Abstract
Background
The objective of this study was to evaluate the mortality of and risk factors for bacteriuria due to carbapenem-resistant Klebsiella pneumoniae (CRKp) versus carbapenem-susceptible K. pneumoniae (CSKp) producing extended spectrum β lactamase (ESBL).
Methods
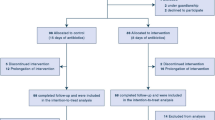
This was a retrospective case–control study in which 135 case-patients with bacteriuria due to CRKp were compared with 127 control patients with CSKp producing ESBL. In a first step, multivariate Cox regression and Kaplan–Meier survival analysis models were used to determine the difference in mortality between the two groups and risk factors for mortality. In a second step, a univariate analysis was used to identify risk factors for CRKp colonization.
Results
There were no significant demographic or clinical differences between the groups. In-hospital mortality in the study and control groups was 29 and 25 %, respectively (non-significant difference). Multivariate analysis revealed that the most important risk factor for mortality in both groups was being bed ridden [hazard ratio 2.2, 95 % confidence interval (CI) 1.23–3.93; P = 0.008]. Patients with CRKp bacteriuria had a longer hospitalization time with a mean ± standard deviation of 28 ± 33 days compared to 22 ± 28 days in the control group (P < 0.05). Several univariate risk factors for acquiring CRKp bacteriuria were identified: antibiotic use [odds ratio (OR) 1.93, 95 % CI 1.18–3.17, p = 0.008], especially colistin (OR 2.04, 95 % CI 1.04–4.02; P = 0.036), presence of a urinary catheter (OR 2.09, 95 % CI 1.2–3.63; P = 0.008), surgery (OR 3.94, 95 % CI 1.85–8.37; P = 0.0002), invasive procedures (OR 3.06, 95 % CI 1.61–5.8; P = 0.0004), and intensive care unit admission (OR 2.49, 95 % CI 1.18–5.37; P = 0.015).
Conclusion
Bacteriuria caused by CRKp as compared that caused by CSKp was not found to be a risk factor for death.

Similar content being viewed by others
References
Meier S, Weber R, Zbinden R, Ruef C, Hasse B. Extended-spectrum beta-lactamase-producing Gram-negative pathogens in community-acquired urinary tract infections: an increasing challenge for antimicrobial therapy. Infection. 2011;39:333–40.
Gona F, Mezzatesta ML, Corona D, Zerbo D, Scriffignano V, Stefani S, Veroux P, Veroux M. Klebsiella pneumoniae ESBL producers responsible for severe UTIs in a renal transplant unit. Infection. 2011;39:83–5.
Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009;9:228–36.
Raveh D, Rudensky B, Huerta M, Aviv Y, Yinnon AM. Use of time-trend analysis in the design of empirical antimicrobial treatment of urinary tract infection. Eur J Clin Microbiol Infect Dis. 2003;22:158–64.
MacKenzie FM, Forbes KJ, Dorai-John T, Amyes SG, Gould IM. Emergence of a carbapenem-resistant Klebsiella pneumoniae. Lancet. 2007;350:783.
Navon-Venezia S, Chmelnitsky I, Leavitt A, Schwaber MJ, Schwartz D, Carmeli Y. Plasmid-mediated imipenem-hydrolyzing enzyme KPC-2 among multiple carbapenem-resistant Escherichia coli clones in Israel. Antimicrob Agents Chemother. 2006;50:3098–101.
Tenover FC, Kalsi RK, Williams PP, et al. Carbapenem resistance in Klebsiella pneumoniae not detected by automated susceptibility testing. Emerg Infect Dis. 2006;12:1209–13.
Schwaber MJ, Lev B, Israeli A, Solter E, Smollan G, Rubinovitch B, Shalit I, Carmeli Y. Containment of a country-wide outbreak of carbapenem resistant Klebsiella pneumoniae in Israeli hospitals via a nationally implemented intervention. Clin Infect Dis. 2011;52:848–55.
Wiener-Well Y, Rudensky B, Yinnon AM, et al. Carriage rate of carbapenem-resistant Klebsiella pneumoniae in hospitalized patients during a national outbreak. J Hosp Infect. 2010;74:344–9.
Falagas ME, Rafailidis PI, Kofteridis D, et al. Risk factors of carbapenem-resistant Klebsiella pneumoniae infections: a matched case control study. J Antimicrob Chemother. 2007;60:1124–30.
Schwaber MJ, Klarfeld-Lidji S, Navon-Venezia S, Schwartz D, Leavitt A, Carmeli Y. Predictors of carbapenem-resistant Klebsiella pneumoniae acquisition among hospitalized adults and effect of acquisition on mortality. Antimicrob Agents Chemother. 2007;52:1028–33.
Ben-David D, Kordevani R, Keller N, Tal I, Marzel A, Gal-Mor O, Maor Y, Rahav G. Outcome of carbapenem resistant Klebsiella pneumoniae bloodstream infections. Clin Microbiol Infect. 2012;18:54–60.
Kwak YG, Choi SH, Choo EJ, et al. Risk factors for the acquisition of carbapenem-resistant Klebsiella pneumoniae among hospitalized patients. Microb Drug Resist. 2005;11:165–9.
Cope M, Cevallos ME, Cadle RM, Darouiche RO, Musher DM, Trautner BW. Inappropriate treatment of catheter-associated asymptomatic bacteriuria in a tertiary care hospital. Clin Infect Dis. 2009;48:1182–8.
Bradford PA, Bratu S, Urban C. Emergence of carbapenem-resistant Klebsiella species possessing the class A carbapenem-hydrolyzing KPC-2 and inhibitor-resistant TEM-30 beta-lactamases in New York City. Clin Infect Dis. 2004;39:55–60.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. 19th International supplement. CLSI document M100-S10. Wayne: Clinical Laboratory Standards Institute; 2009.
Henschke R, Yinnon AM, Rudensky B, Attias D, Raveh D. Assessment of the clinical significance of production of extended-spectrum-β-lactamase (ESBL) by Enterobacteriaceae. Infection. 2006;34:66–74.
Raveh D, Yinnon AM, Broide E, Rudensky B. Susceptibilities of ESBL-producing Enterobacteriaceae to ertapenem, meropenem, and piperacillin-tazobactam, with and without clavulanic acid. Chemotherapy. 2007;53:185–9.
Yinnon AM, Butnaru A, Raveh D, Jerassy Z, Rudensky B. Klebsiella bacteraemia: community versus nosocomial infection. Q J Med. 1996;89:933–41.
Bahagon Y, Raveh D, Schlesinger Y, Rudensky B, Yinnon AM. Prevalence and predictive features of bacteremic urinary tract infection in emergency department patients. Eur J Clin Microbiol Infect Dis. 2007;26:349–52.
Marchi M, Grilli E, Mongardi M, Bedosti C, Nobilio L, Moro ML. Prevalence of infections in long-term care facilities: how to read it? Infection. 2012;40:493–500.
Burke JP. Nosocomial urinary tract infections. In: Mayhall CG, editor. Hospital epidemiology infection control. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2004. p. 267–86.
Salgavo CD. Prevention of catheter associated urinary tract infection. In: Wenzel RP, editor. Prevention and control of nosocomial infections. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2004. p. 297–311.
Borer A, Saidel-Odes L, Riesenberg K, et al. Attributable mortality rate for carbapenem resistant pneumonia bacteremia. Infect Control Hosp Epidemiol. 2009;30:972–6.
Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008;29:1099–106.
Kang CI, Kim SH, Kim DM, et al. Risk factors for and clinical outcomes of bloodstream infections caused by extended-spectrum beta-lactamase-producing Klebsiella pneumoniae. Infect Control Hosp Epidemiol. 2004;25:860–7.
Ben-David D, Maor Y, Keller N, et al. Potential role of active surveillance in the control of a hospital-wide outbreak of carbapenem-resistant Klebsiella pneumoniae infection. Infect Control Hosp Epidemiol. 2010;31:620–6.
Carmeli Y, Akova M, Cornaglia G, et al. Controlling the spread of carbapenemase-producing Gram-negatives; therapeutic approach and infection control. Clin Microbiol Infect. 2010;16:102–11.
Miriagou V, Cornaglia G, Edelstein M, et al. Acquired carbapenemases in Gram-negative bacterial pathogens: detection and surveillance issues. Clin Microbiol Infect. 2010;16:112–22.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shilo, S., Assous, M.V., Lachish, T. et al. Risk factors for bacteriuria with carbapenem-resistant Klebsiella pneumoniae and its impact on mortality: a case–control study. Infection 41, 503–509 (2013). https://doi.org/10.1007/s15010-012-0380-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-012-0380-0