Abstract
Excessive body weight negatively affects balance. Clinical examination provides insight into the physiopathology and etiology of balance disorders and functional scales can rate its severity. Instrumental evaluation can add further information and provide objective baseline and outcome measures for evidence-based rehabilitation programs. Static posturography focuses on the properties of the center of pressure trajectory using time series. Its utility in clinical practice is limited by absence of a definite normal pattern, lack of standardization in the measurement protocols, and large number of variables computed from the force platform. Recently, some advanced mathematical methods have been proposed to describe the biological signals (entropy and fractal dimension). The increased body mass produces anteroposterior instability in both genders and mediolateral destabilization in males. Proprioceptive exercises together with isometric strengthening of the ankle agonist and antagonist muscles, cardiorespiratory conditioning, and exercises aimed at improving perception of the body should be implemented in the rehabilitation program.
Similar content being viewed by others
Introduction
Postural stability and balance are defined as the ability to return the body close to equilibrium point when exposed to a perturbation and it represents a key function for performing daily life tasks. Aging and a number of pathologies often increase the amounts of postural sway, which may ultimately lead to falls [1]. Among the pathological conditions, obesity has a profound effect on disability and quality of life [2]. The excessive amount of fat modifies the body geometry by adding passive mass to different regions [3] and it influences the biomechanics of activities of daily living, causing functional limitations, and possibly predisposing to injury [4]. Quantitative evidence exists that excessive body weight negatively affects the movement from sitting to standing [5, 6], walking [3, 7–9] and balance [10•]. Adipose tissue accumulation and body mass increases can be a major factor contributing to the occurrence of falls, which explains why obese persons appear to be at greater risk than normal-weight subjects under daily postural stresses and perturbations [11].
Although fat mass could be considered a potential protective layer in falling, the additional weight of the fat mass itself yields some negative aspects. The consequences of falling in obese subjects are more critical with higher treatment costs and more specialized care required following orthopaedic surgery [11, 12]. Complications associated with falls (eg, fractures, muscle contractures, post-trauma injury) are often more difficult to treat in obese persons than in normal-weight individuals [13].
Balance Control
Clinical examination provides insight into the physiopathology and etiology of balance disorders and functional scales (Tinetti, Berg, Conley) can rate its severity and the related risk of fall. Instrumental evaluation can add further information and provide objective baseline and outcome measures for evidence-based rehabilitation programs. Among the available modalities, platform posturography is the most widely used [14]. In particular, static posturography has been extensively used in populations of various age to study the biomechanical effects on gross motor skills in subjects affected by various motor disorders (cerebral palsy, muscular dystrophy, spinal cord injuries), fine cognitive or learning disabilities (autism, developmental coordination disorder, attention deficit hyperactivity disorder, and dyslexia) [15], genetic disorders (Down syndrome, Prader-Willi syndrome [PWS]) [16, 17•], and obesity [10•].
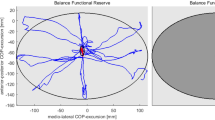
Platform stabilometry consists of the measurement of forces exerted against a platform during quiet stance. The force platform quantifies the body sways of an individual in a standing position. It is widely used in clinical settings to obtain functional markers on fine competencies and their development and a large number of posturographic measures are sensitive to testing condition (ie, eyes open vs eyes closed, feet position, and presence of external stimuli). Static posturography is user-friendly and typically in everyday practice focuses on the properties of the center of pressure (CoP) trajectory using time series (length, surface, maximal amplitude of the displacement, speed, and frequency analysis). Simplicity of the experimental protocols and safety of the individuals subject to the tests, especially in pathological conditions, are potentially advantages [18]. However, the information obtained is difficult to be univocally interpreted from a physiological point of view. The utility of static posturography in clinical practice is somehow limited for the following factors: 1) the absence of a definite normal pattern; 2) the lack of standardization in the measurement protocols; and 3) the large number of highly coupled variables that are computed from the force platform recordings [12]. From these limiting factors there is a need for reliable approaches to extract physiologically meaningful information from stabilograms [16, 17•, 18, 19].
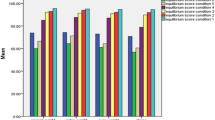
Recently, some advanced mathematical methods have been proposed to describe the patterns of biological signals [16, 20] applying a dynamic approach, in terms of entropy [18, 21] and fractal dimension (FD) analysis [19]. In particular, the latter can be used to quantify the complexity of a biological signal. As for the CoP trajectory, a change in FD may indicate a change in control strategies for maintaining quiet stance [19]. Previous studies [17•, 22–25] suggested that FD could represent a reliable method to assess balance control complementary to traditional analysis in time and frequency domain. Recently, Cimolin et al. [25] used the traditional method with time (the range of sway in anteroposterior (AP) and mediolateral (ML) direction and the total trajectory length) and frequency domain approaches and then integrated them with the FD approach to quantify balance control in genetically obese patients. While time domain analysis showed higher values of CoP excursion in both AP and ML direction with longer CoP trajectory compared to healthy controls, frequency analysis showed the same values as controls. As for the presence of higher oscillations in obese individuals with respect to controls, two hypotheses are proposed by literature: 1) the reduction of plantar sensitivity due to the hyperactivation of the plantar mechanoreceptors for the continuous pressure of supporting the large mass; and 2) the presence of high mechanical request in obese subjects due to a whole body center of mass further away from the axis of rotation causing a greater gravitational torque [26, 27]. Furthermore, the frequency analysis therefore seems to add information to the traditional one, analyzing the rate at which the CoP direction changes, reflecting the action-reaction times between external perturbations and compensatory movements to re-establish balance: the obese individuals present larger excursions of CoP, which are characterized by the same velocity of oscillation if compared to controls. These data suggest that time domain parameters are not completely satisfactory for the detection of early changes in standing balance: the dynamic characteristics of posture, characterized by chaotic fluctuation of CoP trajectories, are not detected. Frequency-domain characteristics and dynamical system theory can detect early changes and may be considered complementary to time frequency analysis for characterizing posture. Genetically obese patients were characterized by higher values of FD parameter, indicative of the complexity of the stabilometric pattern in postural maintenance. The higher FD values may be interpreted as an inability to synergically modulate the three systems (ie, visual, vestibular, and somatosensory) involved in maintaining posture. The human body is continuously exposed to external perturbations, which we try to counteract by integrating the real-time inputs and the prediction system based on previous inputs. On the other hand, a more complex stabilometric pattern could be also interpreted as a characteristic of a successful vigilant strategy to keep balance. Both interpretations can be correct but the question is then how to decide which one is the most appropriate one in a case at hand and the debate is still open. More work is needed to identify the correct physiological interpretation of DS parameter in a given condition.
There is now evidence that body weight is a strong predictor of postural instability [26], with obesity-associated postural perturbations appearing in adolescence [28]. In particular, obesity has been associated with greater forward displacement of the CoP during dynamic standing balance activities [29]. Excessive body weight affects posture linearly with the increase of body mass index (BMI) [30, 31], akin to what occurs in the later stages of pregnancy [32]: the center of gravity shifts forward, the lumbar lordosis increases together with the pelvic forward tilt, and the dorsal kyphosis and a secondary cervical lordosis become more pronounced [33, 34]. Frequently, internal rotation of the hips, knee valgism, and flat feet coexist. The feet tend to splay apart during standing to optimize the center of gravity and stability. This also occurs in the seated posture to facilitate trunk flexion and to reduce weight on the pelvis [31]. Discomfort and reduced tolerance of fixed postures are also consequences of a redundant mass. Pain has been shown to affect posture [33]. Reduced sensory integration has been hypothesized for the poor balance [34]. Reduced balance affects a variety of daily and occupational tasks, particularly those performed with the upper limbs from a standing posture [35]. Obesity would therefore appear to be linked to an increased risk of falling [3], while weight loss increases postural stability [36]. However, whether this is due to weight loss per se or to the beneficial effects of physical activity needs further investigation. Not only does BMI increase but also its fluctuations (eg, in eating disorders) show a correlation with reduced stability [36, 37]. High BMI values are coupled with increased bone density and a protective layer of fat around the joints. But still obese subjects are not protected against falls and older obese subjects in particular are at a high risk of falls and fractures [38, 39•].
Body mass distribution usually shows gender differences (gynoid and android shape), even if android fat distribution is also observed in females, particularly in postmenopausal women: thus, whether shape induces possible gender-specific consequences on balance is still controversial. Few dated studies on normal-weight persons reported no gender differences in sway area during standing and in perturbed conditions [40, 41], although elderly women appear to have poorer balance and functional performances [42]. In 2003, Gravante et al. [43] studied gender differences in obese and healthy subjects using a baropodometric platform. They reported no gender-related differences in foot pressure, foot contact surface, and CoP mean location. They also found that the CoP mean location was not influenced by weight. More recent studies have investigated obese male subjects. Hue et al. [26] reported the lower postural stability of obese men, assessed by the AP and ML coordinates of the CoP, than their lean counterparts, although other authors showed that postural stability improved in severely obese men after weight loss [3] and specific balance training [1]. The linear relationship between magnitude of the weight loss and improved balance provides additional support to the suggestion that body weight is an important predictor of postural stability [26]. A recent paper [44] has investigated gender differences in postural control as assessed by standardized functional tests (one-leg standing balance and walking performance) in 318 healthy normal-weight adults. The authors reported that women performed significantly poorer during the timed getup-and-go test and the tandem Romberg with eyes closed. These results were mainly influenced by the instability shown by middle-aged women.
The increased body mass seems to produce AP instability in both genders and ML destabilization only in males. Therefore, obesity seems to produce gender-specific: obese males, differently from females, show greater CoP displacements in the ML direction [10•]. Two possible hypotheses could explain our results, both related to the mass distribution. The fat mass is usually concentrated in the thorax-abdominal region in males (android shape), while it is usually around the hips and the upper portion of legs in females (gynoid shape) [45].
In both genders the increased body mass contributes to an increased ankle torque (AP destabilization), but the android shape involves a greater amount of mass/load over the hips, which could account for the increased ML CoP excursion. The second hypothesis, partially overlapping with the previous one, is related to the effect of a different mass distribution on the center of mass. This is defined as the imaginary point where we can assume the total body mass is concentrated and the stabilization of its spatial position has previously been proposed as the goal of postural responses [10•]. The mass distribution alters the center of mass position, which is higher in the android than in the gynoid shape. Furthermore, the fact that males are usually heavier than females should be taken into account. In summary, men have to cope with heavier body weights and higher center of mass, possibly leading to an increased loading/unloading mechanism in ML direction. The assumption of the different mass distribution in men and women is in accordance with the experimental data we found. However, such difference is merely a hypothesis because the experimental design of our study does not investigate the gender-shape association (eg, some women could have an android rather than gynoid shape). The inclusion of the waist-to-hip ratio measure in our study would have provided quantitative characterization of the subjects’ shape, thus ensuring the homogeneity of the groups. Whether the reported difference between males and females in CoP displacements is only shape-related still remains an open question. The potential differences related to shape and gender could be topics of future studies, which should consider the waist-to-hip ratio measure. Those studies might also provide insight on the potential correlations with CoP displacements.
From a clinical perspective, AP instability has been suggested to be related to the increased muscle activity [10•, 26]. Obese males and females like elderly fallers show an increased AP instability and an increased muscle activity during static posture [10•]. There is growing evidence that ML instability is an important posturographic marker of functional balance impairment [14, 29, 46, 47], and to our knowledge, the different behavior in ML direction observed across genders is a novel result.
Efficient lower limb muscles are the key to independent mobility, and strength of the flexor and extensor muscles is highly correlated with the capacity to execute daily tasks safely and maintain balance [48]. The relationship between strength and mobility tasks is curvilinear, suggesting that factors other than muscle function contribute to mobility—still muscle strength is considered the most important factor to enhance mobility [42, 49]. It has been shown that reduced muscle strength relative to body weight induces earlier fatigue of the quadriceps muscles in the obese that, in turn, reduces shock attenuation and increases the loading rate and variability at the knee during gait [34]. Quadriceps muscle strength is known to be an important factor governing the vibration dampening of the lower limb [50] and its weakness is known to be a risk factor for the development of knee osteoarthritis [51–56]. Lower rates of musculoskeletal loading have been found in strength-trained females when compared with sedentary females walking at similar speeds, suggesting that increased muscular strength may enhance shock attenuation [57].
Muscle strength in normal-weight, obese, and genetically obese populations appears to be clearly stratified [39•]. Subjects affected by genetic obesity, such as PWS, show the lowest absolute peak torque for knee flexor and extensor muscles. Reduced muscle tone, early childhood obesity, and impaired muscular trophic response could negatively interfere with muscular strength and coordination development, as well as with motor planning skills and account for the lowest absolute strength measured. On the other hand, it is not possible to exclude that the impairment of lower limb muscle function associated with PWS may be secondary to different mechanisms from those observed in patients with nonsyndromic obesity (eg, primary muscle pathology). The comparison of syndromal and nonsyndromal obese subjects suggests factors other than obesity per se seem to contribute to reduced muscular strength in PWS. Non-syndromal obese subjects produce greater absolute isokinetic torque than their lean counterpart [58, 59]. Absolute strength is higher in obese than normal-weight subjects possibly due to a higher absolute fat free mass rate correlated to BMI. It could therefore be hypothesized that obese patients retain a greater muscle mass in response to a greater loading, which could act as training stimulus. However, when data are normalized per body weight, obese subjects show significantly lower knee flexor and extensor strength compared to normal-weight subjects. Normalization per body weight instead of the more common normalization per fat-free mass can represent the load bearing on the muscles, which is in actual fact one of the major biomechanical constraints in obese subjects. Normalization per body weight may provide a realistic picture of the functional capacity of obese patients and may appropriately reflect the disabling degree of the motor limitation and represent a more meaningful indicator of physical capacity. In fact, it has been shown that muscle power, thus strength under dynamic conditions, normalized per body weight is reliably related with functional performance in obese patients [39•]. One of the prerequisites for balance control is the ability to generate adequate muscle force to maintain stability while moving. If the ankle joint stabilizers are relatively insufficient we might expect an increase in postural sway.
Significant weight loss or excessive gain has been shown to induce musculoskeletal adaptations that may induce postural and motor alterations [60]. Neuromuscular abnormalities have been described in 45 % of patients, muscle weakness in 43 %, and peripheral neuropathies in 13 % [61]. Peripheral neuropathy, probably secondary to chronic malnutrition and thiamine deficiency [62, 63], and localized compression neuropathies are notable complications of anorexia nervosa. Type 2 fiber atrophy with no evidence of neuropathic changes has also been noticed [64]. Such neuromuscular adaptations may ultimately cause postural and motor alterations. Postural control is a complex task performed by the integration of somatosensorial inputs processed in the nervous cerebral system and a reflex or voluntary response. Its aim is to maintain the body’s center of mass within the base of support during quiet upright stance. Impaired postural control may be secondary not only to sensorial damage such as visual [65], vestibular [66], and somatosensorial inputs [67], but also to central nervous system disorders [68, 69] and psychopathological problems [70]. Emotional factors, in particular anxiety, whose prevalence is particularly high in eating disorders [71–74], have been shown to negatively influence the efficiency of human postural control [75]. Anxiety appears to influence the interactions of visual with vestibular and somatosensory inputs, thus affecting the net performance of postural control [76]. There is some evidence that compulsive habits such as smoking causes more unstable posturographic results than nonsmoking [77] and that excessive body weight seems to affect the ability to withstand balance perturbations [78]. A few studies have utilized loading healthy subjects with extra weight, which imposed a relative weakness of the muscles that swing the leg, impaired the position control ,and increased the body sway areas, both with and without available vision [79, 80].
Balance Recovery
All obese individuals may experience decreased quality of life because excess body fat can interfere with daily activities of physical functioning, such as walking, bending, stooping, and kneeling [81]. Lessened ability to perform these physical tasks may lead to dependency on others for assistance with daily household chores [82], and, ultimately, to a sense of inadequacy or failure. Obese individuals are typically sedentary as there is an inverse relationship between BMI and activity levels [83]. An increase in BMI is not only negatively associated with physical activity levels, but it is also associated with an increase in functional impairment [84], which could lead to impaired balance and an increased risk of falls. Consequently, obese individuals may fear falling, which may lead to further reductions in physical activity [83], greater functional impairment [85], and greater risk of falling [17•]. Whether physical activity and training could represent the key solutions for counteracting balance problems in obese individuals need to be further demonstrated.
However, it appears from the considerations above that specific physical activity and rehabilitation exercises, also because they induce weight loss, may serve to disrupt the vicious circle of inactivity and relative muscle weakness and improve balance capacity and enhance confidence while performing daily tasks in obese subjects. The modality of supervised exercise classes is known to be the most effective way of prescribing adequate and safe physical activity. However, they can reach only small figures [86•]. Partially supervised, home-based or mixed training programs could potentially have a greater impact and be more accessible to the general population. Providing an effective and simple home-based training would represent a continuum of the rehabilitation process outside the hospital, which appears crucial in all chronic conditions. Low-intensity long-term training is feasible in the obese and even genetically obese populations and can enhance overall function, including gait and balance, more than muscle function. Training sessions should be kept simple and reasonably short to guarantee compliance to the program. The exercises prescribed need to be clearly explained and they should not exceed a total of 30 minutes per day. Also, patients should first be familiarized with the exercises and supervised for 2 weeks to make sure they would be able to perform them properly at home in the following period. It is very important that training addresses the muscle groups that are mainly responsible for balance capacity, specifically the ankle stabilizers that can increase peak ankle power. At this level push-off capacity is lower than normal-weight subjects [87]. After 6-month home training PWS individuals have been shown to improve significantly in cadence and in ankle plantar and dorsal flexor isokinetic strength [86•].
Improvement in spatiotemporal parameters has a positive impact on performing activities of daily life and is decisive for determining compliance in a weight-loss program. Rehabilitation programs should take such findings into account on a larger scale. It has been documented that obese patients benefit from specific posture programs designed to improve balance and strength [10•], and that weight reduction has a favorable impact on posture instability [33]. Therefore, not only weight loss but strengthening of ankle flexors/extensors, and balance training should be implemented as part of comprehensive rehabilitation programs [34].
A recent paper argues against the suggestion that physical activity is the key factor explaining balance control deficits [27]. In this study, sway from heavy and trained individuals (American football players) was compared to that of sedentary obese subjects matched for BMI and lean individuals. Their results showed no differences in sways between footballers and obese individuals, with these two groups swaying more than lean individuals. Weight loss per se may well represent the key factor, because it reduces body mass and pressure on the muscular system, or because it allows plantar mechanoreceptors to work within a more normal range of sensitivity. Therefore, the issue of whether training and physical activity or rather weight loss can represent the key factors to counteract balance control problems related to obesity needs further scientific evidence.
Quantification of their high CoP displacement in the AP and the ML directions strongly supports the issue that these patients need tailored rehabilitation programs. Particularly, those aimed at improving ML control using hip strategies should be given consideration. The inclusion of proprioceptive exercises in the comprehensive rehabilitation program appears important, together with isometric strengthening of the ankle agonist and antagonist muscles, cardiorespiratory conditioning, and exercises aimed at improving perception of the body. Activity programs including resistance training, stretching, and an increase in balance confidence have already been shown to decrease the fear of falling and thus have a positive impact on the elderly [84, 88, 89]. In the future, larger studies should address the issue of whether balance training in obese subjects could be equally effective.
Conclusions
As the prevalence of obesity is increasing at an alarming rate worldwide, obesity-related disabilities will eventually become a serious threat to national health systems. Among several disabling conditions, an increase in BMI is associated with an increase in functional impairment, impaired balance, and an increased risk of falls. Complications associated with falls are often more difficult to treat in obese persons than in normal-weight individuals. Although further conclusive research is needed, some evidence has been provided that targeted physical activity and rehabilitation exercises could play an important role in improving balance capacity. Based on recent initial findings, partially supervised, home-based, or mixed training programs could have a significant impact in reducing risk of falls in this population. Whether regular program of exercises or rather weight loss can represent the prime solution to counteract the obesity-related reduced balance is still debated. However, training programs inducing weight loss appear to be beneficial, even if this effect may tap at other processes (eg, fear of falling). More studies are needed to assess effectiveness of balance training and weight loss programs in the long term in wider populations of obese subjects.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Maffiuletti NA, Agosti F, Proietti M, Riva D, Resnik M, Lafortuna CL, Sartorio A. Postural instability of extremely obese individuals improves after a body weight reduction program entailing specific balance training. J Endocrinol Invest. 2005;28:2–7.
Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004;89:2583–9.
de Souza SA, Faintuch J, Valezi AC, et al. Gait cinematic analysis in morbidly obese patients. Obes Surg. 2005;15:1238–42.
Wearing SC, Hennig EM, Byrne NM, Steele JR, Hills AP. The biomechanics of restricted movement in adult obesity. Obes Rev. 2006;7:13–24.
Sibella F, Galli M, Romei M, Montesano A, Crivellini M. Biomechanical analysis of sit-to-stand movement in normal and obese subjects. Clin Biomech. 2003;18:745–50.
Galli M, Crivellini M, Sibella F, et al. Sit-to-stand movement analysis in obese subjects. Int J Obes. 2000;24:1488–92.
Saibene F, Minetti AE. Biomechanical and physiological aspects of legged locomotion in humans. Eur J Appl Physiol. 2003;88:297–316.
Spyropoulos P, Pisciotta JC, Pavlou KN, Cairns MA, Simon SR. Biomechanical gait analysis in obese men. Arch Phys Med Rehabil. 1991;72:1065–70.
Vismara L, Romei M, Galli M, et al. Clinical implications of gait analysis in the rehabilitation of adult patients with “Prader-Willi” Syndrome: a crosssectional comparative study (“Prader-Willi” Syndrome vs matched obese patients and healthy subjects). J Neuroengineering Rehabil. 2007;4:14.
• Menegoni F, Galli M, Tacchini E, Vismara L, Cavigioli M, Capodaglio P. Gender-specific effect of obesity on balance. Obesity. 2009;17(10):1951–6. This study quantifies balance capacity with stabilogram in obese subjects and explains gender differences providing insight in balance control mechanisms and spinoffs for rehabilitation.
Finkelstein EA, Chen H, Prabhu M, Trogdon JG, Corso PS. The relationship between obesity and injuries among U.S. adults. Am J Health Promot. 2007;21:460–8.
Kim Y, Morshed S, Joseph T, Bozic K, Ries MD. Clinical impact of obesity on stability following revision total hip arthroplasty. Clin Orthop Relat Res. 2006;453:142–6.
Jiganti JJ, Goldstein WM, Williams CS. A comparison of the perioperative morbidity in total joint arthroplasty in the obese and nonobese patient. Clin Orthop Relat Res. 1993;289:175–9.
Chiari L, Rocchi L, Cappello A. Stabilometric parameters are affected by anthropometry and foot placement. Clin Biomech (Bristol, Avon). 2002;17:666–77.
Schmid M, Conforto S, Lopez L, Renzi P, D’Alessio T. The development of postural strategies in children: a factorial design study. J Neuroeng Rehabil. 2005;30(2):29.
Galli M, Rigoldi C, Mainardi L, Tenore N, Onorati P, Albertini G. Postural control in patients with down syndrome. Disabil Rehabil. 2008;30:1274–8.
• Capodaglio P, Menegoni F, Vismara L, Cimolin V, Grugni G, Galli M. Characterisation of balance capacity in Prader-Willi patients. Res Dev Disabil. 2011;32(1):81–6. This study provides evidence of reduced balance capacity in genetically obese as compared to nonsyndromal obese subjects.
Sabatini AM. Analysis of postural sway using entropy measures of signal complexity. Med Biol Eng Comput. 2000;38(6):617–24.
Doyle TL, Newton RU, Burnett AF. Reliability of traditional and fractal dimension measures of quiet stance center of pressure in young, healthy people. Arch Phys Med Rehabil. 2005;86:2034–40.
Manabe Y, Honda E, Shiro Y, et al. Fractal dimension analysis of static stabilometry in Parkinson’s disease and spinocerebellar ataxia. Neurol Res. 2001;23:397–404.
Myklebust JB, Prieto T, Myklebust B. Evaluation of nonlinear dynamics in postural steadiness time series. Ann Biomed Eng. 1995;23(6):711–9.
Peng CK, Hausdorff JM, Goldberger AL. Fractal mechanisms in neural control: human heartbeat and gait dynamics in health and disease. In: Walleczek J, editor. Nonlinear dynamics, self-organization, and biomedicine. Cambridge: Cambridge Univ Pr; 2000.
Pincus SM. Approximate entropy as a measure of system complexity. Proc Natl Acad Sci USA. 1991;88:2297–301.
Blaszczky JW, Klonowsky W. Postural stability and fractal dynamics. Acta Neuro Exp. 2001;61:105–12.
Cimolin V, Galli M, Rigoldi C, Grugni G, Vismara L, Mainardi L, Capodaglio P. Fractal dimension approach in postural control of subjects with Prader-Willi Syndrome. J Neuroeng Rehabil. 2011;8:45.
Hue O, Simoneau M, Marcotte J, Berrigan F, Doré J, Marceau P, Marceau S, Tremblay A, Teasdale N. Body weight is a strong predictor of postural stability. Gait Posture. 2007;26:32–8.
Handrigan GA, Berrigan F, Hue O, Simoneau M, Corbeil P, Tremblay A, Teasdale N. The effects of muscle strength on center of pressure-based measures of postural sway in obese and heavy athletic individuals. Gait Posture. 2012;35(1):88–91.
McGraw B, McClenaghan BA, Williams HG, Dickerson J, Ward DS. Gait and postural stability in obese and nonobese prepubertal boys. Arch Phys Med Rehabil. 2000;81:484–9.
Berrigan F, Simoneau M, Tremblay A, Hue O, Teasdale N. Influence of obesity on accurate and rapid arm movement performed from a standing posture. Int J Obes (Lond). 2006;30:1750–7.
Gilleard W, Smith T. Effect of obesity on posture and hip joint moments during a standing task, and trunk forward flexion motion. Int J Obes (Lond). 2007;31(2):267–71.
Corbeil P, Simoneau M, Rancourt D, Tremblay A, Teasdale N. Increased risk for falling associated with obesity: mathematical modeling of postural control. IEEE Trans Neural Syst Rehabil Eng. 2001;9(2):126–36.
Teasdale N, Hue O, Marcotte J, Berrigan F, Simoneau M, Doré J, et al. Reducing weight increases postural stability in obese and morbid obese men. Int J Obes (Lond). 2007;31(1):153–60.
Rodacki AL, Fowler NE, Provensi CL, Rodacki C de L, Dezan VH. Body mass as a factor in stature change. Clin Biomech (Bristol, Avon) 2005;20(8):799–805.
Syed IY, Davis BL. Obesity and osteoarthritis of the knee: hypotheses concerning the relationship between ground reaction forces and quadriceps fatigue in long-duration walking. Med Hypotheses. 2000;54:182–5.
Chau N, Gauchard GC, Siegfried C, Benamghar L, Dangelzer JL, Français M, et al. Relationships of job, age, and life conditions with the causes and severity of occupational injuries in construction workers. Int Arch Occup Environ Health. 2004;77(1):60–6.
Fontana MP, Menegoni F, Vismara L, Galli M, Romei M, Bergamini E, et al. Balance in patients with anorexia and bulimia nervosa. Eur J Phys Rehabil Med. 2009;45(3):335–40.
Tinetti ME. Clinical practice preventing falls in elderly persons. N Engl J Med. 2003;348:42–9.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–7.
• Capodaglio P, Vismara L, Menegoni F, Baccalaro G, Galli M, Grugni G. Strength characterization of knee flexor and extensor muscles in Prader-Willi and obese patients. BMC Musculoskelet Disord. 2009;10:47. This paper objectively quantifies muscle function and strength in genetically and non-genetically obese subjects.
Maki BE, McIlroy WE, Perry SD. Influence of lateral destabilization on compensatory stepping responses. J Biomech. 1996;29:343–53.
Wolfson L, Whipple R, Derby CA, Amerman P, Nashner L. Gender differences in the balance of healthy elderly as demonstrated by dynamic posturography. J Gerontol. 1994;49:M160–7.
Capodaglio P, Capodaglio EM, Facioli M, Saibene F. Long-term strength training for community-dwelling people over 75: impact on muscle function, functional ability and life style. Eur J Appl Physiol. 2007;100:535–42.
Gravante G, Russo G, Pomara F, Ridola C. Comparison of ground reaction forces between obese and control young adults during quiet standing on a baropodometric platform. Clin Biomech (Bristol, Avon). 2003;18:780–2.
Vereeck L, Wuyts F, Truijen S, Van de Heyning P. Clinical assessment of balance: normative data, and gender and age effects. Int J Audiol. 2008;47:67–75.
Clark KN. Balance and strength training for obese individuals. ACSM’S Health Fitness J. 2004;8:14–20.
Laughton CA, Slavin M, Katdare K, et al. Aging, muscle activity, and balance control: physiologic changes associated with balance impairment. Gait Posture. 2003;18:101–8.
Blaszczyk JW, Orawiec R, Duda-Klodowska D, Opala G. Assessment of postural instability in patients with Parkinson’s disease. Exp Brain Res. 2007;183:107–14.
Ferrucci L, Guralnik JM, Buchner D, et al. Departures from linearity in the relationship between measures of muscular strength and physical performance of the lower extremities: the women’s health and ageing study. J Gerontol A Biol Sci Med Sci. 1997;52(5):M275–85.
Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? Am J Prev Med. 2003;25(3 Suppl 2):129–36.
Wakeling JM, Liphardt AM, Nigg BM. Muscle activity reduces soft tissue resonance at heel-strike during walking. J Biomech. 2003;36:1761–9.
Slemenda C, Brandt KD. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997;127:97–104.
Slemenda C, Heilman DK, Brandt KD, Katz BP, Mazzuca SA, Braunstein EM, Byrd D. Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis in women? Arthritis Rheum. 1998;41:1951–59.
Baker KR, Xu L, Zhang Y, Nevitt M, Niu J, Aliabadi P, Yu W, Felson D. Quadriceps weakness and its relationship to tibio-femoral and patella-femoral knee osteoarthritis in Chinese: the Beijing osteoarthritis study. Arthritis Rheum. 2004;50:1815–21.
Hortobagyi T, Garry J, Holbert D, Devita P. Aberrations in the control of quadriceps muscle force in patients with knee osteoarthritis. Arthritis Rheum. 2004;51:562–9.
Becker R, Berth A, Nehring M, Awiszus F. Neuromuscular quadriceps dysfunction prior to osteoarthritis of the knee. J Orthop Res. 2004;22:768–73.
Thorstensson CA, Petersson IF, Jacobsson LT, Boegard TL, Roos EM. Reduced functional performance in the lower extremity predicted radiographic knee osteoarthritis five years later. Ann Rheum Dis. 2004;63:402–7.
Mikesky AE, Meyer A, Thompson KL. Relationship between quadriceps strength and rate of loading during gait in women. J Orthop Res. 2000;18:171–5.
Lafortuna CL, Maffiuletti NA, Agosti F, Sartorio A. Gender variations of body composition, muscle strength and power output in morbid obesity. Int J Obes. 2005;29:833–41.
Lafortuna CL, Agosti F, Marinone PG, Marazzi N, Sartorio A. The relationship between body composition and muscle power output in men and women with obesity. J Endocrinol Invest. 2004;27:854–61.
Smith FM, Latchford G, Hall RM, Millner PA, Dickson RA. Indications of disordered eating behaviour in adolescent patients with idiopathic scoliosis. J Bone Joint Surg Br. 2002;84:392–4.
Patchell RA, Fellows HA, Humpries LL. Neurologic complications of anorexia nervosa. Acta Neurol Scand. 1994;89:111–6.
Winston AP, Jamieson CP, Madira W, Gatward NM, Palmer RL. Prevalence of thiamin deficiency in anorexia nervosa. Int J Eat Disord. 2000;28:451–4.
Thaisetthawaktul P, Collazo-Clavell ML, Sarr MG, Norell JE, Dyck PJ. A controlled study of peripheral neuropathy after bariatric surgery. Neurology. 2004;63:1462–70.
McLoughlin DM, Spargo E, Wassif WS, Newham DJ, Peters TJ, Lantos PL, Russell GF. Structural and functional changes in skeletal muscle in anorexia nervosa. Acta Neuropathol. 1998;95:632–40.
Zabjek KF, Leroux MA, Coillard C, Rivard CH, Prince F. Evaluation of segmental postural characteristics during quiet standing in control and Idiopathic Scoliosis patients. Clin Biomech. 2005;20:483–90.
Rondot P, Odier F, Valade D. Postural disturbances due to homonymous hemianopic visual ataxia. Brain. 1992;115:178–88.
Black FO, Shupert FB, Nashner LM. Abnormal postural control associated with peripheral vestibular disorders. In: Pompeiano O, Allum JHJ, editors. Vestibulospinal control of posture and locomotion. Amsterdam: Elsevier; 1988.
Diener HC, Dichgans J, Guschlauber B, Man H. The significance of proprioception on postural stabilization as assessed by ischemia. Brain Res. 1984;296:103–9.
Hood JD. Unsteadiness of cerebellar origin: an investigation into the cause. J Laryngol Otol. 1980;9:865–76.
Karnath HO, Ferber S, Dichgans J. The neural representation of postural control in humans. Proc Natl Acad Sci. 2000;97:13931–6.
Wada M, Sunaga N, Nagai M. Anxiety affects the postural sway of the anterior-posterior axis in college students. Neurosci Lett. 2001;302:157–9.
Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry. 2004;161:2215–21.
Brewerton TD, Lydiard RB, Herzog DB, Brotman A, O’Neil P, Ballenger JC. Comorbidity of axis I psychiatric disorders in bulimia nervosa. J Clin Psychiatry. 1995;56:77–80.
Bulik CM. Anxiety, depression and eating disorders. In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity. 2nd ed. New York: The Guildford Press; 2002.
Deep AL, Nagy LM, Weltzin TE, Rao R, Kaye WH. Premorbid onset of psychopathology in long term recovered anorexia nervosa. Int J Eat Disord. 1995;17:291–7.
Galeazzi GM, Monzani D, Gherpelli C, Covezzi R, Guaraldi GP. Posturographic stabilization of healthy subjects exposed to full-lenght mirror image is inversely related to body-image preoccupations. Neurosci Lett. 2006;410:71–5.
Iki M, Ishizaki H, Aalto H, Starck J, Pyykkö I. Smoking habits and postural stability. Am J Otolaryngol. 1994;15:124–8.
Ledin T, Fransson PA, Magnusson M. Effects of postural disturbances with fatigued triceps surae muscles or with 20 % additional body weight. Gait Posture. 2004;19:184–93.
Eke-Okoro S, Larsson L, Sandlund B. Simulation of paretic gait in normal subjects by loading the ankles. Scand J Rehabil Med. 1985;17:147–50.
Odenrick P, Tropp H, Larsson L, Örtengren R. The effect of load in postural control at upright stance. In: Proceedings of applications of biomechanics. Bjärka-Säby, Sweden; 1985.
Han TS, Tijhuis MA, Lean ME, Seidell JC. Quality of life in relation to overweight and body fat distribution. Am J Public Health. 1998;88(12):1814–20.
Jensen GL, Rogers J. Obesity in older persons. J Am Diet Assoc. 1998;98(11):1308–11.
Bruce DG, Devine A, Prince RL. Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc. 2002;50(1):84–9.
Brouwer BJ, Walker C, Rydahl SJ, Culham EG. Reducing fear of falling in seniors through education and activity programs: a randomized trial. J Am Geriatr Soc. 2003;51(6):829–34.
Wearing SC, Hennig EM, Byrne NM, Steele JR, Hills AP. Musculoskeletal disorders associated with obesity: a biomechanical perspective. Obes Rev. 2006;7(3):239–50.
• Vismara L, Cimolin V, Grugni G, Galli M, Parisio C, Sibilia O, Capodaglio P. Effectiveness of a 6-month home-based training program in Prader-Willi patients. Res Dev Disabil. 2010;31(6):1373–9. This is the only paper objectively showing that home-based rehabilitation programs are feasible and effective in genetically obese patients.
Cimolin V, Galli M, Grugni G, Vismara L, Albertini G, Rigoldi C, Capodaglio P. Gait patterns in Prader-Willi and Down syndrome patients. J Neuroeng Rehabil. 2010;7:28.
Hatch J, Gill-Body KM, Portney LG. Determinants of balance confidence in community-dwelling elderly people. Phys Ther. 2003;83(12):1072–9.
Fuzhong L, McAuley E, Fisher KJ, Harmer P, Chaumeton N, Wilson NL. Self-efficacy as a mediator between fear of falling and functional ability in the elderly. J Aging Health. 2002;14(4):452–66.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Capodaglio, P., Cimolin, V., Tacchini, E. et al. Balance Control and Balance Recovery in Obesity. Curr Obes Rep 1, 166–173 (2012). https://doi.org/10.1007/s13679-012-0018-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-012-0018-7