Abstract
Preeclampsia is a disease of the placenta that results in widespread, multisystem, maternal vascular endothelial dysfunction and microangiopathy. It is multisystem disease that is clinically defined by new onset hypertension and proteinuria, typically presenting after 20 weeks of gestation. This nonspecific presentation often overlaps with other diseases. As such, the diagnosis remains challenging and relies on careful clinical assessment. The disease pathogenesis is complex, but is currently better understood. Despite novel research advances in understanding the pathogenesis of preeclampsia, to date there is no single diagnostic test available. However, meticulous antepartum care with careful assessment of preexisting maternal risk factors, understanding of the disease pathogenesis and recognition of the clinical manifestations will increase the likelihood of timely diagnosis and institution of appropriate interventions that can positively impact maternal and fetal outcomes.
Similar content being viewed by others
Introduction
Preeclampsia complicates approximately 5–7% of all pregnancies worldwide and remains one of the largest single causes of maternal and fetal morbidity and mortality. It is a disease of the placenta that results in widespread, multisystem, maternal vascular endothelial dysfunction and microangiopathy. It is clinically characterized by new onset hypertension, proteinuria, and a decreased glomerular filtration rate (GFR), typically presenting after 20 weeks of gestation. Progression of preeclampsia may lead to other systemic complications, including the HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets), neurologic involvement (eclampsia), as well as cardiac and renal failure. Fetal complications include oligohydramnios, intrauterine growth restriction, preterm delivery, and stillbirth. Treatment of preeclampsia is delivery of the placenta and, consequently, the fetus. Thus, the correct diagnosis is critical because timing delivery often requires balancing disease severity with the potential for fetal viability and well-being.
At present, there is no specific diagnostic test for the identification of preeclampsia and physicians must rely on careful clinical acumen to make the correct diagnosis. Numerous risk factors for the development of preeclampsia have been described to assist clinicians in the identification of at-risk populations, and novel insights into the pathogenesis of preeclampsia will provide future early diagnostic opportunities. In this manuscript, we review the risk factors for developing placental disease as well as the pathogenesis of the disease as it relates to the clinical syndrome. An approach to early diagnosis and standardized follow-up is discussed.
Risk Factors
The early diagnosis of preeclampsia is facilitated by knowledge of potential risk factors for inadequate placentation. Furthermore, identification of women at risk for preeclampsia before conception allows for medical optimization, early initiation of preventive measures, as well as enhanced surveillance for untoward maternal and fetal outcomes. To date, multiple risk factors for the development of preeclampsia have been reported in the literature (Table 1). These include a genetic predisposition, nulliparity and prolonged inter-birth interval, advancing maternal age as well as number of preexisting medical conditions, such as infertility necessitating in vitro fertilization (IVF), obesity, chronic renal disease, diabetes mellitus, hypertension and possibly thrombophilias [1–3]. In addition, conditions associated with either increased or abnormal placental mass are associated with increased rates of preeclampsia, such as multiple gestations resulting from assisted reproductive technologies and molar pregnancies [4–6].
A family history of preeclampsia, especially in first-degree relatives, either on the maternal or paternal side, increases the risk for preeclampsia, suggesting a genetic contribution in the formation of an abnormal placenta [7, 8]. Women with a previous history of preeclampsia have been documented to have a sevenfold increased risk of developing it again in a subsequent pregnancy (relative risk (RR) 7.19; 95% confidence interval (CI) 5.85–8.83) [1]. Furthermore, the severity and timing of onset affect the risk of recurrence; severe, early onset preeclampsia is associated with a 25–65% risk of recurrence compared with a 5–7% risk of recurrence in milder, late onset disease [9–11]. Even a family history of coronary artery disease is predictive for the development of preeclampsia [12], illustrating the link between poor placentation and vascular disease.
Classically, the first pregnancy (nulliparity) was considered to be one of the predisposing factors for developing preeclampsia, suggesting that exposure to a new antigen may be involved in the pathogenesis of preeclampsia. Similarly, a new partner, even with a history of multiparity, was stated to be associated with an increased risk of preeclampsia [13]. Surprisingly, recent evidence from an international population-based study demonstrated the rate of nulliparity did not correlate with the rate of preeclampsia [14]. In a Norwegian population study, the association between the risk for preeclampsia and the interval between pregnancies, 10 years or more, was more significant than the association between the risk and change of partner [15]. As such, advancing maternal age may be a significant confounder in many of these studies that propose the theory of exposure to a novel antigen. Still prior miscarriages with the same partner have been shown to be protective [12], whereas donor gametes have been linked to increased rates of preeclampsia [16], supporting the notion that exposure to a novel antigen may factor into the disease pathogenesis.
Extremes of maternal age have been suggested to place women at risk. However, in one study, younger women (age less than 20 years) were not found to be at increased risk for developing preeclampsia, whereas women older than 40 years of age had approximately twice the risk [1]. Whether older age itself affects ones ability to form a healthy placenta or whether older women simply tend to have other comorbidities, such as pregestational diabetes (RR 3.56; 95% CI 2.54–4.99), hypertension (RR 1.38; 95% CI 1.01–1.87), increased body mass index (RR 2.47; 95% CI 1.66–3.67), or higher rates of infertility that place them at increased risk is still unclear [1, 12]. Irrespective, an aging demographic with more women attempting conception even in the presence of significant comorbidities, and often utilizing reproductive assistance, necessitates careful pre-pregnancy assessment and perinatal follow-up in a growing population of mothers.
Pathogenesis
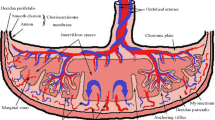
In normal pregnancy, the process of placentation begins when blastocysts adhere to the uterine endometrium forming a lineage of epithelial cells termed the invasive extravillous cytotrophoblast, which invades the uterine wall to create the decidua, transforming the spiral arteries into a low resistance uteroplacental circulation. There are likely multiple factors—genetic, environmental, immunological, etc.—that contribute to abnormal placentation, and the resulting “decidual vasculopathy,” wherein small, poorly developed spiral arteries result in compromised blood flow to the maternal-fetal interface [17, 18]. As the pregnancy progresses and the fetus outgrows the placental reserve, placental ischemia and infarction result in the “maternal placental syndrome”: preeclampsia, placental abruption and infarction, and/or ensuing adverse perinatal outcomes, including fetal growth restriction and stillbirth. As such, preeclampsia is a disease of the placenta that has its origins in the first trimester of pregnancy.
Underlying the link between impaired placentation and the clinical syndrome of preeclampsia is the endothelial cell. The profound assault to the maternal endothelium that results from placental ischemia is now understood to be due to the release of soluble factors from an ischemic placenta (Fig. 1). Vascular integrity throughout the body is maintained by vascular endothelial growth factors (VEGF) and, in pregnancy, placental growth factor PlGF. Both VEGF and PlGF circulate in high concentrations during normal pregnancy and are known to induce the synthesis of vasodilators, such as nitric oxide and prostacyclin in endothelial cells, decreasing vascular tone and blood pressure. A splice variant of the VEGF receptor Flt-1 produces soluble Flt-1 (sFlt-1), which binds with vascular endothelial growth factor (VEGF) and placental growth factor (PlGF), preventing their interaction with receptors located on the vascular endothelial cells [19]. A second soluble factor (sEng) is produced when the angiogenic receptor endoglin is proteolytically cleaved [20]. Endoglin, typically expressed on the surface of placental syncytio trophoblast layer and endothelial cells, acts as a coreceptor for the pro-angiogenic TGF-β. Thus, sEng deleteriously affects vascular tone by blocking the activation of endothelial nitric oxide synthase [20].
Pathogenesis of Preeclampsia. Placental ischemia results in the release of antiangiogenic factors (sFtl-1 and sEng), which bind to vascular endothelial growth factor (VEGF) and placental growth factor (PlGF), preventing their interaction with their native high affinity kinase receptors on the vascular endothelium. The resultant endothelial dysfunction presents as the clinical syndrome of preeclampsia
Assessment of these factors in a variety of clinical scenarios has provided insights with respect to some of the aforementioned at-risk populations. For example, maternal serum concentrations of sFlt-1 have been documented to be approximately two times higher than those measured in singleton pregnancies correlating well with placental weight, suggesting that the increased risk for preeclampsia in multiple gestations may be related to increased placental mass [21]. Larger placentas also have been noted in pregnancies conceived with assisted reproductive technologies [6]. Semiquantitative immunohistochemical staining of placental tissue in both molar pregnancies and pregnancies complicated by Trisomy 13 revealed increased sFlt-1 expression compared with control placental tissue [4, 22]. The increased risk of preeclampsia among women carrying trisomy 13 fetuses is not surprising because the gene for sFlt-1 also is located on chromosome 13 [23].
In women with chronic medical conditions, overproduction of the antiangiogenic factors may be less important with respect to the pathogenesis of preeclampsia. Instead an already compromised endothelium likely contributes to the noted increased rates of the clinical syndrome in women with medical comorbidities. Chronic kidney disease, for example, is a risk factor for the development of preeclampsia; and of all renal diseases, diabetic nephropathy confers the highest risk for pregnancy complications and renal compromise. A reverse transcription/polymerase chain reaction assessment of glomerular and tubular VEGF expression in patients with type II diabetes revealed progressive decline in VEGF expression with more severe glomerular and tubulointerstitial disease [24]. Thus, one can easily conceptualize based on such data why women with diabetic nephropathy are at a substantially increased risk for the development of preeclampsia. Further studies of at-risk populations with medical comorbidities will further assist with the understanding of the pathogenesis of preeclampsia.
Clinical Syndrome
As mentioned, preeclampsia is characterized by maternal multisystem vascular endothelial dysfunction and microangiopathy. It is defined by established criteria from the American College of Obstetrics and Gynecology (ACOG) as a systolic blood pressure of 140 mmHg or diastolic blood pressure of 90 mmHg along with new-onset proteinuria occurring after 20 weeks of gestation [25]. Proteinuria is defined as >300 mg per day in a 24-hour urine specimen, persistent +2 protein on dipstick testing, or a random protein to creatinine ratio >30 mg per mmol. Although renal involvement characterizes the syndrome (hypertension, proteinuria, and reduced glomerular filtration rate [GFR]), involvement of the liver (HELLP syndrome) and the brain (eclampsia) along with cardiac dysfunction may complicate severe cases. Novel understanding with respect to the balance between angiogenic and antiangiogenic factors has led to a more complete understanding of the clinical picture.
Hypertension
Maternal vascular accommodation to normal pregnancy begins shortly after conception with the formation of the low-resistance placental circulation. By week 6 of gestation, maternal systemic vascular resistance falls significantly while cardiac output increases [26]. The net effect of the low-resistance placental circulation and systemic vasodilatation, despite the increase in cardiac output, is a fall in mean arterial pressure [26, 27]. Although the exact mechanisms responsible for the systemic vasodilation that accompanies healthy pregnancy are not entirely clear, an intricate interplay of vasodilator and vasoconstrictive hormones, such as relaxin, nitric oxide, and alterations to the renin angiotensin system (RAS), are likely key contributors.
The hypertension associated with preeclampsia, however, also can certainly be explained by the presence of soluble antiangiogenic factors, as presumably the vascular endothelial injury secondary to the antiangiogenic factors reduces the synthesis of vasodilatory molecules while increasing the responsiveness to vasoconstrictor molecules, resulting in severe vasoconstriction. In the original publication that described the antiangiogenic factors, Maynard and colleagues utilized an in vitro assay for microvascular reactivity to assess the hemodynamic effects of circulating sFlt-1 [19]. Although the antiangiogenic factor itself did not cause significant vasoconstriction, it blocked the dose-dependent increase in vasodilatation induced by VEGF and PlGF. Furthermore, soluble endoglin (sEng) deleteriously affects vascular tone by blocking the activation of endothelial nitric oxide synthase [20].
Glomerular Endotheliosis
Preeclampsia is the most common cause of renal insufficiency and proteinuria during pregnancy. Compared with the healthy pregnant state, preeclampsia presents with variable degrees of renal insufficiency. A study that utilized precise physiological measurements in conjunction with morphometric analysis of postpartum biopsies to examine the determinants of the GFR in 13 women with preeclampsia and 12 healthy gravid controls noted GFR to be significantly depressed in women with preeclampsia compared with healthy controls (91 vs. 149 ml/min/1.73m2, respectively; p < 0.0001) [28]. Compared with tissue obtained from healthy female kidney transplant donors, the morphometric analysis revealed numerous significant ultrastructural differences, including swelling of the endothelial cells, the presence of subendothelial fibrinoid deposition, and mesangial cell interposition along with partial effacement of the renal podocyte or foot process.
In the kidney, the renal podocyte has been shown to be the site of VEGF production in vivo. VEGF receptors are expressed on the endothelial cells, suggesting that the VEGF produced by the podocyte travels against the flow of filtrate to its receptor. Thus, paracrine and autocrine pathways could very well exist that govern the integrity of the glomerular filtration barrier, and tight regulation of VEGF signaling is necessary to maintain a healthy glomerulus [29]. Mice with a homozygous deletion in podocyte-specific VEGF fail to develop a filtration barrier, a uniformly lethal condition. Podocyte-specific heterozygosity, on the other hand, resulted in glomerular endotheliosis and proteinuria, a lesion reminiscent of human preeclampsia. In another rat model wherein overexpression of sFlt-1 produced hypertension, proteinuria, and glomerular endotheliosis, VEGF121 treatment improved the clinical symptoms as well as renal histology [30]. Human data linking endothelial injury with enhanced glomerular permeability in preeclampsia includes two studies. The first study noted decreased glomerular expression of podocyte specific proteins, nephrin and synaptopodin, in renal tissue from autopsies of women who died from preeclampsia compared with women who died from trauma [31]. The same authors demonstrated that podocyturia (loss of podocytes into the urine) was associated with preeclampsia and correlated with the degree of proteinuria [32]. One can therefore postulate that in preeclamptic women, high levels of circulating sFlt-1 systematically deprive the glomeruli of local VEGF signaling, result in the renal pathological features frequently referred to as glomerular endotheliosis, and damage the glomerular barrier increasing albumin permeability.
Despite this significant reduction in GFR, blood urea nitrogen and serum creatinine often remain within the normal nonpregnancy range [33]. The proteinuria is nonselective, but is mainly constituted of albumin [34]. The urinary sediment in preeclamptic women is usually benign. However, microscopic hematuria is not uncommon in pregnant women [35]. Both the renal insufficiency and proteinuria resolve after delivery of the placenta, further highlighting the importance of the placental-derived antiangiogenic factors.
HELLP Syndrome
The HELLP syndrome (Hemolysis, Elevated Liver Enzyme Levels and Low Platelets) occurs in 10–20% of patients with preeclampsia and is characterized by hemolysis with a microangiopathic blood smear, elevated liver enzyme tests, and low platelet count. Occasionally, subcapsular liver bleeding or liver rupture may complicate the clinical picture. These clinical manifestations also occur as a result of diffuse maternal vascular endothelial injury along with impaired synthesis of endogenous anticoagulant and increased procoagulant synthesis. It usually resolves within 7 days after delivery of the placenta, again implicating the antiangiogenic factors along with the potential for a dose-response relationship. Furthermore, data exist to suggest that sEng might be particularly important in the evolution of the HELLP Syndrome from preeclampsia. Utilizing an adenovirus vector, sFlt-1 and sEng were isolated from maternal serum and injected into an animal model [20]. Alone sFlt-1 resulted in hypertension and proteinuria, but when given in conjunction with sEng, the rats developed more significant hypertension and proteinuria along with increased liver enzymes and a decreased platelet count.
Eclampsia
Eclampsia is defined as the sudden onset of a grand mal seizure typically in the presence of hypertension and proteinuria. Other neurological manifestations of preeclampsia include blurry vision, headache, or in rare cases, transient loss of vision (cortical blindness). These manifestations have been attributed to severe elevations in blood pressure, which subsequently lead to cerebral edema. Other contributing elements include thrombotic microangiopathic injury and cerebral vasoconstriction. Cerebral edema mainly involves the posterior white hemispheres and is referred to as reversible posterior leukoencephalopathy syndrome (PRES), which is best observed by magnetic resonance imaging [36, 37]. Again resolution in the early postpartum period implicates the antiangiogenic factors. In adult mice, the roles of VEGF and TGF-beta were investigated with respect to the integrity of the choroid plexus [38]. Receptors for VEGF and TGF-beta were detected, and inhibition of VEGF with maternally derived antiangiogenic factors led to decreased choroid plexus vascular perfusion and fibrin deposition. Simultaneous blockade of VEGF and TGF-beta resulted in the loss of fenestrae on choroid plexus vasculature and the development of periventricular edema, mimicking human PRES. In human studies, progressing from preeclampsia to eclampsia may be a dose-response relationship, as the mean levels of both sFlt-1 and sEng were noted to be significantly higher in the women who developed eclampsia [39].
Cardiac Manifestations
Severe preeclampsia is characterized by rapid weight gain, with edema of the face, hands, and feet. The edema is thought to be in part secondary to salt and water retention. Furthermore, hypoalbuminemia secondary to urinary protein loss also contributes to the edema formation in preeclamptic women. Pulmonary edema indicates severe preeclampsia, suggesting cardiac dysfunction. In the aforementioned animal studies wherein both sFlt-1 and sEng were infused, the sacrificed animals also demonstrated increased microvascular permeability in the lungs [20]. In a very recent study, the authors sought to assess the link between postpartum cardiomyopathy, preeclampsia, and the antiangiogenic factors [40••]. The two conditions frequently coexist, as women with postpartum cardiomyopathy are prone to the development of preeclampsia, and the levels of antiangiogenic levels in the serum of women with postpartum cardiomyopathy are higher compared to controls. They studied PGC-1 alpha, a transcriptional cofactor that is highly expressed in cardiac muscle. It drives mitochondrial biogenesis and induces expression and secretion of proangiogenic factors, such as VEGF, to form new blood vessels. In female knockout mice for PGC-1 alpha, progressive pregnancies resulted in death due to dilated cardiomyopathy. To also test the hypothesis that cardiac dysfunction occurs in women with preeclampsia, cardiac function was assessed by sensitive markers of diastolic dysfunction (the myocardial performance index (MPI) as well as E/E that measures flow velocities). Both were significantly worse in women with preeclampsia. Furthermore, the degree of cardiac dysfunction correlated with sFlt-1 levels. In their final experiment, sFlt-1 from the serum of women with preeclampsia was injected into control animals and knockout mice for PGC-1 alpha. Although both developed myocardial dysfunction, the condition was more severe in the knockout mice. As such, the release of antiangiogenic factors during severe preeclampsia results in cardiac dysfunction. Furthermore, the late pregnancy release in select susceptible women with insufficient local proangiogenic defenses in the heart may result in postpartum cardiomyopathy providing novel insights into both conditions along with the potential for future treatment strategies.
Diagnosis
At present, the diagnosis of preeclampsia remains a clinical diagnosis that can be particularly challenging in young women with other comorbidities, such as hypertension or renal disease. Furthermore, the disease manifestations are nonspecific, and therefore, other conditions that may necessitate treatments other than delivery often have to be distinguished from preeclampsia. Finally, preeclampsia may be superimposed on these very same conditions that place women at risk for placental disease. Thus, a coordinated approach that involves both obstetrical and medical specialists is necessary to determine the optimal management in women presenting with new onset or worsening hypertension and proteinuria, as a careful assessment of placental function and fetal status is necessary to make the diagnosis. In the future, however, assays of the angiogenic and antiangiogenic factors may prove to be helpful in some clinical situations.
Increased sFlt-1 and sEng along with decreased serum and urine PlGF and VEGF levels have been demonstrated to precede the clinical syndrome and are correlated with disease severity. The level of sFlt-1 has been documented to increase several weeks [41], whereas sEng has been documented to increase several months before the onset of the clinical syndrome [42]. Increased sFlt-1 and sEng along with decreased serum and urine PlGF and VEGF levels result in an adjusted odds ratio of 31.6 (95% CI 10.7-93.4) for the development of early-onset preeclampsia [42], but to facilitate widespread clinical use a better understanding of the serum level that identifies the presence of placental compromise will be necessary. In a recent study, a sFlt-1/PlGF ratio of 85 differentiated adverse outcomes from unremarkable pregnancies in women who presented before 34 weeks gestation [43••]. However, a recent systematic review that synthesized results of 34 studies calculated summary diagnostic odds ratios of PlGF 9.0 (95% CI 5.6–14.5), sFlt-1 6.6 (95% CI 3.1–13.7), and sEng 4.2 (95% CI 2.4–7.2), which correspond to sensitivities of 32%, 26%, and 18%, respectively. The authors concluded that the test accuracies of all four markers might be too poor for accurate prediction of preeclampsia in clinical practice [44]. To date, however, the antiangiogenic factor assays have been used to discriminate preeclampsia from other etiologies of renal compromise, and have proven useful in a variety of select clinical scenarios, including presumed glomerulonephritis [45], lupus [46], and in patients on hemodialysis [47]. Further studies, particularly in women with comorbidities, are required as the necessary amount of antiangiogenic factor released from a placenta to cause worsening hypertension and proteinuria, in a woman with underlying renal disease or hypertension, for example, may depend on the degree of already present vascular endothelial damage.
Until there is standardization and widespread availability of the angiogenic and antiangiogenic assays, one can glean important insights about the placenta from more readily available obstetrical assessments, including maternal biochemistry, placental, and fetal ultrasounds as well as uterine artery Doppler assessments (Table 2 and see www.mountsinai.on.ca/care/placenta-clinic). Components of the first trimester and maternal serum screen provide early insights into placental integrity [48]. Pregnancy-associated plasma protein A (PAPP-A) is released from the developing placenta and activates factors required for fetal growth. As such, low levels reflect an inadequate placental footprint [49]. Alpha fetoprotein (AFP) is produced by the fetal liver, and high levels in a structurally normal fetus suggest loss of placental integrity. Both total human chorionic gonadotropin (hCG) and the Dimeric Inhibin Assay (DIA) are made by the syncytio trophoblast layer. As such, elevations in both levels are suggestive of potentially severe preeclampsia. When all these tests are normal, the odds ratio for developing placental disease is low (odds ration 0.2; 95% CI 0.1–0.4) [50]. Ultrasound can be used to assess placental morphology and fetal growth. Finally, alterations in uterine artery flow also relate closely to the clinical symptoms of preeclampsia, as mechanical uterine artery constriction in animal models has been shown to lead to hypertension and proteinuria [51]. In addition, changes in uterine flow from the first to the second trimester correlate with intrauterine growth restriction and hypertensive disorders of pregnancy; and clinically, an abnormal mean pulsatility index represents the greatest risk for adverse perinatal outcomes [52].
Conclusions
An enhanced understanding of the pathogenesis of preeclampsia will facilitate identification of women at risk such that these women may benefit from preventative strategies that exist and become available, as well as enhanced surveillance during pregnancy such that maternal and fetal complications can be minimized. The angiogenic and antiangiogenic factors may prove useful to assist with the prediction of preeclampsia before the onset of the clinical syndrome and may assist with diagnosis in complicated cases. Finally, treatment strategies designed to prolong gestation are in evolution. Most recently, a small pilot study utilized dextran sulfate cellulose apheresis treatments and successfully reduced circulating sFlt-1 levels in a dose-dependent fashion without apparent adverse effects on mother or fetus [53•]. Further studies will determine the feasibility of using clearance techniques to manage the growing number of women affected by placental disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ. 2005;330:565.
Lamminpaa R, Vehvilainen-Julkunen K, Gissler M, Heinonen S. Preeclampsia complicated by advanced maternal age: a registry-based study on primiparous women in Finland 1997-2008. BMC Pregnancy and Childbirth. 2012;12:47.
Calhoun KC, Barnhart KT, Elovitz MA, Srinivas SK. Evaluating the Association between Assisted Conception and the Severity of Preeclampsia. ISRN Obstetrics and Gynecology. 2011;2011:928592.
Kanter D, Lindheimer MD, Wang E, et al. Angiogenic dysfunction in molar pregnancy. Am J Obstet Gynecol. 2010;202:184 e1-5.
Sultana R, Chen XK, Lee C, Hader J. Outcomes in multiple gestation pregnancies among Canadian women age 35 years and older. Healthcare quarterly (Toronto, Ont). 2011;14:22–4.
Haavaldsen C, Tanbo T, Eskild A. Placental weight in singleton pregnancies with and without assisted reproductive technology: a population study of 536,567 pregnancies. Hum Reprod. 2012;27:576–82.
Nilsson E, Salonen Ros H, Cnattingius S, Lichtenstein P. The importance of genetic and environmental effects for pre-eclampsia and gestational hypertension: a family study. BJOG. 2004;111:200–6.
Skjaerven R, Vatten LJ, Wilcox AJ, Ronning T, Irgens LM, Lie RT. Recurrence of pre-eclampsia across generations: exploring fetal and maternal genetic components in a population based cohort. BMJ. 2005;331:877.
Campbell DM, MacGillivray I, Carr-Hill R. Pre-eclampsia in second pregnancy. Br J Obstet Gynaecol. 1985;92:131–40.
Sibai BM, Mercer B, Sarinoglu C. Severe preeclampsia in the second trimester: recurrence risk and long-term prognosis. Am J Obstet Gynecol. 1991;165:1408–12.
Gaugler-Senden IP, Berends AL, de Groot CJ, Steegers EA. Severe, very early onset preeclampsia: subsequent pregnancies and future parental cardiovascular health. Eur J Obstet Gynecol Reprod Biol. 2008;140:171–7.
North RA, McCowan LM, Dekker GA, et al. Clinical risk prediction for pre-eclampsia in nulliparous women: development of model in international prospective cohort. BMJ. 2011;342:d1875.
Deen ME, Ruurda LG, Wang J, Dekker GA. Risk factors for preeclampsia in multiparous women: primipaternity versus the birth interval hypothesis. J Matern Fetal Neonatal Med. 2006;19:79–84.
Roberts CL, Ford JB, Algert CS, et al. Population-based trends in pregnancy hypertension and pre-eclampsia: an international comparative study. BMJ open. 2011;1:e000101.
Skjaerven R, Wilcox AJ, Lie RT. The interval between pregnancies and the risk of preeclampsia. N Engl J Med. 2002;346:33–8.
Salha O, Sharma V, Dada T, et al. The influence of donated gametes on the incidence of hypertensive disorders of pregnancy. Hum Reprod. 1999;14:2268–73.
Lim KH, Zhou Y, Janatpour M, et al. Human cytotrophoblast differentiation/invasion is abnormal in pre-eclampsia. Am J Pathol. 1997;151:1809–18.
Zhou Y, Damsky CH, Fisher SJ. Preeclampsia is associated with failure of human cytotrophoblasts to mimic a vascular adhesion phenotype. One cause of defective endovascular invasion in this syndrome? J Clin Invest. 1997;99:2152–64.
Maynard SE, Min JY, Merchan J, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003;111:649–58.
Venkatesha S, Toporsian M, Lam C, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med. 2006;12:642–9.
Bdolah Y, Lam C, Rajakumar A, et al. Twin pregnancy and the risk of preeclampsia: bigger placenta or relative ischemia? Am J Obstet Gynecol. 2008;198:428 e1-6.
Silasi M, Rana S, Powe C, et al. Placental expression of angiogenic factors in Trisomy 13. Am J Obstet Gynecol. 2011;204:546 e1-4.
Bdolah Y, Palomaki GE, Yaron Y, et al. Circulating angiogenic proteins in trisomy 13. Am J Obstet Gynecol. 2006;194:239–45.
Bortoloso E, Del Prete D, Gambaro G, et al. Vascular endothelial growth factor (VEGF) and VEGF receptors in diabetic nephropathy: expression studies in biopsies of type 2 diabetic patients. Ren Fail. 2001;23:483–93.
ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol. 2002;99:159–67.
Chapman AB, Abraham WT, Zamudio S, et al. Temporal relationships between hormonal and hemodynamic changes in early human pregnancy. Kidney Int. 1998;54:2056–63.
Halligan A, O’Brien E, O'Malley K, et al. Twenty-four-hour ambulatory blood pressure measurement in a primigravid population. J Hypertens. 1993;11:869–73.
Lafayette RA, Druzin M, Sibley R, et al. Nature of glomerular dysfunction in pre-eclampsia. Kidney Int. 1998;54:1240–9.
Eremina V, Sood M, Haigh J, et al. Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J Clin Invest. 2003;111:707–16.
Li Z, Zhang Y, Ying Ma J, et al. Recombinant vascular endothelial growth factor 121 attenuates hypertension and improves kidney damage in a rat model of preeclampsia. Hypertension. 2007;50:686–92.
Garovic VD, Wagner SJ, Petrovic LM, et al. Glomerular expression of nephrin and synaptopodin, but not podocin, is decreased in kidney sections from women with preeclampsia. Nephrol Dial Transplant. 2007;22:1136–43.
Garovic VD, Wagner SJ, Turner ST, et al. Urinary podocyte excretion as a marker for preeclampsia. Am J Obstet Gynecol. 2007;196:320 e1-7.
Hladunewich MA, Lafayette RA, Derby GC, et al. The dynamics of glomerular filtration in the puerperium. Am J Physiol Renal Physiol. 2004;286:F496–503.
Moran P, Baylis PH, Lindheimer MD, Davison JM. Glomerular ultrafiltration in normal and preeclamptic pregnancy. J Am Soc Nephrol. 2003;14:648–52.
Brown MA, Holt JL, Mangos GJ, Murray N, Curtis J, Homer C. Microscopic hematuria in pregnancy: relevance to pregnancy outcome. Am J Kidney Dis. 2005;45:667–73.
Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494–500.
Aukes A, De Groot J, Wiegman M, Aarnoudse J, Sanwikarja G, Zeeman G. Long-term cerebral imaging after pre-eclampsia. BJOG. 2012;119:1117–22.
Maharaj AS, Walshe TE, Saint-Geniez M, et al. VEGF and TGF-beta are required for the maintenance of the choroid plexus and ependyma. The Journal of experimental medicine. 2008;205:491–501.
Vaisbuch E, Whitty JE, Hassan SS, et al. Circulating angiogenic and antiangiogenic factors in women with eclampsia. Am J Obstet Gynecol. 2011;204:152 e1-9.
•• Patten IS, Rana S, Shahul S, et al. Cardiac angiogenic imbalance leads to peripartum cardiomyopathy. Nature. 2012;485:333–8. This important series of experiments noted the association between the antiangiogenic factors, preeclampsia and peripartum cardiomyopathy. The two conditions frequently coexist as women with postpartum cardiomyopathy are prone to the development of preeclampsia, and the levels of antiangiogenic levels in the serum of women with postpartum cardiomyopathy are higher compared to controls. Further, women with preeclampsia were noted to have diastolic dysfunction that correlated with the serum level of sFlt-1.
Levine RJ, Maynard SE, Qian C, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350:672–83.
Levine RJ, Lam C, Qian C, et al. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med. 2006;355:992–1005.
•• Rana S, Hacker MR, Modest AM, et al. Circulating angiogenic factors and risk of adverse maternal and perinatal outcomes in twin pregnancies with suspected preeclampsia. Hypertension. 2012;60:451–8. This recent work from Dr. Karumanchi’s laboratory noted a sFlt-1/PlGF ratio of 85 identified the evolution of untoward pregnancy outcomes in women who presented prior to 34 weeks gestation.
Kleinrouweler CE, Wiegerinck MM, Ris-Stalpers C, et al. Accuracy of circulating placental growth factor, vascular endothelial growth factor, soluble fms-like tyrosine kinase 1 and soluble endoglin in the prediction of pre-eclampsia: a systematic review and meta-analysis. BJOG. 2012;119:778–87.
Hladunewich MA, Steinberg G, Karumanchi SA, et al. Angiogenic factor abnormalities and fetal demise in a twin pregnancy. Nat Rev Nephrol. 2009;5:658–62.
Williams WW, Ecker JL, Thadhani RI, Rahemtullah A. Case records of the Massachusetts General Hospital. Case 38-2005. A 29-year-old pregnant woman with the nephrotic syndrome and hypertension. N Engl J Med. 2005;353:2590–600.
Shan HY, Rana S, Epstein FH, Stillman IE, Karumanchi SA, Williams ME. Use of circulating antiangiogenic factors to differentiate other hypertensive disorders from preeclampsia in a pregnant woman on dialysis. Am J Kidney Dis. 2008;51:1029–32.
Huang T, Hoffman B, Meschino W, Kingdom J, Okun N. Prediction of adverse pregnancy outcomes by combinations of first and second trimester biochemistry markers used in the routine prenatal screening of Down syndrome. Prenat Diagn. 2010;30:471–7.
Proctor LK, Toal M, Keating S, et al. Placental size and the prediction of severe early-onset intrauterine growth restriction in women with low pregnancy-associated plasma protein-A. Ultrasound Obstet Gynecol. 2009;34:274–82.
Toal M, Chan C, Fallah S, et al. Usefulness of a placental profile in high-risk pregnancies. Am J Obstet Gynecol. 2007;196:363 e1-7.
Alexander BT, Llinas MT, Kruckeberg WC, Granger JP. L-arginine attenuates hypertension in pregnant rats with reduced uterine perfusion pressure. Hypertension. 2004;43:832–6.
Gomez O, Figueras F, Martinez JM, et al. Sequential changes in uterine artery blood flow pattern between the first and second trimesters of gestation in relation to pregnancy outcome. Ultrasound Obstet Gynecol. 2006;28:802–8.
• Thadhani R, Kisner T, Hagmann H, et al. Pilot Study of Extracorporeal Removal of Soluble Fms-Like Tyrosine Kinase 1 in Preeclampsia / Clinical Perspective. Circulation. 2011;124:940–50. This small pilot study utilized dextran sulfate cellulose apheresis treatments to reduce circulating sFlt-1 levels in a dose-dependent fashion. Following numerous treatments in 3 women with severe early onset preeclampsia, the extracorporeal system lowered circulating sFlt-1 levels, reduced proteinuria, and stabilized blood pressure without apparent adverse maternal or fetal effects.
Disclosures
H. Alhorzali: none; J. Kingdom: none; M.A. Hladunewich.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alhozali, H., Kingdom, J. & Hladunewich, M.A. Early Diagnosis of Preeclampsia. Curr Obstet Gynecol Rep 1, 190–197 (2012). https://doi.org/10.1007/s13669-012-0026-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-012-0026-3