Abstract
Purpose
Rapidly changing medical environments may have changed the microbiology of infected bile. The aim of our study was to identify the changing trends in microorganisms in biliary infections and examine their susceptibilities against currently recommended antibiotics.
Methods
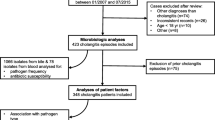
Bile cultures taken between 1998 and 2010 at Seoul National University Hospital, a tertiary medical center, were retrospectively reviewed. From 1,403 patients, 3,425 microorganisms were isolated from 2,217 cultures. The cultures were then tested to determine the types of microorganisms and their antibiotic susceptibility.
Results
The five most frequently isolated microorganisms were Enterococcus (22.7 %) followed by Escherichia (13.2 %), Pseudomonas (10.9 %), Klebsiella (10.3 %), and Enterobacter (7.2 %). The trend in annual incidence indicated a growing emergence of Enterococcus (P < 0.001). Among Enterococcus, E. faecium acquired a dominant position (50.6 %), showing an increasing trend over the study period (P = 0.026). The incidence of vancomycin-resistant Enterococcus also showed an increasing trend (P < 0.001). Many of the commonly used antibiotics provided inadequate coverage for the more frequently encountered microorganisms. Multiple regression revealed that benign causes of obstruction and non-operative treatment harbor an increased risk for enterococcal growth (P = 0.001 and P = 0.027, respectively).
Conclusions
In contrast to earlier reports, we found that Enterococcus has emerged as the most frequently isolated microorganism from bile. The importance of enterococcal infection should be recognized, and currently recommended antibiotics need to be re-evaluated since in our bile cultures most provided inadequate coverage for the more frequently encountered microorganisms. The changes in the trends of microorganisms isolated from bile should be considered in cases where patients present with biliary obstruction.



Similar content being viewed by others
References
Lipsett PA, Pitt HA. Acute cholangitis. Surg Clin N Am. 1990;70:1297–312.
Leung JW, Ling TK, Chan RC, Cheung SW, Lai CW, Sung JJ, et al. Antibiotics, biliary sepsis, and bile duct stones. Gastrointest Endosc. 1994;40:716–21.
Lee DW, Chung SC. Biliary infection. Baillieres Clin Gastroenterol. 1997;11:707–24.
Maluenda F, Csendes A, Burdiles P, Diaz J. Bacteriological study of choledochal bile in patients with common bile duct stones, with or without acute suppurative cholangitis. Hepatogastroenterology. 1989;36:132–5.
Dowidar N, Kolmos HJ, Lyon H, Matzen P. Clogging of biliary endoprostheses. A morphologic and bacteriologic study. Scand J Gastroenterol. 1991;26:1137–44.
Mandell GL, Bennett JE, Dolin R. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 7th ed. Philadelphia: Elsevier; 2010.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: 17th informational supplement. In: Institute CaLS, editor. CLSI document M100S17. Wayne: Clinical and Laboratory Standard Institute; 2007.
Fukunaga FH. Gallbladder bacteriology, histology, and gallstones. Study of unselected cholecystectomy specimens in Honolulu. Arch Surg. 1973;106:169–71.
Chetlin SH, Elliott DW. Biliary bacteremia. Arch Surg. 1971;102:303–7.
Suzuki Y, Kobayashi A, Ohto M, Tsuchiya Y, Saisho H, Kimura K, et al. Bacteriological study of transhepatically aspirated bile. Relation to cholangiographic findings in 295 patients. Dig Dis Sci. 1984;29:109–15.
Melzer M, Toner R, Lacey S, Bettany E, Rait G. Biliary tract infection and bacteraemia: presentation, structural abnormalities, causative organisms and clinical outcomes. Postgrad Med J. 2007;83:773–6. doi:10.1136/pgmj.2007.064683.
Bae WK, Moon YS, Kim JH, Lee SH, Kim NH, Kim KA, et al. Microbiologic study of the bile culture and antimicrobial susceptibility in patients with biliary tract infection. Korean J Gastroenterol. 2008;51:248–54.
Li QW, Ji F. A clinical study of bile cultures and antibiotic susceptibility test in the patients with operation on biliary tract. Zhonghua Wai Ke Za Zhi. 2009;47:527–9.
Salvador VB, Lozada MC, Consunji RJ. Microbiology and antibiotic susceptibility of organisms in bile cultures from patients with and without cholangitis at an Asian academic medical center. Surg Infect (Larchmt). 2011;12:105–11. doi:10.1089/sur.2010.005.
Karpel E, Madej A, Buldak L, Dulawa-Buldak A, Nowakowska-Dulawa E, Labuzek K, et al. Bile bacterial flora and its in vitro resistance pattern in patients with acute cholangitis resulting from choledocholithiasis. Scand J Gastroenterol. 2011;46:925–30. doi:10.3109/00365521.2011.560676.
Flores C, Maguilnik I, Hadlich E, Goldani LZ. Microbiology of choledochal bile in patients with choledocholithiasis admitted to a tertiary hospital. J Gastroenterol Hepatol. 2003;18:333–6.
Sahu MK, Chacko A, Dutta AK, Prakash JA. Microbial profile and antibiotic sensitivity pattern in acute bacterial cholangitis. Indian J Gastroenterol. 2011;30:204–8. doi:10.1007/s12664-011-0135-3.
Rerknimitr R, Fogel EL, Kalayci C, Esber E, Lehman GA, Sherman S. Microbiology of bile in patients with cholangitis or cholestasis with and without plastic biliary endoprosthesis. Gastrointest Endosc. 2002;56:885–9. doi:10.1067/mge.2002.129604.
Nomura T, Shirai Y, Hatakeyama K. Bacteribilia and cholangitis after percutaneous transhepatic biliary drainage for malignant biliary obstruction. Dig Dis Sci. 1999;44:542–6.
Yu H, Guo Z, Xing W, Guo X, Liu F, Li B. Bile culture and susceptibility testing of malignant biliary obstruction via PTBD. Cardiovasc Intervent Radiol. 2012;35:1136–44. doi:10.1007/s00270-011-0263-2.
Englesbe MJ, Dawes LG. Resistant pathogens in biliary obstruction: importance of cultures to guide antibiotic therapy. HPB (Oxford). 2005;7:144–8. doi:10.1080/13651820510028792.
Nomura T, Shirai Y, Hatakeyama K. Enterococcal bactibilia in patients with malignant biliary obstruction. Dig Dis Sci. 2000;45:2183–6.
Bryan CS, Reynolds KL, Brown JJ. Mortality associated with enterococcal bacteremia. Surg Gynecol Obstet. 1985;160:557–61.
McBride SJ, Upton A, Roberts SA. Clinical characteristics and outcomes of patients with vancomycin-susceptible Enterococcus faecalis and Enterococcus faecium bacteraemia—a five-year retrospective review. Eur J Clin Microbiol Infect Dis. 2010;29:107–14. doi:10.1007/s10096-009-0830-5.
Caballero-Granado FJ, Becerril B, Cuberos L, Bernabeu M, Cisneros JM, Pachon J. Attributable mortality rate and duration of hospital stay associated with enterococcal bacteremia. Clin Infect Dis. 2001;32:587–94. doi:10.1086/318717.
Schaberg DR, Culver DH, Gaynes RP. Major trends in the microbial etiology of nosocomial infection. Am J Med. 1991;91:S72–5.
Bush LM, Calmon J, Cherney CL, Wendeler M, Pitsakis P, Poupard J, et al. High-level penicillin resistance among isolates of enterococci. Implications for treatment of enterococcal infections. Ann Intern Med. 1989;110:515–20.
Patterson JE, Zervos MJ. High-level gentamicin resistance in Enterococcus: microbiology, genetic basis, and epidemiology. Rev Infect Dis. 1990;12:644–52.
Rice LB. Emergence of vancomycin-resistant enterococci. Emerg Infect Dis. 2001;7:183–7.
DiazGranados CA, Zimmer SM, Klein M, Jernigan JA. Comparison of mortality associated with vancomycin-resistant and vancomycin-susceptible enterococcal bloodstream infections: a meta-analysis. Clin Infect Dis. 2005;41:327–33. doi:10.1086/430909.
Bhavnani SM, Drake JA, Forrest A, Deinhart JA, Jones RN, Biedenbach DJ, et al. A nationwide, multicenter, case-control study comparing risk factors, treatment, and outcome for vancomycin-resistant and -susceptible enterococcal bacteremia. Diagn Microbiol Infect Dis. 2000;36:145–58.
Thompson J, Bennion RS, Pitt HA. An analysis of infectious failures in acute cholangitis. HPB Surg. 1994;8:139–44. (discussion 45).
Yellin AE, Heseltine PN, Berne TV, Appleman MD, Gill MA, Riggio CE, et al. The role of Pseudomonas species in patients treated with ampicillin and sulbactam for gangrenous and perforated appendicitis. Surg Gynecol Obstet. 1985;161:303–7.
Walker AP, Nichols RL, Wilson RF, Bivens BA, Trunkey DD, Edmiston CE Jr, et al. Efficacy of a beta-lactamase inhibitor combination for serious intraabdominal infections. Ann Surg. 1993;217:115–21.
Cohn SM, Lipsett PA, Buchman TG, Cheadle WG, Milsom JW, O’Marro S, et al. Comparison of intravenous/oral ciprofloxacin plus metronidazole versus piperacillin/tazobactam in the treatment of complicated intraabdominal infections. Ann Surg. 2000;232:254–62.
Ohlin B, Cederberg A, Forssell H, Solhaug JH, Tveit E. Piperacillin/tazobactam compared with cefuroxime/metronidazole in the treatment of intra-abdominal infections. Eur J Surg. 1999;165:875–84. doi:10.1080/11024159950189393.
Sirinek KR, Levine BA. A randomized trial of ticarcillin and clavulanate versus gentamicin and clindamycin in patients with complicated appendicitis. Surg Gynecol Obstet. 1991;172:30–5.
Polk HC Jr, Fink MP, Laverdiere M, Wilson SE, Garber GE, Barie PS, et al. Prospective randomized study of piperacillin/tazobactam therapy of surgically treated intra-abdominal infection. The piperacillin/tazobactam intra-abdominal infection study group. Am Surg. 1993;59:598–605.
Solomkin JS, Mazuski JE, Baron EJ, Sawyer RG, Nathens AB, DiPiro JT, et al. Guidelines for the selection of anti-infective agents for complicated intra-abdominal infections. Clin Infect Dis. 2003;37:997–1005. doi:10.1086/378702.
Harbarth S, Uckay I. Are there patients with peritonitis who require empiric therapy for enterococcus? Eur J Clin Microbiol Infect Dis. 2004;23:73–7. doi:10.1007/s10096-003-1078-0.
Marne C, Pallares R, Martin R, Sitges-Serra A. Gangrenous cholecystitis and acute cholangitis associated with anaerobic bacteria in bile. Eur J Clin Microbiol. 1986;5:35–9.
van den Hazel SJ, Speelman P, Tytgat GN, Dankert J, van Leeuwen DJ. Role of antibiotics in the treatment and prevention of acute and recurrent cholangitis. Clin Infect Dis. 1994;19:279–86.
Gilbert DN, Moellering RC, Eliopoulis GM, Saag MS, Chambers HF. The Sanford guide to antimicrobial therapy 2011. 39th ed. Sperryville, VA: Antimicrobial Therapy Inc; 2011.
Negm AA, Schott A, Vonberg R-P, Weismueller TJ, Schneider AS, Kubicka S, et al. Routine bile collection for microbiological analysis during cholangiography and its impact on the management of cholangitis. Gastrointest Endosc. 2010;72:284–91. doi:10.1016/j.gie.2010.02.043.
Tanaka A, Takada T, Kawarada Y, Nimura Y, Yoshida M, Miura F, et al. Antimicrobial therapy for acute cholangitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg. 2007;14:59–67. doi:10.1007/s00534-006-1157-6.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kwon, W., Jang, JY., Kim, EC. et al. Changing trend in bile microbiology and antibiotic susceptibilities: over 12 years of experience. Infection 41, 93–102 (2013). https://doi.org/10.1007/s15010-012-0358-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-012-0358-y