Kuti JL, Nightingale CH, Nicolau DP. Impact of extended-spectrum beta-lactamase-positive E. coli and Klebsiella species on clinical outcomes and hospital costs: a matched cohort study. Infect Control Hosp Epidemiol. 2006;27:1226–32.
de Kraker ME, Wolkewitz M, Davey PG, Koller W, Berger J, Nagler J, et al. Burden of antimicrobial resistance in European hospitals: excess mortality and length of hospital stay associated with bloodstream infections due to E. coli resistant to third-generation cephalosporins. J Antimicrob Chemother. 2011;66:398–407.
Schwaber MJ, Carmeli Y. Mortality and delay in effective therapy associated with extended-spectrum beta-lactamase positivity in Enterobacteriaceae bacteraemia: a systematic review and meta-analysis. J Antimicrob Chemother. 2007;60:913–20.
Biehl LM, Schmidt-Hieber M, Liss B, Cornely OA, Vehreschild MJ. Colonization and infection with extended spectrum beta-lactamase positive Enterobacteriaceae in high-risk patients—review of the literature from a clinical perspective. Crit Rev Microbiol. 2014.
Acknowledgments
We would like to thank Georg Pilarsky, Sebastian Kruse and Oleg Jarychkivski for their excellent work in SQL programming and database management. We also thank Ryan Plocher for his service as language consultant.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Leistner, R., Gürntke, S., Sakellariou, C. et al. Bloodstream infection due to extended-spectrum beta-lactamase (ESBL)-positive K. pneumoniae and E. coli: an analysis of the disease burden in a large cohort. Infection 42, 991–997 (2014). https://doi.org/10.1007/s15010-014-0670-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-014-0670-9