Abstract
Introduction
There was a growing need for practical guidelines for the most common OIs in Germany and Austria under consideration of the local epidemiological conditions.
Materials and methods
The German and Austrian AIDS societies developed these guidelines between March 2010 and November 2011. A structured Medline research was performed for 12 diseases, namely Immune reconstitution inflammatory syndrome, Pneumocystis jiroveci pneumonia, cerebral toxoplasmosis, cytomegalovirus manifestations, candidiasis, herpes simplex virus infections, varizella zoster virus infections, progressive multifocal leucencephalopathy, cryptosporidiosis, cryptococcosis, nontuberculosis mycobacteria infections and tuberculosis. Due to the lack of evidence by randomized controlled trials, part of the guidelines reflects expert opinions. The German version was accepted by the German and Austrian AIDS Societies and was previously published by the Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF; German Association of the Scientific Medical Societies).
Conclusion
The review presented here is a translation of a short version of the German–Austrian Guidelines of opportunistic infections in HIV patients. These guidelines are well-accepted in a clinical setting in both Germany and Austria. They lead to a similar treatment of a heterogeneous group of patients in these countries.
Similar content being viewed by others
Introduction
Although opportunistic infections (OIs) in human immunodeficiency virus (HIV)-infected patients have become rare in industrialized countries [1], patients continue to present with advanced HIV disease and HIV-related OIs. Patients (so-called “late presenters”) are often unaware of their HIV infection or have not received antiretroviral treatment. They present at a late stage and when their overall health status is already poor [2]. Diagnosis and therapy of these OIs remain a challenge.
The aim of the recommendations presented here is to develop general and practical guidelines for the treatment and prophylaxis of the most common OIs in Germany within the framework of local epidemiological conditions. The tables in the different sections of the guidelines represent a summary of the therapeutic guidelines. With regard to diagnosis, the authors refer to the appropriate literature. At the time the guidelines were approved some articles were only available as congress abstracts; if these were published as peer-reviewed article at a later date, the published articles were cited.
The KAAD (Clinical AIDS Working Group Germany) guidelines conform to the international guidelines of the U.S. Centers for Disease Control and Prevention (CDC) (http://www.cdc.gov/mmwr) [3] and guidelines formulated by the AWMF (Association of the Scientific Medical Societies in Germany) in the overlapping fields dermatology and neurology (http://www.uni-duesseldorf.de/AWMF/ll/). Members of other medical societies and the Austrian AIDS Society have also participated and have been consulted (see Appendix).
Some of the following recommendations go beyond the approved use of drugs. In many cases, data from randomized controlled trials (RCTs) are missing, and evidence is based on practical and clinical experiences not presented in published studies (expert opinion). In addition, we advise always checking interactions and toxicities of the applied drugs as these factors cannot be described in detail within the scope of this guideline.
For the treatment of bacterial pneumonia, which is similar in HIV-positive and HIV-negative patients, the appropriate guidelines should be referred to.
Antiretroviral therapy and OI treatment
The indication for antiretroviral therapy (ART) in Germany is based on the guidelines by the German and Austrian AIDS Societies (DAIG and ÖAG, respectively). However, general recommendations regarding when to start ART with mostly ART-naïve patients in the setting of an (acute) OI cannot be given.
In the case of candidiasis, herpes virus infections or, for example, cryptosporidiosis, the immediate start of ART is uncomplicated; in the case of progressive multifocal leukoencephalopathy (PML) it is even necessary and recommended. The situation is more difficult in cases of Pneumocystis jiroveci pneumonia (PcP), cerebral toxoplasmosis, cytomegalovirus (CMV)-retinitis, tuberculosis (TB), atypical mycobacteriosis, and cryptococcosis. We refer to the corresponding sections of these guidelines.
The recommendations given here represent the consensus of the guideline consensus group. The recommendations referring to medical therapies might involve off-label therapies that have not been officially approved. This is due to the lack of data from RCTs on HIV-infected patients with OI. In such cases, the recommendation often refers to data on HIV-negative persons or personal experience (expert opinion). It should also be noted that drug–drug interactions or toxicities need to be excluded in each single case.
Materials and methods
The KAAD was given the task to develop guidelines for the treatment and prophylaxis of OI by the DAIG in March 2010. The members of the DAIG, ÖAG, and other German medical societies (in total 24 societies represented; see Appendix) were asked to participate in the consensus process. The members formed small interest groups (n = 3–10 members) covering the different chapters of these guidelines. A first version was sent out in March 2010 based on the corresponding chapters of the digital version (http://www.hivbook.com). The different groups were free to base their chapters on this proposal after review of the relevant literature or to create new chapters. Via an email system these new chapters were put together until the groups reached a consensus on a final draft. Four weeks before a consensus conference in Cologne on 25 June 2010, these drafts for all 12 chapters were sent out to all members of all groups and to all DAIG members with the request for suggestions for changes. The submitted suggestions for changes which were received were then sent out to the members prior to the meeting. During the consensus conference all suggestions were discussed and voted on separately. Finally, each single chapter and the whole guideline proposal were voted on separately. There was an agreement of 100 % on the whole proposal between all members of the guideline group.
In a third step the Cologne proposal was sent out via email to all members of the DAIG four weeks prior to a DAIG member assembly in Munich (17 March 2011) for comment. Only minor revisions were asked for. The guidelines were again put to vote during the meeting. During the final vote the guidelines received 36 positive unanimous votes and were agreed on in the current version as the DAIG/KAAD OI guidelines.
The German version (long version) of these guidelines was submitted to the AWMF on 30 August 2011 and was published online on 8 November 2011 (http://www.awmf.org/leitlinien/detail/ll/055-006.html). ÖAG approved these guidelines on 9 November 2011.
Results/Guidelines
Immune reconstitution inflammatory syndrome
The immune system is expected to recover following initiation of ART. Some patients, however, show a paradoxical reaction. With widely varying symptoms, this pattern of disease is defined as immune reconstitution disease, immune reconstitution syndrome, or immune reconstitution inflammatory syndrome (IRIS) [4–7]. Different clinical case definitions exist [8, 9], but the preference in the guidelines is for the consensus definition by the International Network for the Study of HIV-associated IRIS (INSHI; http://www.inshi.umn.edu/):
-
1.
Response to ART by:
-
a.
receiving ART and
-
b.
virologic response with >1 log10 copies/ml decrease in HIV RNA.
-
a.
-
2.
Clinical deterioration of an infectious or inflammatory condition temporally related to ART initiation.
-
3.
Symptoms cannot be explained by:
-
a.
expected clinical course of a previously recognized and successfully treated infection,
-
b.
medication side effect or toxicity,
-
c.
treatment failure,
-
d.
complete non-adherence.
-
a.
Manifestations of IRIS are diverse and range from unspecific symptoms, OIs to autoimmune diseases, and malignomas [10].
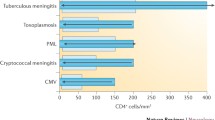
Regarding OIs, the physician must differentiate between symptomatic relapse of a prior infection (paradoxical IRIS) and infections first appearing on ART (unmasking IRIS). Data on the incidence of IRIS vary widely, ranging between 10 and 23 % of all patients at initiation of an ART [10–13]. A prospective study showed an incidence rate in Germany of 24.8 % [14]. An international meta-analysis showed a total incident rate of 16.1 % for IRIS, with the highest rates for IRIS uveitis, followed by TB, cryptococcal meningitis, PML, and rarer cases of Kaposi’s sarcoma or varizella zoster virus (VZV) infections [13]. The greatest risk factor would appear to be a low CD4 T-cell count of <50 cells/μl [12, 15].
Management, treatment, and prophylaxis
Patients starting an ART with a CD4 T-cell count of <200 cells/μl and especially those who have a high viral load require close monitoring. Patients with <50 CD4 T-cells/μl should also be tested for a latent mycobacterial infection (by culture).
A large prospective trial [16] showed no difference for the development of an IRIS when ART was initiated immediately after patients had started an OI therapy (patients with TB were excluded from the trial). In this study, corticosteroids were often given on initiation of ART in a high number of PcP cases, which possibly suppressed some IRIS cases. For TB and cryptococcosis, however, several studies showed an higher incidence of an IRIS when ART was initiated early [17–19].
Corticosteroids are useful in cases of TB-IRIS [20]. Steroid therapy for 2–6 weeks is recommended for cryptococcal-IRIS (increase of intracerebral pressure). The use of non-steroidal anti-inflammatory drugs (NSAIDs) and thalidomide was recommended in some studies, but a general recommendation can not be given for these agents [21].
ART should only be interrupted in very severe cases. Results of the Swiss HIV Cohort Study prove that consequent isoniazid (INH)-prophylaxis in HIV patients with latent TB significantly reduces the risk of a relapse [22].
In general, prognosis for an IRIS is good and the mortality rate is not higher than that for patients without an IRIS [23].
Pneumocystis jiroveci pneumonia
Pneumocystis jiroveci pneumonia is the most frequent OI in Germany and appears predominantly in HIV-infected patients with advanced immunodeficiency (CD4 T cells <200/μl). If there clinical–radiological findings suggest PcP, therapy should be initiated immediately without awaiting results of a bronchoalveolar lavage. A mild PcP [BGA: partial pressure of oxgen (PO2) > 70–80 mmHg] can be treated in outpatient medical care. If ventilation becomes necessary, non-invasive methods (continuous positive airway pressure) are beneficial if applied at an early stage [24]. With respect to the treatment of ART-naïve patients, several experts believe that the initiation of ART can be delayed until acute treatment is completed. However, one RCT has shown advantages of an early start [16].
Treatment
Acute therapy should be given at least for 21 days, if necessary longer. The treatment of choice is a combination of trimethoprim and sulfamethoxazole (TMP/SMX, cotrimoxazole). Oral application of TMP/SMX is only recommended in mild cases, but this therapy can be also considered after initial improvement during intravenous therapy. Positive effects with lower doses of TMP/SMX have been observed in some case reports, but data from controlled trials are missing [25]. All severe cases should be treated intravenously in hospital. In cases of respiratory insufficiency [PO2 < 70 mmHg or alveolar-arterial oxygen tension difference (AaDO2) ≥ 35 mmHg on room air], most experts recommend (5)–10 days of adjuvant administration of prednisolone [approx.1 mg/kg body weight as a single dose or split dose twice daily (bid)]. With prednisolone, mortality risk of severe PcP can be reduced by half and significantly fewer patients require mechanical ventilation [26].
Compared to TMP/SMX, all alternative therapies are less effective. In the event of intolerance or sulfonamide allergy, intravenous pentamidine (4 mg/kg once daily (qd) for 14–21 days is recommended as a second choice; this agent is however more toxic and the dose may therefore have to be reduced after 5 days (2 mg/kg).
Treatment with inhaled pentamidine can be attempted in mild cases of PcP [27, 28]; however, reports on experience with this approach are conflicting [29–31]. Instead of pentamidine, the administration of atovaquone suspension or a combination of trimethoprime and dapsone or clindamycin and primaquine is possible [test for glucose-6-phosphate dehydrogenase (G6PD) deficiency!]. Data are only available for mild to moderate PcP [32–34].
Primaquine is no longer approved for use in Germany, but it is available through international pharmacies. It can only be applied if there are no other alternatives and requires increased efforts in educating patients. According to a meta-analysis, the combination of clindamycin plus primaquine is the most successful therapy if cotrimoxazole therapy fails [35]; this combination appears to be more effective than pentamidine alone [36].
Prophylaxis
Patients with <200 CD4 T-cells/μl (or <14 % of total lymphocytic count) or a previous PcP require prophylaxis. The therapy of choice is TMP/SMX, which also has a protective effect against bacterial infections and cerebral toxoplasmosis [37, 38]. Daily administration is possibly more effective than three doses a week [39]. In cases of moderate cutaneous allergic reactions, desensitization is possible [40]. Monthly pentamidine inhalations are a well-tolerated alternative [41, 42]. A suitable inhalation system should be chosen and an inhalative ß-sympathomimetic should be administered beforehand. Other options are dapsone [41, 42] and atovaquone, both of which have proved to be similarly effective as TMP/SMX, dapsone, and pentamidine in two multi-center trials [43–45]. Atovaquone, however, proved inferior to TMP/SMX in another study [32].
PcP prophylaxis can be discontinued after successful immune reconstitution on ART to ≥200 CD4 T-cells/μl for at least 3 months [46–49]. Only a few cases of reoccurring PcP have been reported for discontinuation at >200 CD4 T-cells/μl [50, 51]. If the HIV RNA is well suppressed, >100 CD4 T-cells/μl may be sufficient to discontinue prophylaxis [52]. However, larger trials would be needed to submit a general recommendation regarding discontinuation for these patients.
The recommendations concerning therapy and prophylaxis of PcP are summarized in Table 1.
Cerebral toxoplasmosis
The incidence of cerebral toxoplasmosis has decreased to less than a quarter of that during the earlier years of the HIV epidemic, [53]. Nevertheless, it remains the most important neurological OI in HIV-infected patients in Europe [54]. Cerebral toxoplasmosis almost always results from a reactivation of a latent infection with Toxoplasma gondii. Extracerebral manifestations are rare.
Treatment
Standard therapy is a combination of pyrimethamine and sulfadiazine, which is effective in 75–89 % of cases [55, 56]. An equivalent alternative is pyrimethamine and clindamycin [55, 57]. TMP/SMX is also possible, with the same doses as used in PcP [58, 59]. TMP/SMX proved to be as effective as sulfadiazine/pyrimethamine in two RCTs on ocular and cerebral toxoplasmosis [60, 61]. A Cochrane review showed no superiority of any one specific regimen [62].
For pyrimethamine, a “loading dose” within the first few days has been used since the first studies [56]. However, the efficacy of this approach has not been proven. Due to the myelotoxicity of pyrimethamine, it is important to add folinic acid (not folic acid) from the start [63].
Other alternatives are atovaquone/pyrimethamine [64] or azithromycin/pyrimethamine [65]; however, data are limited.
Acute therapy lasts for a period of at least 4 (to 6) weeks—longer for alternative therapies. In most cases, empiric treatment of toxoplasmosis is initiated upon identification by radiographic testing. Any improvement or clinical deterioration should be evaluated clinically and by magnetic resonance imaging (MRI) scanning during therapy (after 14 days). In the case of progression, an alternative diagnosis (i.e., cerebral lymphoma, tuberculoma) and a brain biopsy should be considered.
Maintenance therapy with a reduced dosage should be initiated when lesions have resolved at least by 50 %, the clinical course has improved, and contrast enhancement has been reduced or eliminated.
ART should be initiated as soon as possible. In cases of increased intracranial pressure or extensive edema, steroids can be given (dexamethasone, 3–4 × 4–8 mg/day). The choice for steroid therapy must be considered carefully as steroids distort possible differential diagnoses. For example, primary cerebral lymphomas also respond to steroids, and in the case of therapeutic failure, the validity of a potential biopsy can be reduced with steroids.
Antiepileptic therapy is indicated if epileptic attacks occur. Due to rare interactions with ART, gabapentin, pregabalin, and levetiracetam are applied. Levetiracetam is also available as infusion.
Prophylaxis
A distinction must be made between exposure prophylaxis, primary prophylaxis, and secondary prophylaxis after cerebral toxoplasmosis.
-
Exposure prophylaxis: Immunoglobulin G (IgG)-negative patients should avoid eating raw or undercooked meat. An increased risk due to proximity to cats has not been proven [66]. Stricter measures of hygiene should be followed. However, the importance of this recommendation under effective ART is questionable.
-
Primary prophylaxis: IgG-positive patients with <100 CD4 T-cells/μl require primary prophylaxis. The drug regimen of choice is TMP/SMX. In cases of allergy, desensitization may be considered [40]. See above for alternatives. Primary prophylaxis can be discontinued if CD4 T-cell count is >200 cells/μl for at least 3 months.
-
Secondary prophylaxis: In the absence of immune reconstitution, patients require lifelong secondary prophylaxis, usually consisting of half the dose needed for acute therapy [67]. Clindamycin is presumably less suitable as secondary prophylaxis as it cannot cross the intact blood–brain barrier [63]. TMP/SMX also seems less effective for secondary prophylaxis. However, it may be considered because it is simple. A higher dose than that for PcP is definitely required [68, 69]. Prophylaxis may be discontinued safely if initial therapy has led to radiological resolution and if there is an immune reconstitution of >200 CD4 T-cells/μl for at least 3–6 months [31, 70–72].
The recommendations on therapy and prophylaxis of cerebral toxoplasmosis are summarized in Table 2.
Cytomegalovirus manifestations
In Germany, seroprevalence of CMV infection in the adult population is 50–70 %. The risk of a reactivation of CMV infection increases when the CD4 T-cell count is <100 cells/μl. In addition to CMV retinitis, impairment of other end-organs may occur. Due to the limited data on CMV manifestations, the same systemic therapy is recommended in these latter cases as for CMV retinitis [73]. International guidelines are also available for this approach [3].
Treatment
All patients with manifest CMV infection should start ART immediately. The CMV-specific immune response is restored [74], leading to a reduction of CMV viremia [75] and delaying progression of an existing CMV retinitis or its recurrence [76, 77]. In addition to ART, a CMV-specific therapy should be initiated at the time of diagnosis.
Therapy of CMV retinitis can be performed locally or systemically. A local therapy alone does not provide protection against dissemination of infection in the contralateral eye or other organs, but it can be considered if systemic drug toxicity is high. For systemic therapy, four substances are available: gancyclovir, foscarnet, cidofovir, and valgancyclovir (ValGCV). The reader is referred to the product information on these substances for the respective side effects.
Valgancyclovir is the only drug that can be administered orally. It is almost completely hydrolyzed to gancyclovir after resorption in the gastrointestinal tract [78, 79]. Gancyclovir and foscarnet are both recommended as first choices for treating CMV retinitis even though foscarnet proved to be superior in pre-ART times [80, 81]. The side effects of both drugs differ, but the response rates to therapy are similar with both substances [81–83]. As foscarnet must be administered via a central catheter, the administration of gancyclovir is easier and often preferred.
Valgancyclovir has proven to be effective in a comparative study and has the advantage of being less complicated to administer than intravenous infusion. Intravenous treatment, however, may be necessary if foveal infections occur with acute risk of impairing visual acuity. In these cases, gancyclovir and foscarnet are equally recommended for first-line therapy. Treatment with both agents consists of an induction therapy followed by life-long maintenance therapy. Induction therapy usually lasts for at least 2–3 weeks until lesions resolve. Without sufficient ART, selection of resistant CMV mutations is frequent and accumulates as the infection progresses [84, 85].
Several authors recommend ValGCV for first-line therapy based on the results of a prospective randomized trial with ValGCV and parenteral gancyclovir [86] and on those of studies on the pharmacokinetics of ganciclovir, with both showing similar results after the administration of ValGCV [78, 79, 86]. Other studies on the pharmacokinetics of gancyclovir following the administration of valgancyclovir either lack a comparison with parenteral gancyclovir [78], or the administered doses were too low to show bioequivalence of ValGCV and gancyclovir [79]. In summary, a clear recommendation in favor of ValGCV cannot be given at the present time. In the presence of sight-threatening lesions, the panel strongly recommends against treatment with valgancyclovir due to the lack of clear evidence.
Some experts recommend a combination therapy of gancyclovir and foscarnet in full doses for acute sight-threatening lesions. Maintenance therapy with ValGCV can be initiated after lesions have completely resolved [87]; however, this recommendation also lacks data. Without sufficient ART, a relapse is likely to occur, even under maintenance therapy with valgancyclovir.
If lesions (zone II and III) are more anterior, therapy with ValGCV may be attempted with weekly monitoring of the fundus.
Cidofovir has not been tested in controlled trials against gancyclovir or foscarnet. Compared to a delayed therapy, cidofovir significantly slows down the progression of the infection [88]; however, cidofovir is not recommended as first-line therapy due to its side effects. It does remain an important agent in the treatment of progredient CMV retinitis under gancyclovir or foscarnet therapy.
Treatment of recurrences and progression during therapy:
Sufficient ART is crucial for a successful therapy of CMV retinitis. Patients with progredient CMV retinitis on a gancyclovir regimen can be treated successfully with foscarnet or a combination of foscarnet and gancyclovir [89]. A good response is obtained in many cases with treatment with cidofovir, and this drug can therefore be an alternative.
If foscarnet should fail, gancyclovir or a combination of gancyclovir and foscarnet can be effective. Here too, therapy with cidofovir can prevent further progression. Gancyclovir implants can still be effective after therapy failure under systemic gancyclovir or foscarnet due to the significantly higher intraocular gancyclovir concentration produced by the implants [90]. However, there is no protection against further spread of the infection to other organs or to the contralateral eye [91–93].
Extraocular manifestations
Extraocular manifestations are always treated in the same way as a CMV retinitis, although only a few studies support this recommendation. In the presence of a CMV encephalitis or ventriculitis, clinical experience and smaller case studies indicate that a combination therapy with gancyclovir and foscarnet is superior to monotherapy [94–99]. Due to the toxicity of this therapy, the diagnosis should be confirmed.
Prophylaxis
-
Primary prophylaxis: Gancyclovir prophylaxis for CMV retinitis with a CD4 T-cell count of <50 cells/μl is effective, but this is usually too toxic. Fundoscopy every 3 months is recommended but not necessary in the opinion of most experts (especially at a CD4 T-cell count of >100 cells/μl).
-
A dose-reduced secondary prophylaxis should be initiated, preferably with oral ValGCV after about 3 weeks of acute therapy and after lesions have formed scars [87]. Discontinuation of secondary prophylaxis to avoid side effects as soon as possible is recommended and feasible [77, 100, 101]—however, not before at least 6 months of maintenance therapy and immune reconstitution at a CD4 T-cell count of >100–150 cells/μl. A small study showed that discontinuation after 18 months of ART/maintenance therapy is already safe at a CD4 T-cell count of >75/μl [101]. In the first stage after discontinuation, patients undergo an ophthalmology control at least once a month. The required duration of a recurrence prophylaxis is not clear, nor is it as yet known for how long recurrences with other organ manifestations should be monitored. Duration should therefore be handled as for CMV retinitis.
The recommendations on therapy and prophylaxis of CMV manifestations are summarized in Table 3.
Candidiasis
From the roughly 200 Candida species only about 15 different species are encountered in clinical daily practice. The most frequent species by far is C. albicans. Clinical response to fluconazole of infections caused by C. albicans and Candida parapsilosis is mostly good, whereas that to infections caused by C. glabrata or C. krusei is poor or totally missing. Primary in vitro resistance of C. albicans to azoles is rare [102]. Secondary resistance development under long-term azole therapy (fluconazole) was frequently observed in the pre-highly active ART (HAART) era. For the treatment of oral and vulvovaginal candidiasis, the reader is referred to the respective AWMF guidelines [103, 104]. Esophageal candidiasis (thrush) does not require an endoscopy to confirm the diagnosis in the presence of a typical clinical course and a mouth sore.
Treatment
The imidazole antimycotics, such as clotrimazole and the hydroxypyridone ciclopirox olamine, are suitable for local therapy of cutaneous candidiasis. If the immune status of the patient is good and/or in the case of a first episode of an oral candidiasis (OC), topical antimycotics, such as suspensions or pastilles (nystatin, amphotericin B, miconazole), are more inexpensive therapy options, although inferior to a therapy with fluconazole [105–107]. However, adherence is restricted with topically effective suspensions/pastilles. Alternatives are mucoadhesive applications, although these are clearly more expensive. Oral therapy with systemical azole derivatives (fluconazole, itraconazole, posaconazole, voriconazole) show a more rapid response, provide longer protection against recurrences, and are tolerated better by patients [108–111].
Fluconazole can be considered the drug of choice for OC and esophageal candidiasis. A once-daily oral therapy (100 mg for 5–14 days) has been established as the standard for OC [112]. Single doses of up to 750 mg fluconazole have been tested in a small patient group (mostly without ART) and was considered to be equivalent to a 14-day therapy. This therapy, however, should be confined to patients with compliance problems, as data on late relapses are limited [113, 114].
Esophageal candidiasis is usually treated for 10–14 days with doses of 200–400 mg fluconazole qd. Patients presenting with severe dysphagia can initially be treated intravenously and switched to oral application as symptoms improve. If fluconazole resistance has been detected, treatment with other azole derivatives is usually still effective and should be attempted before parenteral therapy is initiated (e.g., with echinocandin). Traconazole, voriconazole, and posaconazole have demonstrated clinical efficacy for cases of fluconazole refractory oropharyngeal and esophageal candidiasis [115–118]. All azole derivatives require a double dose on the first day of the regimen (loading dose).
Therapy with a higher dose of fluconazole (≤800 mg/day ≈ 12 mg/kg/day) or an antimycotic combination therapy [119] can be considered, but data are insufficient. Therapy failure and/or fast relapses occur most frequently in patients with poor immune status (<100 CD4 T-cells/μl).
Data from randomized studies have shown that echinocandins (caspofungin, micafungin or anidulafungin) are as effective and well tolerated as fluconazole for the treatment of candida esophagitis [120–122]. However, application should be restricted to azole refractory infections with clear fluconazole resistance [120, 123, 124].
ART should be initiated immediately if chronic recurring oropharyngeal/esophageal candidiasis is present and at the latest if resistance problems occur. Azole refractory candidiasis as well as azole-resistant strains can disappear with sufficient immune reconstitution as a consequence of ART [125, 126].
Prophylaxis
Regular change of toothbrush and thorough cleaning of dentures are a basic recurrence prophylaxis for OC. OC in HIV-infected children and adults can be treated and relapses prevented by applying disinfecting mouth rinses containing chlorhexidine 0.12 % 1–2× daily for a 90-day period [127, 128]. In the pre-HAART era, secondary prophylaxis or life-long therapy with fluconazole led to significant reductions of chronic recurring oropharyngeal candidiasis—but it has also led to the development of secondary resistance [129, 130].
In a randomized study comparing secondary prophylaxis after OC with intermittent therapy on OC recurrence, relapses and infections of systemic candidiasis were reduced by the long-term prophylaxis. However, no survival benefit has been demonstrated for any candidiasis prophylaxis [131]. Primary prophylaxis is not recommended, and indications for secondary prophylaxis should be restricted to individual case.
The recommendations on therapy and prophylaxis of candidiasis are summarized in Table 4.
Herpes simplex infections
Herpes simplex virus (HSV) infections are frequent in HIV-infected patients. Chronic and atypical courses are possible especially in the setting of severe immune deficiency (<100 CD4 T-cells/μl). Organs such as the esophagus, central nervous system (CNS), eyes, and respiratory tract may also be affected. In these cases and with persistence of lesions for a period of >4 weeks, HSV infection is an AIDS-defining illness.
Treatment
Topical treatment with acyclovir is adequate for patients with a good immune status and only discrete oral lesions. Pencyclovir cream is probably as effective [132]. Genital herpes lesions do not respond as well to topical treatment.
For systemic treatment against HSV-1 and HSV-2, the drug of choice is still acyclovir. Resistance is rare [133], and healing of lesions can be accelerated by the therapy [134]. Severe cases with organ involvement should be treated intravenously. As HSV levels are lower in the CNS than in plasma, the dose to treat encephalitis should be increased. Valacyclovir (ValACV) and famcyclovir are equally effective alternatives to acyclovir [135, 136]. However, they are not approved for patients with immune deficiency and should only be applied if response to acyclovir fails [137].
For uncomplicated genital herpes lesions, shorter regimens of 2 days of 500 mg famcyclovir may be as effective, provided there is no immune deficiency [138].
According to the opinion of some experts, brivudine is an alternative for HSV-1 and VZV, although contraindicated for immunosuppressed patients and only approved for the treatment of VZV. However, results from controlled studies with HIV-infected patients are not available.
In cases of painful mucocutaneous lesions, a local anesthetic can also be applied. Treatment with foscarnet for several weeks may be helpful in exceptional cases, especially if lesions remain refractory to standard treatment [139].
Prophylaxis
Primary prophylaxis is not recommended. An earlier meta-analysis in which acyclovir was found to reduce the risk of both HSV and VZV disease by more than 70 % [140] must be viewed in the context of ART today. Nevertheless, long-term treatment with low-dose acyclovir or ValACV can still be effective treatments for recurrent HSV [141, 142]. The risk of HIV transmission, which is increased threefold by genital HSV-infection [143], is not reduced by treatment with acyclovir [144–146]. Between 70 and 90 % of patients with symptomatic HSV-2 infection and at least 20–50 % of patients with symptomatic HSV-1 infection experience recurring episodes within the first year. Possible causes are local trauma, UV exposure, fever, and immune suppression. A long-term prophylaxis for at least 6 months is recommended for frequent recurrences. This prophylaxis can prevent further episodes in 70–80 % of cases.
The recommendations on therapy and prophylaxis of genital HSV infections are summarized in Table 5.
Varicella zoster infections
Patients infected with HIV are at increased risk for VZV infection. Multisegmental zoster or zoster generalisatus are often observed with low CD4 T-cell counts. Chronic courses with ulcerating forms and involvement of other organs are rare. Pneumonia or CNS involvement should be considered.
Treatment
A monosegmental zoster can be treated with oral acyclovir. Famcyclovir and ValACV are alternatives. Each complicated, multisegmental or facial zoster should be treated intravenously for 10–14 days. After clinical improvement is evident, a switch to oral therapy is possible.
Zoster neuralgia occurs less frequently in HIV-negative patients treated with the alternative drugs ValACV, famcyclovir, and brivudine than when treated with acyclovir [147]. However, according to a Cochrane analysis, the results of this study are not clear [148]. Brivudine is not licensed for the treatment of immunocompromised patients. Acyclovir resistance is rare and most frequently observed under long-term therapy [149, 150]; in these cases, foscarnet (3 × 40 mg/kg) or cidofovir (5 mg/kg, maximum 375 mg 1×/week) can be given.
Early concomitant and monitored pain management with NSAIDs and/or other opiates in combination with amitriptyline and/or pregabalin is important. For further information on zoster pain, the reader is referred to the AWMF guidelines.
Prophylaxis
Varicella vaccination seems to be fairly safe and effective for patients with a CD4 T-cell count of >400/μl [149]. Vaccination should be considered if VZV serology is negative. In individuals with negative serology and exposure to VZV, administration of hyperimmunoglobulin may be attempted. Long-term primary prophylaxis is usually not effective; however, a long-term low-dose therapy can be considered in the presence of persistent recurring episodes.
The recommendations on therapy and prophylaxis of VZV-infections are summarized in Table 6.
Progressive multifocal leukoencephalopathy
Progressive multifocal leukoencephalopathy (PML) is a severe demyelinating disease of the CNS caused by the John Cunningham virus (JCV). Prognosis for PML was poor in the pre-HAART era, with the median interval between the onset of the first symptoms and death being 3–6 months. With effective ART, there are significantly fewer cases of disease progression, and even complete remission seems possible [151]. Nevertheless, mortality of patients with PML remains high at 50 %, albeit ART [152].
Treatment
There is no specific PML treatment with proven efficacy; consequently, the mainstay of therapy is immune reconstitution. As such, priority remains on the initiation and optimization of an ART. Treating physicians are recommended to apply intracerebral penetrating agents. A successful immune reconstitution accounts for a significant reduction in mortality [151–156].
After initiation of ART, a paradoxical worsening of clinical symptoms in terms of an immune reconstitution inflammatory syndrome (IRIS) has been observed in approximately 16–23 % of PML cases. Administration of corticosteroids for PML-IRIS has only been described in case studies [157], and evidence of a benefit was not provided. Given the slight difference in the 1-year survival rate for PML patients and PML-IRIS patients [158], the use of corticosteroids or a temporary discontinuation of ART must be weighed up against the risks of a possible decline of the JCV-specific immune response.
Several supportive immunomodulatory approaches have been tested, but to date there is no convincing evidence for the efficacy of treatments with immunoglobulin, interleukin-2 (IL-2), or IL-α [159]. Therapeutic regimens aimed at inhibiting JCV replication have also been attempted, but as yet relevant evidence supporting the clinical use of drugs such as cytosine arabinoside is not available [153, 160].
Antiviral treatment with acyclovir, cidofovir, ganciclovir, brivudin, ribavirin, foscarnet and the combination therapy foscarnet and zidovudine have also proven to be ineffective [161].
Recently, 5-HT2a inhibitors and/or serotonin receptor antagonists have been discussed for PML treatment. In vitro data for the suppression of JCV replicates via 5HT(2A)R inhibitors are contradictory [162–167]. Results from controlled clinical studies are missing. Based on promising in vitro data [168] a phase I/II study of mefloquine was initiated—only be stopped due to a lack of efficacy. In summary, specific treatments for PML cannot be recommended outside clinical trials.
Prophylaxis
There is no prophylaxis. Exposure prophylaxis is also not possible.
The recommendations for therapy and prophylaxis of PML are summarized in Table 7.
Cryptosporidiosis
Cryptosporidiosis is a parasitic intestinal disease with fecal–oral transmission, mainly caused Cryptosporidium parvum (two other frequent types: C. hominis and C. meleagridis). While diarrhea almost always resolves within a few days in healthy hosts or in HIV-infected patients with CD4 T-cell counts of >200 cells/μl, it is often chronic in HIV patients with a CD4 T-cell count of <100 cells/μl [169]. Infection of the biliary tract leading to sclerosing cholangitis is frequent, particularly among patients with severe immunodeficiency, but may be reversible with immune reconstitution [170–172] (level of evidence C). Other rare manifestations are infections of the pancreatic duct and pulmonary infections [173, 174].
Treatment
Successful immune reconstitution under ART can lead to complete resolution of clinical crytosporidiosis [175, 176].
Symptomatic treatment with loperamide and/or tincture of opium should be given. Octreotide (off label) can also be applied. Sufficient hydration is important and infusions may even be required. No specific treatment has been validated [177]. Rifaximin is promising, as first studies with AIDS patients show [178]; however, results from randomized studies are still missing.
Nitazoxanide was found to be effective in a small randomized study in immunocompetent patients [179]. However, this drug is not approved for AIDS patients and showed no effects in a double-blind randomized study in HIV-infected children with cryptosporidiosis [180].
Paromomycin has been found to have favorable effects on diarrhea [181]. However, a double-blind randomized study showed no benefit compared to placebo [182]. In a Cochrane review for the prevention and treatment of cryptosporidiosis, paromomycin did not reduce diarrheal frequency permanently [177].
Prophylaxis
There is no generally accepted prophylaxis, although a protective effect of rifabutin and clarithromycin has been reported from retrospective studies. Azithromycin showed no effect [183]. The usual hygienic measures (gloves) are usually adequate. Patients do not need to be isolated. However, accommodation with other immunosuppressed patients should be avoided.
The recommendations on therapy and prophylaxis of cryptosporidiosis are summarized in Table 8.
For further information, refer to guidelines by the CDC for cryptosporidiosis in HIV-infected patients (CDC 2009; http://www.cdc.gov/mmwr) [3].
Cryptococcal infections
Cryptococcosis occurs much more frequently in Africa, the USA, and Southeast Asia than in Europe. Bird droppings (especially of pigeons) are presumably a key reservoir, but a direct transmission between humans has not been observed. Although transmission occurs via inhalation, pulmonary symptoms or lung infiltration are only seen in 30–40 % of cases of HIV-infected patients. Cryptococcosis infection is often followed by disseminated disease in HIV patients with severe immunodeficiency (<100 CD4 T-cells/μl) and often involves the CNS (>75 %, meningitis) [21].
Treatment
Recommended treatment for a cryptococcal meningitis is the combination regimen of amphotericin B deoxycholate (AmB-D; 0.7–1.0 mg/kg/day i.v.) and flucytosine (100 mg/kg/day i.v. or p.o. if available), divided into four doses a day. Acute therapy should be given for at least 14 days. If clinical response is good, a switch to monotherapy with fluconazole (400 mg/day) for another 8 weeks is possible [21]. Liposomal amphotericin is slightly more effective than conventional AmB-D and provides an alternative, if AmB-D is not well tolerated [184]. Monotherapy with fluconazole as initial treatment in HIV-infected patients is not sufficient, even with higher daily doses of 800–2,000 mg. Thus, it is only considered as an option in countries with limited resources [21, 185].
In the pre-HAART era, a triple combination therapy with AmB-D, flucytosine, and fluconazole was favored for the treatment of cryptococcal meningitis in Germany [186]. However, in one randomized study, the triple combination was not more effective than a combination with AmB-D and flucytosine or AmB-D and fluconazole or a monotherapy with AmB-D [187].
The combination with AmB-D and fluconazole is an alternative in regions with limited resources where flucytosine is not available. In a small study in Thailand, a higher dose of fluconazole (800 mg/day) combined with AmB-D (0.7 mg/kg/day) was more effective than monotherapy with AmB-D alone or a regimen of AmB-D + fluconazole (400 mg/day). Other combination therapies (e.g. fluconazole + flucytosine) are possible alternatives, but lack sufficient data [188].
Itraconazole plays no role in primary therapy and is less effective than fluconazole in maintenance therapy [189].
Monotherapy with posaconazole showed a response rate of up to 50 % in a small case study on refractory diseases and therefore provides an alternative for this indication [190]. Efficacy of voriconazole in salvage therapy is still not clear [191]. Echinocandines show no in vitro effect against C. neoformans.
In the case of an IRIS when ART is initiated during antimycotic treatment, additional treatment with corticosteroids (0.5–1.0 mg/kg/day prednisolone equivalent) is required [21].
In refractory treatment situations, additional administration of γ-interferon might be useful in individual cases [192].
Treatment success is monitored based on the clinical course and repeated lumbal punctures. Patients should have their intracranial pressure measured at time of diagnosis. If the intracranial pressure is very high, several punctures should be made in the first week until it is reduced to ≤20 cm. In individual cases, cerebrospinal fluid (CSF) drainage can be considered to reduce the intracranial pressure if there are no contraindications [21].
For mild, isolated cryptococcal pneumonia (negative CSF diagnosis), monotherapy with fluconazole (400 mg/day) is possible. Treatment should continue for 6–12 months. Severe cases of pneumonia with or without acute respiratory distress syndrome (ARDS) should be treated the same way as meningitis (see above).
ART-naïve patients at the time of diagnosis should start an ART after a 2wo-week induction therapy with antimycotics. However, an optimal time for initiation of ART is not yet clearly defined.
Prophylaxis
Primary prophylaxis can not be recommended to HIV-infected patients in Germany due to lack of a clear survival benefit [193].
After acute therapy of cryptococcal meningitis, secondary prophylaxis should be introduced. Fluconazole (200 mg/day) is the regimen of choice and is also more effective than itraconazole [21]. Secondary prophylaxis can be discontinued after at least 6 months maintenance therapy with sufficient immune reconstitution (>100 CD4 T-cells/μl and HIV-RNA below detection limit for over 6 months). The risk of a relapse is high if maintenance therapy is discontinued too early [194].
The recommendations on therapy and prophylaxis of cryptococcosis are summarized in Table 9.
Infections of nontuberculous mycobacteria
Human immunodeficiency virus-associated infections of nontuberculous mycobacteria (NTM) have declined in countries where ART is available [195–197]. In addition to disseminated NTM diseases, which develop almost exclusively in the setting of severe CD4 T-cell depletion (<50 CD4 T-cells/μl) and which are mainly (>90 %) caused by the Mycobacterium avium complex or M. intracellulare (Mycobacterium avium intracellure complex, MAI), incidences of NTM-IRIS as well as pulmonary NTM diseases are also observed. Pulmonary NTM is frequently caused by other species, such as M. kansasii, M. xenopi, M. malmoense, and M. abscessus. For further information on diagnosis, the reader is referred to the American Thoracic Society criteria [198].
Due to the ubiquitous occurrence of NTM, pre-exposure prophylaxis is not possible and an isolation of infected patients is not necessary. Some specialists, however, recommend a screening of generalized MAI infections in patients with CD4 T-cell counts of <50/μl prior to initiation of an ART.
Treatment
Given here are only recommendations for the MAI therapy. With respect to NTM species other than MAI, the reader is referred to the appropriate literature [198] or advised to consult experts (NTM-NET). A combination treatment of macrolide (clarithromycin or azithromycin) and ethambutol plus/minus rifabutin is recommended [198]. Rifabutin is preferred to rifampicin due to its in vitro efficacy against MAI and its lower interaction potential. Following the publication of data showing that rifabutin could be omitted from the treatment regimen [199], another randomized study demonstrated a survival benefit with the triple combination clarithromycin, rifabutin, and ethambutol compared to clarithromycin with either ethambutol or rifabutin—the mortality rate was halved in the treatment arm receiving this triple (clarithromycin-containing) combination [200].
The doses for rifabutin must occasionally be adjusted to the ART regimen [201]. Clarithromycin increases the rifabutin serum level, while rifabutin decreases the clarithromycin level. Treatment duration with rifabutin has not yet been determined in studies; however, experts recommend discontinuing rifabutin after a few weeks and with clinical improvement.
The daily doses for clarithromycin should not exceed 2 × 500 mg, as a higher mortality risk has been described for patients receiving higher dosages [202, 203]. Azithromycin can be administered instead of clarithromycin, as these two drug are comparably effective in combination with ethambutol, with slightly more rapid sterilization of blood cultures with clarithromycin [196, 199, 204]. As macrolides are the cornerstone of therapy, the development of resitance to macrolides must be avoided, and monotherapy with macrolides should not be administered. In the case of intolerance, alternative substances, such as fluoroquinolone, amikacin, cycloserine, dapsone, linezolid, or mefloquine, are available. However, clinical evidence for the treatment of MAI infections with these alternative substances is still insufficient.
In the case of NTM-IRIS, the extent and duration of an antimycobacterial therapy are not clear. It is possible that partial virus suppression is enough for a NTM-specific immune reconstitution [205].
It is easier to evaluate the clinical response to localized NTM infections. In cases of localized lymphadenitis and skin manifestations, therapy duration of 6 months is recommended after patients are culture-negative. If the clinical response is good and CD4 T-cells continue to increase under a still effective ART, the regimen can be reduced after 3 months to a recurrence prophylaxis with a macrolide for a further 3 months. Patients with abdominal localization have a poorer response and require a more aggressive and longer therapy [206, 207]. Additive corticoid therapy has symptomatic indications.
The treatment of patients with pulmonal NTM diseases not deriving from an IRIS are based on the guidelines for non-HIV-infected patients [198].
Prophylaxis
In the USA, placebo controlled trials for clarithromycin, azithromycin and rifabutin showed that primary prophylaxis significantly reduced MAI-morbidity and -mortality in severely immunocompromised patients [208–211]. All these studies, however, were undertaken in the pre-HAART era. In addition, MAI-infections are less frequent in Europe, so that only a few patients receive primary prophylaxis [212]. Due to the declining incidences since the introduction of ART, primary prophylaxis can only avoid a small number of diseases [197]. NTM-associated IRIS can also not be prevented by prophylactic drugs [206].
Therefore primary prophylaxis is not recommended in Germany. After treatment of a disseminated MAI-infection, patients lacking other ART options, should receive secondary prophylaxis with a macrolide, provided CD4 T-cell count is under 50 cells/μl. Weekly doses of azithromycin are convenient and efficacy is comparable to daily rifabutin [208].
Secondary prophylaxis or maintenance therapy can be discontinued under an ART and if patients are without symptoms and CD4 T-cell count is >100/μl for 6 months.
The recommendations concerning therapy and prophylaxis of disseminated MAI-diseases are summarized in Table 10.
Tuberculosis
Globally, TB is the most prevalent HIV-associated opportunistic infection. In Germany, TB is rare. HIV-infected patients are affected by TB independent of their CD4 T-cell count [213], although incidences increase with advanced immunodeficiency [214].
Treatment
Uncomplicated cases of TB can successfully be treated with a standard therapy regimen over a period of 6 months, regardless of HIV status.
First-line drugs are rifampicin, INH, ethambutol, pyrazinamide, and streptomycin, with INH and rifampicin being the most effective. TB should always be treated with a combination of four drugs in the initial phase to prevent drug resistance. Standard initial phase therapy is a 2-month course of rifampicin, INH, ethambutol, and pyrazinamide, followed by a continuation phase therapy of 4 months rifampicin and INH.
In individual cases, such as incompliance, it may be necessary to extend the standard treatment duration to ≥9 months, especially if sputum cultures are still positive after 2 months. Recurrences after successful therapy appear more frequently in HIV-infected patients [215]. If standard therapy has not been initially applied, treatment should always last for at least 9 months.
Alternatively, ethambutol, streptomycin, and reserve drugs such as ofloxacin or moxifloxazin, cycloserine, and linezolid may be administered. Since this treatment is no different from that for multiresistant TB, these patients should be treated in specialized centers.
Adverse events
Adverse effects occur frequently with anti-TB therapy (refer to individual drug information for side effects, necessary testing, and drug interactions). Severe side effects are observed more often in HIV-infected patients than in HIV-negative patients [216].
ART and TB therapy
Antiretroviral therapy significantly reduces the morbidity and mortality rate in HIV-infected patients [217]. A 6-month TB standard therapy achieves similar success in both HIV-infected and HIV-negative patients [218].
Although a large retrospective and a large open-label, randomized trial showed a survival benefit with simultaneous ART and anti-TB treatment, this approach proves to be difficult in practice due to overlapping drug interactions and side effects [219]. For TB meningitis, side effects are more frequent during the first 2 months of therapy if ART and anti-TB therapy are initiated simultaneously. In this case, a delay of ART by 2 months is possible without risking a higher mortality [220].
With regard to other forms of TB, 25–60 % of patients develop an IRIS in the first 3 months of ART treatment [221]. A consensus on a uniform case definition of TB-IRIS was reached in 2008 [9], which we refer to in the chapter on IRIS of this guideline.
Adherence to simultaneous HIV and Mycobacterium TB treatment is difficult to achieve due to the high pill burden and overlapping toxicities. Both rifampicin and protease inhibitors (PIs) are metabolized by cytochrome P450 3A. Concomitant therapy is therefore not recommended [222, 223] (Table 11). Rifabutin can be combined with boosted PIs, however the dose must be adjusted (Table 12). It may be useful to determine serum levels [201]; however, this approach has not been tested in clinical research with clear endpoints.
Recommendations can be given for first-line ART therapy with tenofovir (TDF), TDF + emtricitabine (FTC), and FTC plus efavirenz in combination with rifampicin-based TB therapy. Alternatives are other efavirenz-based regimens (without adjustment of dose) with rifabutin [222].
To date, clinical data on combinations of rifamycin with new drugs, such as darunavir, raltegravir, or maraviroc, are limited. Due to the strong inducing potential of cytochrome P450 3A, PIs should be avoided and maraviroc should only be given under close observation. Rifampicin also induces the enzyme UGT1A1, leading to increased glucoronidation and reduced plasma levels of raltegravir [224]. No interactions have been reported with tenofovir and T-20 [225].
The recommendations on the adjustment for combination of ART/rifampicin in TB therapy are summarized in Table 12.
Treatment of active TB has clinical priority over ART. In patients with <100 CD4 T-cells/μl, simultaneous treatment of both infections is indicated [222, 226]. However, even in this situation it is recommended to start TB therapy first for 2 weeks before initiating ART to prevent possible side effects.
For patients with 100–350 CD4 T-cells/μl, ART can be delayed for 2 months until the anti-TB drugs can be reduced for the continuation phase. There is no evidence for an optimal timing of ART when the CD4 T-cell count is >350 cells/μl [222]. The results of a large randomized trial indicate that mortality rate in patients with 200–500 CD4 T-cells/μl is reduced when ART is initiated during TB therapy [219].
For HIV patients with <50 CD4 T-cells/μl, the results of a recent study show a benefit of a delayed ART. The decision should be made carefully under consideration of the situation of each single patient [17, 227].
HIV-infected patients already on a successful ART should remain on ART, although the regimen may need to be modified [226].
The recommendations for co-administering ART with rifabutin are summarized in the statement that adherence is the most important factor for therapeutic success and to avoid resistant TB strains. The World Health Organization (WHO) recommends a directly observed therapy for these patients.
Treatment of latent TB infection with M. tuberculosis
Latent tuberculosis infection (LTBI) is defined by a positive Mycobacterium TB-specific immune response in the tuberculin skin test (TST) or an interferon gamma release assay (IGRA) in the absence of active TB. Clear values for a positive Mycobacterium TB-specific immune response in HIV-infected patients do not exist. Patients are not infectious as the TB is not active.
However, HIV-infected patients with LTBI carry a higher risk of developing active TB. According to guidelines for the treatment of LTBI by the CDC [228], HIV-infected patients with a TST of >5 mm should be given treatment with INH for 9 months. This probably also applies to patients with positive IGRA test results, but convincing data are still missing [229]. Alternatively, a 4-month course of rifampicin can be given.
A 2-month course of rifampicin and pyrazinamide is no longer recommended, as it has been associated with significantly higher toxicities in HIV-negative patients [230, 231].
Multidrug resistant and extensively drug-resistant TB
In 2006, 2.2 % of all TB patients showed multidrug resistance (at least resistance against INH and rifampicin). Among these, 5 % were HIV-infected [232]. In addition to incidences of multidrug resistance (MDR), incidences of extensive drug resistance (XDR) were reported in at least 58 countries in 2010 [233]. XDR TB is defined by the WHO as TB which is additionally resistant to fluoroquinolones and at least one of the injectable drugs amikacin, capreomycin, or kanamycin.
Due to the complex therapy and an overall poor prognosis, patients with MDR/XDRTB should be treated in specialized centers.
References
Brooks JT, Kaplan JE, Holmes KK, Benson C, Pau A, Masur H. HIV-associated opportunistic infections—going, going, but not gone: the continued need for prevention and treatment guidelines. Clin Infect Dis. 2009;48:609–11. doi:10.1086/596756.
Mussini C, Manzardo C, Johnson M, Monforte A, Uberti-Foppa C, Antinori A, et al. Patients presenting with AIDS in the HAART era: a collaborative cohort analysis. AIDS. 2008;22:2461–9. doi:10.1097/QAD.0b013e328314b5f1.
Kaplan JE, Benson C, Holmes KH, Brooks JT, Pau A, Masur H. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009;58(RR-4):1–207; quiz CE1-4..
Jacobson MA, Zegans M, Pavan PR, O’Donnell JJ, Sattler F, Rao N, et al. Cytomegalovirus retinitis after initiation of highly active antiretroviral therapy. Lancet. 1997;349:1443–5. doi:10.1016/S0140-6736(96)11431-8.
Race EM, Adelson-Mitty J, Kriegel GR, Barlam TF, Reimann KA, Letvin NL, et al. Focal mycobacterial lymphadenitis following initiation of protease-inhibitor therapy in patients with advanced HIV-1 disease. Lancet. 1998;351:252–5. doi:10.1016/S0140-6736(97)04352-3.
Shelburne SA, Montes M, Hamill RJ. Immune reconstitution inflammatory syndrome: more answers, more questions. J Antimicrob Chemother. 2006;57:167–70. doi:10.1093/jac/dki444.
French MA. HIV/AIDS: immune reconstitution inflammatory syndrome: a reappraisal. Clin Infect Dis. 2009;48:101–7. doi:10.1086/595006.
Robertson J, Meier M, Wall J, Ying J, Fichtenbaum CJ. Immune reconstitution syndrome in HIV: validating a case definition and identifying clinical predictors in persons initiating antiretroviral therapy. Clin Infect Dis. 2006;42:1639–46. doi:10.1086/503903.
Meintjes G, Lawn SD, Scano F, Maartens G, French MA, Worodria W, et al. Tuberculosis-associated immune reconstitution inflammatory syndrome: case definitions for use in resource-limited settings. Lancet Infect Dis. 2008;8:516–23. doi:10.1016/S1473-3099(08)70184-1.
Haddow LJ, Easterbrook PJ, Mosam A, Khanyile NG, Parboosing R, Moodley P, et al. Defining immune reconstitution inflammatory syndrome: evaluation of expert opinion versus 2 case definitions in a South African cohort. Clin Infect Dis. 2009;49:1424–32. doi:10.1086/630208.
Ratnam I, Chiu C, Kandala NB, Easterbrook PJ. Incidence and risk factors for immune reconstitution inflammatory syndrome in an ethnically diverse HIV type 1-infected cohort. Clin Infect Dis. 2006;42:418–27. doi:10.1086/499356.
Murdoch DM, Venter WD, Feldman C, Van Rie A. Incidence and risk factors for the immune reconstitution inflammatory syndrome in HIV patients in South Africa: a prospective study. AIDS. 2008;22:601–10. doi:10.1097/QAD.0b013e3282f4a607.
Muller M, Wandel S, Colebunders R, Attia S, Furrer H, Egger M. Immune reconstitution inflammatory syndrome in patients starting antiretroviral therapy for HIV infection: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:251–61. doi:10.1016/S1473-3099(10)70026-8.
Wahlers K. Immunereconstitution inflammatory syndrome in a prospective German cohort. Abstract 149. KIT. 2010.
Lawn SD, Myer L, Bekker LG, Wood R. Tuberculosis-associated immune reconstitution disease: incidence, risk factors and impact in an antiretroviral treatment service in South Africa. AIDS. 2007;21:335–41. doi:10.1097/QAD.0b013e328011efac.
Zolopa A, Andersen J, Powderly W, Sanchez A, Sanne I, Suckow C, et al. Early antiretroviral therapy reduces AIDS progression/death in individuals with acute opportunistic infections: a multicenter randomized strategy trial. PLoS ONE. 2009;4:e5575. doi:10.1371/journal.pone.0005575.
Abdool Karim SS, Naidoo K, Grobler A, Padayatchi N, Baxter C, Gray AL et al. Integration of antiretroviral therapy with tuberculosis treatment. N Engl J Med. 2011;365(16):1492–1501. doi:10.1056/NEJMoa1014181.
Makadzange AT, Ndhlovu CE, Takarinda K, Reid M, Kurangwa M, Gona P, et al. Early versus delayed initiation of antiretroviral therapy for concurrent HIV infection and cryptococcal meningitis in sub-saharan Africa. Clin Infect Dis. 2010;50:1532–8. doi:10.1086/652652.
Sungkanuparph S, Filler SG, Chetchotisakd P, Pappas PG, Nolen TL, Manosuthi W, et al. Cryptococcal immune reconstitution inflammatory syndrome after antiretroviral therapy in AIDS patients with Cryptococcal meningitis: a prospective multicenter study. Clin Infect Dis. 2009;49:931–4. doi:10.1086/605497.
Meintjes G, Wilkinson RJ, Morroni C, Pepper DJ, Rebe K, Rangaka MX, et al. Randomized placebo-controlled trial of prednisone for paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome. AIDS. 2010;24:2381–90. doi:10.1097/QAD.0b013e32833dfc68.
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50:291–322. doi:10.1086/649858.
Elzi L, Schlegel M, Weber R, Hirschel B, Cavassini M, Schmid P, et al. Reducing tuberculosis incidence by tuberculin skin testing, preventive treatment, and antiretroviral therapy in an area of low tuberculosis transmission. Clin Infect Dis. 2007;44:94–102. doi:10.1086/510080.
Park WB, Choe PG, Jo JH, Kim SH, Bang JH, Kim HB, et al. Immune reconstitution inflammatory syndrome in the first year after HAART: influence on long-term clinical outcome. AIDS. 2006;20:2390–2. doi:10.1097/QAD.0b013e328010f201.
Confalonieri M, Calderini E, Terraciano S, Chidini G, Celeste E, Puccio G, et al. Noninvasive ventilation for treating acute respiratory failure in AIDS patients with Pneumocystis carinii pneumonia. Intensive Care Med. 2002;28:1233–8. doi:10.1007/s00134-002-1395-2.
Thomas M, Rupali P, Woodhouse A, Ellis-Pegler R. Good outcome with trimethoprim 10 mg/kg/day-sulfamethoxazole 50 mg/kg/day for Pneumocystis jirovecii pneumonia in HIV infected patients. Scand J Infect Dis. 2009;17:1–7.
Briel M, Bucher HC, Boscacci R, Furrer H. Adjunctive corticosteroids for Pneumocystis jiroveci pneumonia in patients with HIV-infection. Cochrane Database Syst Rev. 2006;19(3):CD006150.
Arasteh K, Heise W, L’Age M. Treatment of mild to moderately severe Pneumocystis carinii pneumonia with cotrimoxazole versus pentamidine aerosol. Preliminary results of a prospective randomized therapy study. Med Klin (Munich). 1990;85:260–3.
Montgomery AB, Feigal DW Jr, Sattler F, Mason GR, Catanzaro A, Edison R, et al. Pentamidine aerosol versus trimethoprim-sulfamethoxazole for Pneumocystis carinii in acquired immune deficiency syndrome. Am J Respir Crit Care Med. 1995;151:1068–74.
Conte JE Jr, Chernoff D, Feigal DW Jr, Joseph P, McDonald C, Golden JA. Intravenous or inhaled pentamidine for treating Pneumocystis carinii pneumonia in AIDS. A randomized trial. Ann Intern Med. 1990;113:203–9.
Soo Hoo GW, Mohsenifar Z, Meyer RD. Inhaled or intravenous pentamidine therapy for Pneumocystis carinii pneumonia in AIDS. A randomized trial. Ann Intern Med. 1990;113:195–202.
Benson CA, Kaplan JE, Masur H, Pau A, Holmes KK. Treating opportunistic infections among HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America. MMWR Recomm Rep. 2004;53:1–112.
Hughes W, Leoung G, Kramer F, Bozzette SA, Safrin S, Frame P, et al. Comparison of atovaquone (566C80) with trimethoprim-sulfamethoxazole to treat Pneumocystis carinii pneumonia in patients with AIDS. N Engl J Med. 1993;328:1521–7. doi:10.1056/NEJM199305273282103.
Dohn MN, Weinberg WG, Torres RA, Follansbee SE, Caldwell PT, Scott JD, et al. Oral atovaquone compared with intravenous pentamidine for Pneumocystis carinii pneumonia in patients with AIDS. Atovaquone Study Group. Ann Intern Med. 1994;121:174–80.
Toma E, Thorne A, Singer J, Raboud J, Lemieux C, Trottier S, et al. Clindamycin with primaquine vs. Trimethoprim-sulfamethoxazole therapy for mild and moderately severe Pneumocystis carinii pneumonia in patients with AIDS: a multicenter, double-blind, randomized trial (CTN 004). CTN-PCP Study Group. Clin Infect Dis. 1998;27:524–30.
Benfield T, Atzori C, Miller RF, Helweg-Larsen J. Second-line salvage treatment of AIDS-associated Pneumocystis jirovecii pneumonia: a case series and systematic review. J Acquir Immune Defic Syndr. 2008;48:63–7. doi:10.1097/QAI.0b013e31816de84d.
Helweg-Larsen J, Benfield T, Atzori C, Miller RF. Clinical efficacy of first- and second-line treatments for HIV-associated Pneumocystis jirovecii pneumonia: a tri-centre cohort study. J Antimicrob Chemother. 2009;64:1282–90. doi:10.1093/jac/dkp372.
Ioannidis JP, Cappelleri JC, Skolnik PR, Lau J, Sacks HS. A meta-analysis of the relative efficacy and toxicity of Pneumocystis carinii prophylactic regimens. Arch Intern Med. 1996;156:177–88.
DiRienzo AG, van Der Horst C, Finkelstein DM, Frame P, Bozzette SA, Tashima KT. Efficacy of trimethoprim-sulfamethoxazole for the prevention of bacterial infections in a randomized prophylaxis trial of patients with advanced HIV infection. AIDS Res Hum Retroviruses. 2002;18:89–94. doi:10.1089/08892220252779629.
El-Sadr WM, Luskin-Hawk R, Yurik TM, Walker J, Abrams D, et al. A randomized trial of daily and thrice-weekly trimethoprim-sulfamethoxazole for the prevention of PCP in HIV-infected persons. Clin Infect Dis. 1999;29:775–83.
Leoung GS, Stanford JF, Giordano MF, Stein A, Torres RA, Giffen CA, et al. Trimethoprim-sulfamethoxazole (TMP-SMZ) dose escalation versus direct rechallenge for Pneumocystis carinii pneumonia prophylaxis in human immunodeficiency virus-infected patients with previous adverse reaction to TMP-SMZ. J Infect Dis. 2001;184:992–7. doi:10.1086/323353.
Bucher HC, Griffith L, Guyatt GH, Opravil M. Meta-analysis of prophylactic treatments against Pneumocystis carinii pneumonia and toxoplasma encephalitis in HIV-infected patients. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;15:104–14.
Bozzette SA, Finkelstein DM, Spector SA, Frame P, Powderly WG, He W, et al. A randomized trial of three antipneumocystis agents in patients with advanced human immunodeficiency virus infection. NIAID AIDS Clinical Trials Group. N Engl J Med. 1995;332:693–9. doi:10.1056/NEJM199503163321101.
El-Sadr WM, Murphy RL, Yurik TM, Luskin-Hawk R, Cheung TW, Balfour HH Jr, et al. Atovaquone compared with dapsone for the prevention of Pneumocystis carinii pneumonia in patients with HIV infection who cannot tolerate trimethoprim, sulfonamides, or both. Community Program for Clinical Research on AIDS and the AIDS Clinical Trials Group. N Engl J Med. 1998;339:1889–95. doi:10.1056/NEJM199812243392604.
Chan C, Montaner J, Lefebvre EA, Morey G, Dohn M, McIvor RA, et al. Atovaquone suspension compared with aerosolized pentamidine for prevention of Pneumocystis carinii pneumonia in human immunodeficiency virus-infected subjects intolerant of trimethoprim or sulfonamides. J Infect Dis. 1999;180:369–76. doi:10.1086/314893.
Rosenberg DM, McCarthy W, Slavinsky J, Chan CK, Montaner J, Braun J, et al. Atovaquone suspension for treatment of Pneumocystis carinii pneumonia in HIV-infected patients. AIDS. 2001;15:211–4.
Schneider MM, Borleffs JC, Stolk RP, Jaspers CA, Hoepelman AI. Discontinuation of prophylaxis for Pneumocystis carinii pneumonia in HIV-1-infected patients treated with highly active antiretroviral therapy. Lancet. 1999;353:201–3. doi:10.1016/S0140-6736(98)07204-3.
Weverling GJ, Mocroft A, Ledergerber B, Kirk O, Gonzales-Lahoz J, d’Arminio Monforte A et al. Discontinuation of Pneumocystis carinii pneumonia prophylaxis after start of highly active antiretroviral therapy in HIV-1 infection. EuroSIDA Study Group. Lancet. 1999;353:1293–8.
Lopez Bernaldo de Quiros JC, Miro JM, Pena JM, Podzamczer D, Alberdi JC, Martinez E et al. A randomized trial of the discontinuation of primary and secondary prophylaxis against Pneumocystis carinii pneumonia after highly active antiretroviral therapy in patients with HIV infection. Grupo de Estudio del SIDA 04/98. N Engl J Med. 2001;344:159–67. doi:10.1056/NEJM200101183440301.
Abgrall S, Matheron S, Le Moing V, Dupont C, Costagliola D. Pneumocystis carinii pneumonia recurrence in HIV patients on highly active antiretroviral therapy: secondary prophylaxis. J Acquir Immune Defic Syndr. 2001;26:151–8.
Degen O, ven Lunzen J, Horstkotte MA, Sobottka I, Stellbrink HJ. Pneumocystis carinii pneumonia after the discontinuation of secondary prophylaxis. AIDS. 2002;16(10):1433–4.
Mussini C, Pezzotti P, Antinori A, Borghi V, Monforte A, Govoni A, et al. Discontinuation of secondary prophylaxis for Pneumocystis carinii pneumonia in human immunodeficiency virus-infected patients: a randomized trial by the CIOP Study Group. Clin Infect Dis. 2003;36:645–51. doi:10.1086/367659.
D’Egidio GE, Kravcik S, Cooper CL, Cameron DW, Fergusson DA, Angel JB. Pneumocystis jiroveci pneumonia prophylaxis is not required with a CD4 + T-cell count <200 cells/microl when viral replication is suppressed. AIDS. 2007;21:1711–5. doi:10.1097/QAD.0b013e32826fb6fc.
Abgrall S, Rabaud C, Costagliola D. Incidence and risk factors for toxoplasmic encephalitis in human immunodeficiency virus-infected patients before and during the highly active antiretroviral therapy era. Clin Infect Dis. 2001;33:1747–55. doi:10.1086/322622.
Antinori A, Larussa D, Cingolani A, Lorenzini P, Bossolasco S, Finazzi MG, et al. Prevalence, associated factors, and prognostic determinants of AIDS-related toxoplasmic encephalitis in the era of advanced highly active antiretroviral therapy. Clin Infect Dis. 2004;39:1681–91. doi:10.1086/424877.
Dannemann B, McCutchan JA, Israelski D, Antoniskis D, Leport C, Luft B, et al. Treatment of toxoplasmic encephalitis in patients with AIDS. A randomized trial comparing pyrimethamine plus clindamycin to pyrimethamine plus sulfadiazine. The California Collaborative Treatment Group. Ann Intern Med. 1992;116:33–43.
Leport C, Raffi F, Matheron S, Katlama C, Regnier B, Saimot AG, et al. Treatment of central nervous system toxoplasmosis with pyrimethamine/sulfadiazine combination in 35 patients with the acquired immunodeficiency syndrome. Efficacy of long-term continuous therapy. Am J Med. 1988;84(1):94–100.
Katlama C, De Wit S, O’Doherty E, Van Glabeke M, Clumeck N. Pyrimethamine-clindamycin vs. pyrimethamine-sulfadiazine as acute and long-term therapy for toxoplasmic encephalitis in patients with AIDS. Clin Infect Dis. 1996;22:268–75.
Canessa A, Del Bono V, De Leo P, Piersantelli N, Terragna A. Cotrimoxazole therapy of Toxoplasma gondii encephalitis in AIDS patients. Eur J Clin Microbiol Infect Dis. 1992;11:125–30.
Beraud G, Pierre-Francois S, Foltzer A, Abel S, Liautaud B, Smadja D, et al. Cotrimoxazole for treatment of cerebral toxoplasmosis: an observational cohort study during 1994–2006. Am J Trop Med Hyg. 2009;80:583–7.
Torre D, Casari S, Speranza F, Donisi A, Gregis G, Poggio A, et al. Randomized trial of trimethoprim-sulfamethoxazole versus pyrimethamine-sulfadiazine for therapy of toxoplasmic encephalitis in patients with AIDS. Italian Collaborative Study Group. Antimicrob Agents Chemother. 1998;42:1346–9.
Soheilian M, Sadoughi MM, Ghajarnia M, Dehghan MH, Yazdani S, Behboudi H, et al. Prospective randomized trial of trimethoprim/sulfamethoxazole versus pyrimethamine and sulfadiazine in the treatment of ocular toxoplasmosis. Ophthalmology. 2005;112:1876–82. doi:10.1016/j.ophtha.2005.05.025.
Dedicoat M, Livesley N. Management of toxoplasmic encephalitis in HIV-infected adults (with an emphasis on resource-poor settings). Cochrane Database Syst Rev. 2006;3:CD005420. doi:10.1002/14651858.CD005420.pub2.
Luft BJ, Chua A. Central nervous system toxoplasmosis in HIV pathogenesis, diagnosis, and therapy. Curr Infect Dis Rep. 2000;2:358–62.
Chirgwin K, Hafner R, Leport C, Remington J, Andersen J, Bosler EM, et al. Randomized phase II trial of atovaquone with pyrimethamine or sulfadiazine for treatment of toxoplasmic encephalitis in patients with acquired immunodeficiency syndrome: ACTG 237/ANRS 039 Study. AIDS Clinical Trials Group 237/Agence Nationale de Recherche sur le SIDA, Essai 039. Clin Infect Dis. 2002;34:1243–50. doi:10.1086/339551.
Bosch-Driessen LH, Verbraak FD, Suttorp-Schulten MS, van Ruyven RL, Klok AM, Hoyng CB, et al. A prospective, randomized trial of pyrimethamine and azithromycin vs pyrimethamine and sulfadiazine for the treatment of ocular toxoplasmosis. Am J Ophthalmol. 2002;134:34–40.
Wallace MR, Rossetti RJ, Olson PE. Cats and toxoplasmosis risk in HIV-infected adults. JAMA. 1993;269:76–7.
Podzamczer D, Miro JM, Ferrer E, Gatell JM, Ramon JM, Ribera E, et al. Thrice-weekly sulfadiazine-pyrimethamine for maintenance therapy of toxoplasmic encephalitis in HIV-infected patients. Spanish Toxoplasmosis Study Group. Eur J Clin Microbiol Infect Dis. 2000;19:89–95.
Ribera E, Fernandez-Sola A, Juste C, Rovira A, Romero FJ, Armadans-Gil L, et al. Comparison of high and low doses of trimethoprim-sulfamethoxazole for primary prevention of toxoplasmic encephalitis in human immunodeficiency virus-infected patients. Clin Infect Dis. 1999;29:1461–6. doi:10.1086/313515.
Duval X, Pajot O, Le Moing V, Longuet P, Ecobichon JL, Mentre F, et al. Maintenance therapy with cotrimoxazole for toxoplasmic encephalitis in the era of highly active antiretroviral therapy. AIDS. 2004;18:1342–4.
Miro JM, Lopez JC, Podzamczer D, Pena JM, Alberdi JC, Martinez E, et al. Discontinuation of primary and secondary Toxoplasma gondii prophylaxis is safe in HIV-infected patients after immunological restoration with highly active antiretroviral therapy: results of an open, randomized, multicenter clinical trial. Clin Infect Dis. 2006;43:79–89. doi:10.1086/504872.
Fournier S, Rabian C, Alberti C, Carmagnat MV, Garin JF, Charron D, et al. Immune recovery under highly active antiretroviral therapy is associated with restoration of lymphocyte proliferation and interferon-gamma production in the presence of Toxoplasma gondii antigens. J Infect Dis. 2001;183:1586–91. doi:10.1086/320706.
Furco A, Carmagnat M, Chevret S, Garin YJ, Pavie J, De Castro N, et al. Restoration of Toxoplasma gondii-specific immune responses in patients with AIDS starting HAART. AIDS. 2008;22:2087–96. doi:10.1097/QAD.0b013e3283136d68.
Whitley RJ, Jacobson MA, Friedberg DN, Holland GN, Jabs DA, Dieterich DT, et al. Guidelines for the treatment of cytomegalovirus diseases in patients with AIDS in the era of potent antiretroviral therapy: recommendations of an international panel. International AIDS Society-USA. Arch Intern Med. 1998;158:957–69.
Komanduri KV, Viswanathan MN, Wieder ED, Schmidt DK, Bredt BM, Jacobson MA, et al. Restoration of cytomegalovirus-specific CD4 + T-lymphocyte responses after ganciclovir and highly active antiretroviral therapy in individuals infected with HIV-1. Nat Med. 1998;4:953–6.
Deayton J, Mocroft A, Wilson P, Emery VC, Johnson MA, Griffiths PD. Loss of cytomegalovirus (CMV) viraemia following highly active antiretroviral therapy in the absence of specific anti-CMV therapy. AIDS. 1999;13:1203–6.
Labetoulle M, Goujard C, Frau E, Rogier H, Niessen F, Furlan V, et al. Cytomegalovirus retinitis in advanced HIV-infected patients treated with protease inhibitors: incidence and outcome over 2 years. J Acquir Immune Defic Syndr. 1999;22:228–34.
Tural C, Romeu J, Sirera G, Andreu D, Conejero M, Ruiz S, et al. Long-lasting remission of cytomegalovirus retinitis without maintenance therapy in human immunodeficiency virus-infected patients. J Infect Dis. 1998;177:1080–3.
Brown F, Banken L, Saywell K, Arum I. Pharmacokinetics of valganciclovir and ganciclovir following multiple oral dosages of valganciclovir in HIV- and CMV-seropositive volunteers. Clin Pharmacokinet. 1999;37:167–76.
Jung D, Dorr A. Single-dose pharmacokinetics of valganciclovir in HIV- and CMV-seropositive subjects. J Clin Pharmacol. 1999;39:800–4.
Polis MA, deSmet MD, Baird BF, Mellow S, Falloon J, Davey RT Jr, et al. Increased survival of a cohort of patients with acquired immunodeficiency syndrome and cytomegalovirus retinitis who received sodium phosphonoformate (foscarnet). Am J Med. 1993;94:175–80.
Group AR. Foscarnet-Ganciclovir Cytomegalovirus Retinitis Trial. 4. Visual outcomes. Studies of Ocular Complications of AIDS Research Group in collaboration with the AIDS Clinical Trials Group. Ophthalmology. 1994;101:1250–61.
[No authors listed]. Foscarnet-Ganciclovir Cytomegalovirus Retinitis Trial. 4. Visual outcomes. Studies of ocular complications of AIDS Research Group in collaboration with the AIDS Clinical Trials Group. Ophthalmology. 1994;101(7):1250–61
Moyle G, Harman C, Mitchell S, Mathalone B, Gazzard BG. Foscarnet and Ganciclovir in the treatment of CMV retinitis in AIDS patients: a randomised comparison. J Infect. 1992;25:21–7.
Jabs DA, Enger C, Dunn JP, Forman M. Cytomegalovirus retinitis and viral resistance: ganciclovir resistance. CMV Retinitis and Viral Resistance Study Group. J Infect Dis. 1998;177:770–3.
Jabs DA, Enger C, Forman M, Dunn JP. Incidence of foscarnet resistance and cidofovir resistance in patients treated for cytomegalovirus retinitis. The Cytomegalovirus Retinitis and Viral Resistance Study Group. Antimicrob Agents Chemother. 1998;42:2240–4.
Martin DF, Sierra-Madero J, Walmsley S, Wolitz RA, Macey K, Georgiou P, et al. A controlled trial of valganciclovir as induction therapy for cytomegalovirus retinitis. N Engl J Med. 2002;346:1119–26.
Lalezari J, Lindley J, Walmsley S, Kuppermann B, Fisher M, Friedberg D, et al. A safety study of oral valganciclovir maintenance treatment of cytomegalovirus retinitis. J Acquir Immune Defic Syndr. 2002;30:392–400.
Lalezari JP, Stagg RJ, Kuppermann BD, Holland GN, Kramer F, Ives DV, et al. Intravenous cidofovir for peripheral cytomegalovirus retinitis in patients with AIDS. A randomized, controlled trial. Ann Intern Med. 1997;126:257–63.
Group AR. Combination foscarnet and ganciclovir therapy vs monotherapy for the treatment of relapsed cytomegalovirus retinitis in patients with AIDS. The Cytomegalovirus Retreatment Trial. The Studies of Ocular Complications of AIDS Research Group in Collaboration with the AIDS Clinical Trials Group. Arch Ophthalmol. 1996;114:23–33.
Hatton MP, Duker JS, Reichel E, Morley MG, Puliafito CA. Treatment of relapsed cytomegalovirus retinitis with the sustained-release ganciclovir implant. Retina. 1998;18:50–5.
Fuchs AV, Wolf E, Scheider A, Jager H, Kampik A. Cytomegalovirus (CMV) retinitis in AIDS. Gancilovir implantation in comparison with systemic therapy. Ophthalmologe. 1999;96:11–5.
Smith CL. Local therapy for cytomegalovirus retinitis. Ann Pharmacother. 1998;32:248–55.
Muccioli C, Belfort R Jr. Treatment of cytomegalovirus retinitis with an intraocular sustained-release ganciclovir implant. Braz J Med Biol Res. 2000;33:779–89.
Berman SM, Kim RC. The development of cytomegalovirus encephalitis in AIDS patients receiving ganciclovir. Am J Med. 1994;96:415–9.
Kalayjian RC, Cohen ML, Bonomo RA, Flanigan TP. Cytomegalovirus ventriculoencephalitis in AIDS. A syndrome with distinct clinical and pathologic features. Medicine (Baltimore). 1993;72(2):67–77.
Ewig S, Bierhoff E, Luster W, Steudel A, Niese D. Progressive cytomegalovirus encephalitis in successful ganciclovir therapy of cytomegalovirus retinitis in an AIDS patient. Klin Wochenschr. 1991;69:449–53.
Schwarz TF, Loeschke K, Hanus I, Jager G, Feiden W, Stefani FH. CMV encephalitis during ganciclovir therapy of CMV retinitis. Infection. 1990;18:289–90.
Mastroianni CM, Ciardi M, Folgori F, Sebastiani G, Vullo V, Delia S, et al. Cytomegalovirus encephalitis in two patients with AIDS receiving ganciclovir for cytomegalovirus retinitis. J Infect. 1994;29:331–7.
Cinque P, Baldanti F, Vago L, Terreni MR, Lillo F, Furione M, et al. Ganciclovir therapy for cytomegalovirus (CMV) infection of the central nervous system in AIDS patients: monitoring by CMV DNA detection in cerebrospinal fluid. J Infect Dis. 1995;171:1603–6.
Macdonald JC, Torriani FJ, Morse LS, Karavellas MP, Reed JB, Freeman WR. Lack of reactivation of cytomegalovirus (CMV) retinitis after stopping CMV maintenance therapy in AIDS patients with sustained elevations in CD4 T cells in response to highly active antiretroviral therapy. J Infect Dis. 1998;177:1182–7.
Jouan M, Saves M, Tubiana R, Carcelain G, Cassoux N, Aubron-Olivier C, et al. Discontinuation of maintenance therapy for cytomegalovirus retinitis in HIV-infected patients receiving highly active antiretroviral therapy. AIDS. 2001;15:23–31.
Sanglard D, Odds FC. Resistance of Candida species to antifungal agents: molecular mechanisms and clinical consequences. Lancet Infect Dis. 2002;2:73–85.
Reinel D, Plettenberg A, Seebacher C, Abeck D, Brasch J, Effendy I, et al. Oral candidiasis. J Dtsch Dermatol Ges. 2004;2:874–6.
Mendling W, Seebacher C. Guideline vulvovaginal candidosis: guideline of the German Dermatological Society, the German Speaking Mycological Society and the Working Group for Infections and Infectimmunology of the German Society for Gynecology and Obstetrics. Mycoses. 2003;46:365–9.
Flynn PM, Cunningham CK, Kerkering T, San Jorge AR, Peters VB, Pitel PA, et al. Oropharyngeal candidiasis in immunocompromised children: a randomized, multicenter study of orally administered fluconazole suspension versus nystatin. The Multicenter Fluconazole Study Group. J Pediatr. 1995;127(2):322–8.
Hood S, Evans J, Bond J, Wilkins E, Denning D. The treatment of oropharyngeal candidiasis in HIV-infected patients with oral amphotericin B suspension. AIDS Patient Care STDS. 1998;12(8):625–7.
Pons V, Greenspan D, Lozada-Nur F, McPhail L, Gallant JE, Tunkel A. Oropharyngeal candidiasis in patients with AIDS: randomized comparison of fluconazole versus nystatin oral suspensions. Clin Infect Dis. 1997;24(6):1204–7.
Vazquez JA, Skiest DJ, Nieto L, Northland R, Sanne I, Gogate J, et al. A multicenter randomized trial evaluating posaconazole versus fluconazole for the treatment of oropharyngeal candidiasis in subjects with HIV/AIDS. Clin Infect Dis. 2006;42:1179–86. doi:10.1086/501457.
Barbaro G, Barbarini G, Di Lorenzo G. Fluconazole compared with itraconazole in the treatment of esophageal candidiasis in AIDS patients: a double-blind, randomized, controlled clinical study. Scand J Infect Dis. 1995;27:613–7.
Ally R, Schurmann D, Kreisel W, Carosi G, Aguirrebengoa K, Dupont B, et al. A randomized, double-blind, double-dummy, multicenter trial of voriconazole and fluconazole in the treatment of esophageal candidiasis in immunocompromised patients. Clin Infect Dis. 2001;33:1447–54. doi:10.1086/322653.
Phillips P, De Beule K, Frechette G, Tchamouroff S, Vandercam B, Weitner L, et al. A double-blind comparison of itraconazole oral solution and fluconazole capsules for the treatment of oropharyngeal candidiasis in patients with AIDS. Clin Infect Dis. 1998;26:1368–73.
Ruhnke M. Mucosal and systemic fungal infections in patients with AIDS: prophylaxis and treatment. Drugs. 2004;64:1163–80 64112 [pii].
Hamza OJ, Matee MI, Bruggemann RJ, Moshi MJ, Simon EN, Mugusi F, et al. Single-dose fluconazole versus standard 2-week therapy for oropharyngeal candidiasis in HIV-infected patients: a randomized, double-blind, double-dummy trial. Clin Infect Dis. 2008;47:1270–6. doi:10.1086/592578.
Chave JP, Cajot A, Bille J, Glauser MP. Single-dose therapy for oral candidiasis with fluconazole in HIV-infected adults: a pilot study. J Infect Dis. 1989;159:806–7.
Cartledge JD, Midgley J, Youle M, Gazzard BG. Itraconazole cyclodextrin solution-effective treatment for HIV-related candidosis unresponsive to other azole therapy. J Antimicrob Chemother. 1994;33:1071–3.
Hegener P, Troke PF, Fatkenheuer G, Diehl V, Ruhnke M. Treatment of fluconazole-resistant candidiasis with voriconazole in patients with AIDS. AIDS. 1998;12:2227–8.
Skiest DJ, Vazquez JA, Anstead GM, Graybill JR, Reynes J, Ward D, et al. Posaconazole for the treatment of azole-refractory oropharyngeal and esophageal candidiasis in subjects with HIV infection. Clin Infect Dis. 2007;44:607–14. doi:10.1086/511039.
Vazquez JA, Skiest DJ, Tissot-Dupont H, Lennox JL, Boparai N, Isaacs R. Safety and efficacy of posaconazole in the long-term treatment of azole-refractory oropharyngeal and esophageal candidiasis in patients with HIV infection. HIV Clin Trials. 2007;8:86–97. doi:10.1310/hct0802-86.
Penk A, Pittrow L. High-dose therapy with fluconazole >or =800 mg/day. Review. Mycoses. 1997;40:33–42.
Villanueva A, Gotuzzo E, Arathoon EG, Noriega LM, Kartsonis NA, Lupinacci RJ, et al. A randomized double-blind study of caspofungin versus fluconazole for the treatment of esophageal candidiasis. Am J Med. 2002;113:294–9.
de Wet NT, Bester AJ, Viljoen JJ, Filho F, Suleiman JM, Ticona E et al. A randomized, double blind, comparative trial of micafungin (FK463) vs. fluconazole for the treatment of oesophageal candidiasis. Aliment Pharmacol Ther. 2005;21(7):899–907. doi:10.1111/j.1365-2036.2005.02427.x.
Krause DS, Simjee AE, van Rensburg C, Viljoen J, Walsh TJ, Goldstein BP, et al. A randomized, double-blind trial of anidulafungin versus fluconazole for the treatment of esophageal candidiasis. Clin Infect Dis. 2004;39:770–5. doi:10.1086/423378.
Vazquez JA, Schranz JA, Clark K, Goldstein BP, Reboli A, Fichtenbaum C. A phase 2, open-label study of the safety and efficacy of intravenous anidulafungin as a treatment for azole-refractory mucosal candidiasis. J Acquir Immune Defic Syndr. 2008;48:304–9. doi:10.1097/QAI.0b013e31817af47a.
Villanueva A, Arathoon EG, Gotuzzo E, Berman RS, DiNubile MJ, Sable CA. A randomized double-blind study of caspofungin versus amphotericin for the treatment of candidal esophagitis. Clin Infect Dis. 2001;33:1529–35. doi:10.1086/323401.
Valdez H, Gripshover BM, Salata RA, Lederman MM. Resolution of azole-resistant oropharyngeal candidiasis after initiation of potent combination antiretroviral therapy. AIDS. 1998;12:538.
Martins MD, Lozano-Chiu M, Rex JH. Declining rates of oropharyngeal candidiasis and carriage of Candida albicans associated with trends toward reduced rates of carriage of fluconazole-resistant C. albicans in human immunodeficiency virus-infected patients. Clin Infect Dis. 1998;27:1291–4.
Barasch A, Safford MM, Dapkute-Marcus I, Fine DH. Efficacy of chlorhexidine gluconate rinse for treatment and prevention of oral candidiasis in HIV-infected children: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:204–7. doi:10.1016/S1079210403005651.
Nittayananta W, DeRouen TA, Arirachakaran P, Laothumthut T, Pangsomboon K, Petsantad S, et al. A randomized clinical trial of chlorhexidine in the maintenance of oral candidiasis-free period in HIV infection. Oral Dis. 2008;14:665–70. doi:10.1111/j.1601-0825.2008.01449.x.
Revankar SG, Kirkpatrick WR, McAtee RK, Dib OP, Fothergill AW, Redding SW, et al. Detection and significance of fluconazole resistance in oropharyngeal candidiasis in human immunodeficiency virus-infected patients. J Infect Dis. 1996;174:821–7.
Fan-Havard P, Capano D, Smith SM, Mangia A, Eng RH. Development of resistance in candida isolates from patients receiving prolonged antifungal therapy. Antimicrob Agents Chemother. 1991;35:2302–5.
Goldman M, Cloud GA, Wade KD, Reboli AC, Fichtenbaum CJ, Hafner R, et al. A randomized study of the use of fluconazole in continuous versus episodic therapy in patients with advanced HIV infection and a history of oropharyngeal candidiasis: AIDS Clinical Trials Group Study 323/Mycoses Study Group Study 40. Clin Infect Dis. 2005;41:1473–80. doi:10.1086/497373.
Chen XS, Han GZ, Guo ZP, Lu NZ, Chen J, Wang JB. A comparison of topical application of penciclovir 1% cream with acyclovir 3% cream for treatment of genital herpes: a randomized, double-blind, multicentre trial. Int J STD AIDS. 2000;11:568–73.
Levin MJ, Bacon TH, Leary JJ. Resistance of herpes simplex virus infections to nucleoside analogues in HIV-infected patients. Clin Infect Dis. 2004;39:S248–57. doi:10.1086/422364.
Phiri S, Hoffman IF, Weiss HA, Martinson F, Nyirenda N, Kamwendo D, et al. Impact of aciclovir on ulcer healing, lesional, genital and plasma HIV-1 RNA among patients with genital ulcer disease in Malawi. Sex Transm Infect. 2010;86:345–52. doi:10.1136/sti.2009.041814.
Ormrod D, Scott LJ, Perry CM. Valaciclovir: a review of its long term utility in the management of genital herpes simplex virus and cytomegalovirus infections. Drugs. 2000;59:839–63.
Conant MA, Schacker TW, Murphy RL, Gold J, Crutchfield LT, Crooks RJ. Valaciclovir versus aciclovir for herpes simplex virus infection in HIV-infected individuals: two randomized trials. Int J STD AIDS. 2002;13:12–21.
Vinh DC, Aoki FY. Famciclovir for the treatment of recurrent genital herpes: a clinical and pharmacological perspective. Expert Opin Pharmacother. 2006;7:2271–86. doi:10.1517/14656566.7.16.2271.
Bodsworth N, Bloch M, McNulty A, Denham I, Doong N, Trottier S, et al. 2-day versus 5-day famciclovir as treatment of recurrences of genital herpes: results of the FaST study. Sex Health. 2008;5:219–25 SH08013 [pii].
Safrin S. Treatment of acyclovir-resistant herpes simplex virus infections in patients with AIDS. J Acquir Immune Defic Syndr. 1992;5:S29–32.
Ioannidis JP, Collier AC, Cooper DA, Corey L, Fiddian AP, Gazzard BG, et al. Clinical efficacy of high-dose acyclovir in patients with human immunodeficiency virus infection: a meta-analysis of randomized individual patient data. J Infect Dis. 1998;178:349–59.
DeJesus E, Wald A, Warren T, Schacker TW, Trottier S, Shahmanesh M, et al. Valacyclovir for the suppression of recurrent genital herpes in human immunodeficiency virus-infected subjects. J Infect Dis. 2003;188:1009–16. doi:10.1086/378416.
Warren T, Harris J, Brennan CA. Efficacy and safety of valacyclovir for the suppression and episodic treatment of herpes simplex virus in patients with HIV. Clin Infect Dis. 2004;39:S258–66. doi:10.1086/422362.
Freeman EE, Weiss HA, Glynn JR, Cross PL, Whitworth JA, Hayes RJ. Herpes simplex virus 2 infection increases HIV acquisition in men and women: systematic review and meta-analysis of longitudinal studies. AIDS. 2006;20:73–83.
Celum C, Wald A, Hughes J, Sanchez J, Reid S, Delany-Moretlwe S, et al. Effect of aciclovir on HIV-1 acquisition in herpes simplex virus 2 seropositive women and men who have sex with men: a randomised, double-blind, placebo-controlled trial. Lancet. 2008;371:2109–19. doi:10.1016/S0140-6736(08)60920-4.
Celum C, Wald A, Lingappa JR, Magaret AS, Wang RS, Mugo N, et al. Acyclovir and transmission of HIV-1 from persons infected with HIV-1 and HSV-2. N Engl J Med. 2010;362:427–39. doi:10.1056/NEJMoa0904849.
Watson-Jones D, Weiss HA, Rusizoka M, Changalucha J, Baisley K, Mugeye K, et al. Effect of herpes simplex suppression on incidence of HIV among women in Tanzania. N Engl J Med. 2008;358:1560–71. doi:10.1056/NEJMoa0800260.
Gnann JW Jr, Whitley RJ. Clinical practice. Herpes zoster. N Engl J Med. 2002;347:340–6. doi:10.1056/NEJMcp013211.
Li Q, Chen N, Yang J, Zhou M, Zhou D, Zhang Q et al. Antiviral treatment for preventing postherpetic neuralgia. Cochrane Database Syst Rev. 2009(2):CD006866. doi:10.1002/14651858.CD006866.pub2.
Gershon AA. Prevention and treatment of VZV infections in patients with HIV. Herpes. 2001;8:32–6.
Saint-Leger E, Caumes E, Breton G, Douard D, Saiag P, Huraux JM, et al. Clinical and virologic characterization of acyclovir-resistant varicella-zoster viruses isolated from 11 patients with acquired immunodeficiency syndrome. Clin Infect Dis. 2001;33:2061–7. doi:10.1086/324503.
Albrecht H, Hoffmann C, Degen O, Stoehr A, Plettenberg A, Mertenskotter T, et al. Highly active antiretroviral therapy significantly improves the prognosis of patients with HIV-associated progressive multifocal leukoencephalopathy. AIDS. 1998;12:1149–54.
Hernandez B, Dronda F, Moreno S. Treatment options for AIDS patients with progressive multifocal leukoencephalopathy. Expert Opin Pharmacother. 2009;10:403–16. doi:10.1517/14656560802707994.
Clifford DB, Yiannoutsos C, Glicksman M, Simpson DM, Singer EJ, Piliero PJ, et al. HAART improves prognosis in HIV-associated progressive multifocal leukoencephalopathy. Neurology. 1999;52:623–5.
Dworkin MS, Wan PC, Hanson DL, Jones JL. Progressive multifocal leukoencephalopathy: improved survival of human immunodeficiency virus-infected patients in the protease inhibitor era. J Infect Dis. 1999;180:621–5. doi:10.1086/314937.
Tantisiriwat W, Tebas P, Clifford DB, Powderly WG, Fichtenbaum CJ. Progressive multifocal leukoencephalopathy in patients with AIDS receiving highly active antiretroviral therapy. Clin Infect Dis. 1999;28:1152–4. doi:10.1086/514762.
Berenguer J, Miralles P, Arrizabalaga J, Ribera E, Dronda F, Baraia-Etxaburu J, et al. Clinical course and prognostic factors of progressive multifocal leukoencephalopathy in patients treated with highly active antiretroviral therapy. Clin Infect Dis. 2003;36:1047–52. doi:10.1086/374048.
Tan K, Roda R, Ostrow L, McArthur J, Nath A. PML-IRIS in patients with HIV infection: clinical manifestations and treatment with steroids. Neurology. 2009;72:1458–64. doi:10.1212/01.wnl.0000343510.08643.74.
Marzocchetti A, Tompkins T, Clifford DB, Gandhi RT, Kesari S, Berger JR, et al. Determinants of survival in progressive multifocal leukoencephalopathy. Neurology. 2009;73:1551–8. doi: 10.1212/WNL.0b013e3181c0d4a1.
Focosi D, Marco T, Kast RE, Maggi F, Ceccherini-Nelli L, Petrini M. Progressive multifocal leukoencephalopathy: what’s new? Neuroscientist. 2010;16:308–23. doi: 10.1177/1073858409356594.
Hall CD, Dafni U, Simpson D, Clifford D, Wetherill PE, Cohen B, et al. Failure of cytarabine in progressive multifocal leukoencephalopathy associated with human immunodeficiency virus infection. AIDS Clinical Trials Group 243 Team. N Engl J Med. 1998;338:1345–51. doi:10.1056/NEJM199805073381903.
Andrei G, Snoeck R, Vandeputte M, De Clercq E. Activities of various compounds against murine and primate polyomaviruses. Antimicrob Agents Chemother. 1997;41:587–93.
Nukuzuma S, Nakamichi K, Nukuzuma C, Takegami T. Inhibitory effect of serotonin antagonists on JC virus propagation in a carrier culture of human neuroblastoma cells. Microbiol Immunol. 2009;53:496–501. doi:10.1111/j.1348-0421.2009.00156.x.
Chapagain ML, Sumibcay L, Gurjav U, Kaufusi PH, Kast RE, Nerurkar VR. Serotonin receptor 2A blocker (risperidone) has no effect on human polyomavirus JC infection of primary human fetal glial cells. J Neurovirol. 2008;14:448–54. doi:10.1080/13550280802235916.
Verma S, Cikurel K, Koralnik IJ, Morgello S, Cunningham-Rundles C, Weinstein ZR, et al. Mirtazapine in progressive multifocal leukoencephalopathy associated with polycythemia vera. J Infect Dis. 2007;196:709–11. doi:10.1086/520514.
Focosi D, Kast RE, Maggi F, Ceccherini-Nelli L, Petrini M. Risperidone-induced reduction in JC viruria as a surrogate marker for efficacy against progressive multifocal leukoencephalopathy and hemorrhagic cystitis. J Clin Virol. 2007;39:63–4. doi:10.1016/j.jcv.2007.03.001.
Focosi D, Kast RE, Maggi F, Lauria G, Ceccherini-Nelli L, Petrini M. 5-HT2a inhibitors for progressive multifocal leukoencephalopathy: old drugs for an old disease. J Infect Dis. 2008;197(2):328; author reply -9. doi:10.1086/524877.
Cettomai D, McArthur JC. Mirtazapine use in human immunodeficiency virus-infected patients with progressive multifocal leukoencephalopathy. Arch Neurol. 2009;66:255–8. doi:10.1001/archneurol.2008.557.
Brickelmaier M, Lugovskoy A, Kartikeyan R, Reviriego-Mendoza MM, Allaire N, Simon K, et al. Identification and characterization of mefloquine efficacy against JC virus in vitro. Antimicrob Agents Chemother. 2009;53:1840–9. doi:10.1128/AAC.01614-08.
Colford JM Jr, Tager IB, Hirozawa AM, Lemp GF, Aragon T, Petersen C. Cryptosporidiosis among patients infected with human immunodeficiency virus. Factors related to symptomatic infection and survival. Am J Epidemiol. 1996;144:807–16.
McGowan I, Hawkins AS, Weller IV. The natural history of cryptosporidial diarrhoea in HIV-infected patients. AIDS. 1993;7:349–54.
Jablonowski H, Szelenyi H, Becker K, Lubke HJ, Borchard F, Strohmeyer G, et al. Sclerosing cholangitis with papillary stenosis in an HIV-infected patients with Cryptosporidium infection. Z Gastroenterol. 1994;32:441–3.
Hashmey R, Smith NH, Cron S, Graviss EA, Chappell CL, White AC, Jr. Cryptosporidiosis in Houston, Texas. A report of 95 cases. Medicine (Baltimore). 1997;76(2):118–39.
Gross TL, Wheat J, Bartlett M, O’Connor KW. AIDS and multiple system involvement with cryptosporidium. Am J Gastroenterol. 1986;81:456–8.
Travis WD, Schmidt K, MacLowry JD, Masur H, Condron KS, Fojo AT. Respiratory cryptosporidiosis in a patient with malignant lymphoma. Report of a case and review of the literature. Arch Pathol Lab Med. 1990;114:519–22.
Carr A, Marriott D, Field A, Vasak E, Cooper DA. Treatment of HIV-1-associated microsporidiosis and cryptosporidiosis with combination antiretroviral therapy. Lancet. 1998;351:256–61. doi:10.1016/S0140-6736(97)07529-6.
Miao YM, Awad-El-Kariem FM, Franzen C, Ellis DS, Muller A, Counihan HM, et al. Eradication of cryptosporidia and microsporidia following successful antiretroviral therapy. J Acquir Immune Defic Syndr. 2000;25:124–9.
Abubakar I, Aliyu SH, Arumugam C, Hunter PR, Usman NK. Prevention and treatment of cryptosporidiosis in immunocompromised patients. Cochrane Database Syst Rev. 2007(1):CD004932. doi:10.1002/14651858.CD004932.pub2.
Gathe JC Jr, Mayberry C, Clemmons J, Nemecek J. Resolution of severe cryptosporidial diarrhea with rifaximin in patients with AIDS. J Acquir Immune Defic Syndr. 2008;48:363–4. doi:10.1097/QAI.0b013e31817beb78.
Rossignol JF, Ayoub A, Ayers MS. Treatment of diarrhea caused by Cryptosporidium parvum: a prospective randomized, double-blind, placebo-controlled study of Nitazoxanide. J Infect Dis. 2001;184:103–6. doi:10.1086/321008.
Amadi B, Mwiya M, Sianongo S, Payne L, Watuka A, Katubulushi M, et al. High dose prolonged treatment with nitazoxanide is not effective for cryptosporidiosis in HIV positive Zambian children: a randomised controlled trial. BMC Infect Dis. 2009;9:195. doi:10.1186/1471-2334-9-195.
White AC Jr, Cron SG, Chappell CL. Paromomycin in cryptosporidiosis. Clin Infect Dis. 2001;32:1516–7. doi:10.1086/320171.
Hewitt RG, Yiannoutsos CT, Higgs ES, Carey JT, Geiseler PJ, Soave R, et al. Paromomycin: no more effective than placebo for treatment of cryptosporidiosis in patients with advanced human immunodeficiency virus infection. AIDS Clinical Trial Group. Clin Infect Dis. 2000;31:1084–92. doi:10.1086/318155.
Holmberg SD, Moorman AC, Von Bargen JC, Palella FJ, Loveless MO, Ward DJ, et al. Possible effectiveness of clarithromycin and rifabutin for cryptosporidiosis chemoprophylaxis in HIV disease. HIV Outpatient Study (HOPS) Investigators. JAMA. 1998;279(5):384–6.
Leenders AC, Reiss P, Portegies P, Clezy K, Hop WC, Hoy J, et al. Liposomal amphotericin B (AmBisome) compared with amphotericin B both followed by oral fluconazole in the treatment of AIDS-associated cryptococcal meningitis. AIDS. 1997;11:1463–71.
Sloan D, Dlamini S, Dedicoat M. Management of cryptoccocal meningitis in resource-limited settings: a systematic review. S Afr Med J. 2009;99:310–2.
Just-Nubling G. Therapy of candidiasis and cryptococcosis in AIDS. Mycoses. 1994;37:56–63.
Brouwer AE, Rajanuwong A, Chierakul W, Griffin GE, Larsen RA, White NJ, et al. Combination antifungal therapies for HIV-associated cryptococcal meningitis: a randomised trial. Lancet. 2004;363:1764–7. doi:10.1016/S0140-6736(04)16301-0.
Nussbaum JC, Jackson A, Namarika D, Phulusa J, Kenala J, Kanyemba C, et al. Combination flucytosine and high-dose fluconazole compared with fluconazole monotherapy for the treatment of cryptococcal meningitis: a randomized trial in Malawi. Clin Infect Dis. 2010;50:338–44. doi:10.1086/649861.
van der Horst CM, Saag MS, Cloud GA, Hamill RJ, Graybill JR, Sobel JD, et al. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. National Institute of Allergy and Infectious Diseases Mycoses Study Group and AIDS Clinical Trials Group. N Engl J Med. 1997;337:15–21. doi:10.1056/NEJM199707033370103.
Pitisuttithum P, Negroni R, Graybill JR, Bustamante B, Pappas P, Chapman S, et al. Activity of posaconazole in the treatment of central nervous system fungal infections. J Antimicrob Chemother. 2005;56:745–55. doi:10.1093/jac/dki288.
Perfect JR, Marr KA, Walsh TJ, Greenberg RN, DuPont B, de la Torre-Cisneros J, et al. Voriconazole treatment for less-common, emerging, or refractory fungal infections. Clin Infect Dis. 2003;36:1122–31. doi:10.1086/374557.
Pappas PG, Bustamante B, Ticona E, Hamill RJ, Johnson PC, Reboli A, et al. Recombinant interferon- gamma 1b as adjunctive therapy for AIDS-related acute cryptococcal meningitis. J Infect Dis. 2004;189:2185–91. doi:10.1086/420829.
Powderly WG, Finkelstein D, Feinberg J, Frame P, He W, van der Horst C, et al. A randomized trial comparing fluconazole with clotrimazole troches for the prevention of fungal infections in patients with advanced human immunodeficiency virus infection. NIAID AIDS Clinical Trials Group. N Engl J Med. 1995;332:700–5. doi:10.1056/NEJM199503163321102.
Lortholary O, Poizat G, Zeller V, Neuville S, Boibieux A, Alvarez M, et al. Long-term outcome of AIDS-associated cryptococcosis in the era of combination antiretroviral therapy. AIDS. 2006;20:2183–91. doi:10.1097/01.aids.0000252060.80704.68.
Buchacz K, Baker RK, Palella FJ Jr, Chmiel JS, Lichtenstein KA, Novak RM, et al. AIDS-defining opportunistic illnesses in US patients, 1994–2007: a cohort study. AIDS. 2010;24:1549–59. doi:10.1097/QAD.0b013e32833a3967.
Karakousis PC, Moore RD, Chaisson RE. Mycobacterium avium complex in patients with HIV infection in the era of highly active antiretroviral therapy. Lancet Infect Dis. 2004;4:557–65. doi:10.1016/S1473-3099(04)01130-2.
Lange CG, Woolley IJ, Brodt RH. Disseminated Mycobacterium avium-intracellulare complex (MAC) infection in the era of effective antiretroviral therapy: is prophylaxis still indicated? Drugs. 2004;64:679–92.
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367–416. doi:10.1164/rccm.200604-571ST.
Dunne M, Fessel J, Kumar P, Dickenson G, Keiser P, Boulos M, et al. A randomized, double-blind trial comparing azithromycin and clarithromycin in the treatment of disseminated Mycobacterium avium infection in patients with human immunodeficiency virus. Clin Infect Dis. 2000;31:1245–52. doi:10.1086/317468.
Benson CA, Williams PL, Currier JS, Holland F, Mahon LF, MacGregor RR, et al. A prospective, randomized trial examining the efficacy and safety of clarithromycin in combination with ethambutol, rifabutin, or both for the treatment of disseminated Mycobacterium avium complex disease in persons with acquired immunodeficiency syndrome. Clin Infect Dis. 2003;37:1234–43. doi:10.1086/378807.
Boulanger C, Hollender E, Farrell K, Stambaugh JJ, Maasen D, Ashkin D, et al. Pharmacokinetic evaluation of rifabutin in combination with lopinavir-ritonavir in patients with HIV infection and active tuberculosis. Clin Infect Dis. 2009;49:1305–11. doi:10.1086/606056.
Chaisson RE, Benson CA, Dube MP, Heifets LB, Korvick JA, Elkin S, et al. Clarithromycin therapy for bacteremic Mycobacterium avium complex disease. A randomized, double-blind, dose-ranging study in patients with AIDS. AIDS Clinical Trials Group Protocol 157 Study Team. Ann Intern Med. 1994;121:905–11.
Cohn DL, Fisher EJ, Peng GT, Hodges JS, Chesnut J, Child CC, et al. A prospective randomized trial of four three-drug regimens in the treatment of disseminated Mycobacterium avium complex disease in AIDS patients: excess mortality associated with high-dose clarithromycin. Terry Beirn Community Programs for Clinical Research on AIDS. Clin Infect Dis. 1999;29:125–33. doi:10.1086/520141.
Ward TT, Rimland D, Kauffman C, Huycke M, Evans TG, Heifets L. Randomized, open-label trial of azithromycin plus ethambutol vs. clarithromycin plus ethambutol as therapy for Mycobacterium avium complex bacteremia in patients with human immunodeficiency virus infection. Veterans Affairs HIV Research Consortium. Clin Infect Dis. 1998;27:1278–85.
Havlir DV, Schrier RD, Torriani FJ, Chervenak K, Hwang JY, Boom WH. Effect of potent antiretroviral therapy on immune responses to Mycobacterium avium in human immunodeficiency virus-infected subjects. J Infect Dis. 2000;182:1658–63. doi:10.1086/317620.
Phillips P, Bonner S, Gataric N, Bai T, Wilcox P, Hogg R, et al. Nontuberculous mycobacterial immune reconstitution syndrome in HIV-infected patients: spectrum of disease and long-term follow-up. Clin Infect Dis. 2005;41:1483–97. doi:10.1086/497269.
Jt Riddell, Kaul DR, Karakousis PC, Gallant JE, Mitty J, Kazanjian PH. Mycobacterium avium complex immune reconstitution inflammatory syndrome: long term outcomes. J Transl Med. 2007;5:50. doi:10.1186/1479-5876-5-50.
Havlir DV, Dube MP, Sattler FR, Forthal DN, Kemper CA, Dunne MW, et al. Prophylaxis against disseminated Mycobacterium avium complex with weekly azithromycin, daily rifabutin, or both. California Collaborative Treatment Group. N Engl J Med. 1996;335:392–8. doi:10.1056/NEJM199608083350604.
Nightingale SD, Byrd LT, Southern PM, Jockusch JD, Cal SX, Wynne BA. Incidence of Mycobacterium avium-intracellulare complex bacteremia in human immunodeficiency virus-positive patients. J Infect Dis. 1992;165:1082–5.
Oldfield EC 3rd, Fessel WJ, Dunne MW, Dickinson G, Wallace MR, Byrne W, et al. Once weekly azithromycin therapy for prevention of Mycobacterium avium complex infection in patients with AIDS: a randomized, double-blind, placebo-controlled multicenter trial. Clin Infect Dis. 1998;26:611–9.
Pierce M, Crampton S, Henry D, Heifets L, LaMarca A, Montecalvo M, et al. A randomized trial of clarithromycin as prophylaxis against disseminated Mycobacterium avium complex infection in patients with advanced acquired immunodeficiency syndrome. N Engl J Med. 1996;335:384–91. doi:10.1056/NEJM199608083350603.
Lundgren JD, Phillips AN, Vella S, Katlama C, Ledergerber B, Johnson AM, et al. Regional differences in use of antiretroviral agents and primary prophylaxis in 3122 European HIV-infected patients. EuroSIDA Study Group. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;16:153–60.
Ackah AN, Coulibaly D, Digbeu H, Diallo K, Vetter KM, Coulibaly IM, et al. Response to treatment, mortality, and CD4 lymphocyte counts in HIV-infected persons with tuberculosis in Abidjan. Cote d’Ivoire. Lancet. 1995;345:607–10.
Wood R, Maartens G, Lombard CJ. Risk factors for developing tuberculosis in HIV-1-infected adults from communities with a low or very high incidence of tuberculosis. J Acquir Immune Defic Syndr. 2000;23:75–80.
Sonnenberg P, Murray J, Glynn JR, Shearer S, Kambashi B, Godfrey-Faussett P. HIV-1 and recurrence, relapse, and reinfection of tuberculosis after cure: a cohort study in South African mineworkers. Lancet. 2001;358:1687–93. doi:10.1016/S0140-6736(01)06712-5.
Breen RA, Miller RF, Gorsuch T, Smith CJ, Schwenk A, Holmes W, et al. Adverse events and treatment interruption in tuberculosis patients with and without HIV co-infection. Thorax. 2006;61:791–4. doi:10.1136/thx.2006.058867.
Dheda K, Lampe FC, Johnson MA, Lipman MC. Outcome of HIV-associated tuberculosis in the era of highly active antiretroviral therapy. J Infect Dis. 2004;190:1670–6. doi:10.1086/424676.
Burman WJ, Jones BE. Treatment of HIV-related tuberculosis in the era of effective antiretroviral therapy. Am J Respir Crit Care Med. 2001;164:7–12.
Abdool Karim SS, Naidoo K, Grobler A, Padayatchi N, Baxter C, Gray A et al. Timing of initiation of antiretroviral drugs during tuberculosis therapy. N Engl J Med. 2010;362(8):697–706. doi:10.1056/NEJMoa0905848.
Torok ME, Farrar JJ. When to start antiretroviral therapy in HIV-associated tuberculosis. N Engl J Med. 2011;365:1538–40. doi:10.1056/NEJMe1109546.
Michailidis C, Pozniak AL, Mandalia S, Basnayake S, Nelson MR, Gazzard BG. Clinical characteristics of IRIS syndrome in patients with HIV and tuberculosis. Antivir Ther. 2005;10:417–22.
European AIDS Clinical Society (EACS). Clinical management and treatment of HIV infected adults in Europe, version 5. 2009. Available at: http://wwweuropeanaidsclinicalsocietyorg.
Office of AIDS Research Advisory Council (OARAC). Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services, National Institutes of Health, Bethesda. 2009:1–161. Available at: http://wwwaidsinfonihgov/ContentFiles/AdultandAdolescentGLpdf
Wenning LA, Hanley WD, Brainard DM, Petry AS, Ghosh K, Jin B, et al. Effect of rifampin, a potent inducer of drug-metabolizing enzymes, on the pharmacokinetics of raltegravir. Antimicrob Agents Chemother. 2009;53:2852–6. doi:10.1128/AAC.01468-08.
Boyd MA, Zhang X, Dorr A, Ruxrungtham K, Kolis S, Nieforth K, et al. Lack of enzyme-inducing effect of rifampicin on the pharmacokinetics of enfuvirtide. J Clin Pharmacol. 2003;43:1382–91. doi:10.1177/0091270003259220.
Dean GL, Edwards SG, Ives NJ, Matthews G, Fox EF, Navaratne L, et al. Treatment of tuberculosis in HIV-infected persons in the era of highly active antiretroviral therapy. AIDS. 2002;16:75–83.
Havlir DV, Kendall MA, Ive P, Kumwenda J, Swindells S, Qasba SS, et al. Timing of antiretroviral therapy for HIV-1 infection and tuberculosis. N Engl J Med. 2011;365:1482–91. doi:10.1056/NEJMoa1013607.
Centers for Disease Control and Prevention (CDC). Treatment of latent tuberculosis infection (LTBI). 2007. Available at: http://wwwcdcgov/tb/publications/factsheets/treatment/treatmentLTBIhtm
Aichelburg MC, Rieger A, Breitenecker F, Pfistershammer K, Tittes J, Eltz S, et al. Detection and prediction of active tuberculosis disease by a whole-blood interferon-gamma release assay in HIV-1-infected individuals. Clin Infect Dis. 2009;48:954–62. doi:10.1086/597351.
Centers for Disease Control and Prevention (CDC). Managing drug interactions in the treatment of HIV-related tuberculosis. Division of Tuberculosis Elimination National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. 2007. Available at: http://wwwcdcgov/tb/publications/guidelines/TB_HIV_Drugs/defaulthtm
Woldehanna S, Volmink J. Treatment of latent tuberculosis infection in HIV infected persons. Cochrane Database Syst Rev. 2004(1):CD000171. doi:10.1002/14651858.CD000171.pub2.
Eker B, Ortmann J, Migliori GB, Sotgiu G, Muetterlein R, Centis R, et al. Multidrug- and extensively drug-resistant tuberculosis. Germany. Emerg Infect Dis. 2008;14:1700–6.
World Health Organization (HO). Multidrug and extensively drug-resistant TB (M/XDR-TB): 2010 global report on surveillance and response. WHO/HTM/TB/2010.3. 2010. WHO, Geneva; available at: http://wwwwhoint/tb/en/
Acknowledgments
We are indepted to Fiona Diekhoff for translation and preparation of the manuscript.
Conflict of interests
Conflict of Interest statements of all authors are published online: http://daignet.de/site-content/hiv-therapie/leitlinien-1/Ubersicht%20Conflict%20of%20Interests%202011%20bis%202013.pdf or http://www.awmf.org/fileadmin/user_upload/Leitlinien/055_D_Aids-Ges/055-006i_S2k_Opportunistische_Infektionen_bei_HIV_infizierten_Patienten_2011_03.pdf.All. All other authors declare no conflicts of interest.
This supplement was not sponsored by industry, it was sponsored by KAAD (Klinische Arbeitsgemeinschaft AIDS Deutschland).
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Contributors to this guideline (alphabetical order): J. Bogner, N.H. Brockmeyer, S. Esser, K. Grabmeier-Pfistershammer, B. Haas, K. Hahn, G. Härter, M. Hartmann, C. Herzmann, C. Hoffmann, J. Hutterer, A. R. Jordan. C. Lange, S. Mauss, D. Meyer-Olson, F. Mosthaf, M. Oette, A. Potthoff, S. Reuter, A. Rieger, T. Rosenkranz, M. Ruhnke, B. Schaaf, S. Schwarze, H.J. Stellbrink, H. Stocker, A. Stoehr, M. Stoll, J. Thoden, C. Träder, M. Vogel, D. Wagner, C. Wyen.
Memberships of the authors: American Society of Cancer Oncology (ASCO), Berufsverband Niedergelassener Gastroenterologen (BNG), Deutsche Arbeitsgemeinschaft niedergelassener Ärzte in der Versorgung HIV-Infizierter (DAGNÄ), Deutsche AIDS Gesellschaft (DAIG), Deutsche Dermatologische Gesellschaft (DDG), Deutsche Gesellschaft für Immunologie (DGFI), Deutsche Gesellschaft für Hämatologie und Onkologie (DGHO), Deutsche Gesellschaft für Infektiologie (DGI), Deutsche Gesellschaft für Innere Medizin (DGIM), Deutsche Gesellschaft für Neurowissenschaftliche Begutachtung (DGNB), Deutsche Gesellschaft für Pneumologie (DGP), Deutsche Gesellschaft für Rheumatologie (DGRh), Deutsche Gesellschaft für Verdauungs- und Stoffwechselkrankheiten (DGVS), Deutschsprachige Mykologische Gesellschaft (DMYKG), Deutsche Neuro-AIDS Arbeitsgemeinschaft (DNAA), Deutsche STI-Gesellschaft (DSTDG), European AIDS Clinical Society (EACS), European Association for the Study of the Liver (EASL), European Respiratory Society (ERS), European Society for Medical Oncology (ESMO), Gesellschaft für Virologie (GfV), Klinische Arbeitsgemeinschaft AIDS Deutschland (KAAD), Österreichische AIDS Gesellschaft (ÖAG), Paul Ehrlich Gesellschaft (PEG).
Consensus version of this guideline by the KAAD approved on 25 June 2010 in Cologne by: N. Baerlecken, J. Bogner, M. Oette, N. Brockmeyer, D. Ernst, S. Esser, B. Haas, M. Hartmann, G. Härter, C. Hoffmann, I. Husstedt, A. Potthoff, B. Schaaf, H. Stocker, A. Stoehr, M. Stoll, J. Thoden, C. Träder, C. Wyen.
Final consent to this version given by the DAIG members on 17 March 2011 in Munich (43 members, final vote of 36 positive unanimous votes).
Final consent to this version by the steering committee of the ÖAG given on 9 November 2011.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Thoden, J., Potthoff, A., Bogner, J.R. et al. Therapy and prophylaxis of opportunistic infections in HIV-infected patients: a guideline by the German and Austrian AIDS societies (DAIG/ÖAG) (AWMF 055/066). Infection 41 (Suppl 2), 91–115 (2013). https://doi.org/10.1007/s15010-013-0504-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-013-0504-1