Abstract
Background
There are a myriad of proteins responsible for modulation of expenditure of energy. Angiotensin II (Ang II) is a vital component of renin-angiotensin system that affects blood pressure and also linked to both cachexia and obesity via fat and muscle metabolism. Previous research suggests that the direct action of Ang II is on the brain, via angiotensin II type 1 receptor protein, affecting food intake and energy expenditure. The objective of the study is to investigate the effect of 1-sarcosine (SAR)-Ang II infusion on energy expenditure and metabolism in a rat model of congestive heart failure cachexia.
Methods
Adult female rats of the Sprague Dawley strain (n = 33) were used (11 pair-fed control, 12 ad libitum and 10, 1-sarcosine–angiotensin II-infused rats). Body weight, faecal excretion, feed intake (in grams), water intake (in milliliters) and urine excreted were recorded daily. The measurements were recorded in three different periods (4 days prior to surgery, “pre-infusion”; day of surgery and 5 days postsurgery, “infusion period”; days 7 to 14, “recovery” period). Different analytical methods were used to measure energy expenditure per period, uncoupling protein 3 mRNA expression, crude protein and adipose tissue body composition.
Results
During the infusion period, the SAR–Ang II group experienced rapid weight loss (p < 0.05) in comparison to the ad libitum and pair-fed groups. The SAR–Ang II group displayed lower (p < 0.05) body fat content (in percent) than the controls. There was also increased (p < 0.05) uncoupling protein 3 (UCP3) mRNA expression in the SAR–Ang II group and pair-fed group when compared to the controls.
Conclusion
In summary, the results suggest that SAR–Ang II infusion impairs appetite and decreases body weight by wasting predominantly adipose tissue, which may be due to elevated energy expenditure via mitochondrial uncoupling (UCP3 protein activity).
Similar content being viewed by others
1 Introduction
Cachexia is derived from the Greek “Kakos” and “Hexis”, literal translation “bad condition” and associated with severe muscle emaciation, loss of adipose tissue, and characterized by abnormality of physiological processes in protein, carbohydrate, and fat metabolism [1]. Cachexia is frequently prevalent as end-point of many chronic diseases such as congestive heart failure (CHF), resulting in increased energy expenditure despite sufficient protein and calorie intake [2]. Most of the studies analyzing energy expenditure in cachexia have been performed on humans, thereby limiting the understanding of the underlying specific molecular mechanisms [2–4]. However, proteolysis is closely linked with proinflammatory cytokines such as TNF-α, IL-1, and IL-6 via the upregulation of ubiquitin ligases like muscle RING finger protein-1 (MuRF1) and muscle atrophy F-box (MAFbx), suppression of hepatic growth hormone receptor (GHr), and insulin-like growth factor (IGF-1) expressions via elevated glucocorticoids [5] and decrease of the orexigenic peptides, AgRP and ghrelin [6], in culmination affecting skeletal muscle content and feed intake. Moreover, angiotensin II (Ang II) inhibits 5′ AMP-activated protein kinase (AMPK) activity, altering energy metabolism and also serum amyloid-A, glucocorticoids, and myostatin-altering muscle protein metabolism [7]. Moreover, blockage of angiotensin II type 1 (AT1) receptors in the brain leads to body weight loss due to hypophagia [8]. Earlier studies indicated that Ang II infusion in rats induces CHF, leading to weight loss [9, 10]. IGF-I was suggested as a key mechanism implicated in the development of CHF in this model of wasting. There is a reduction in IGF-I circulationg, resulting in reduced lean mass and high protein degradation through blockage of the autocrine IGF-I system [9, 11–13]. More recent findings suggest that Ang II causes skeletal muscle wasting in rodents by reducing skeletal muscle regeneration via inhibition of satellite cell proliferation [7]. Moreover, another trial concluded that weight loss was due to both decreased feed intake and an independent component, i.e., IGF-I or uncoupling protein 1 (UCP1) thermogenesis [11]. Increase in the sympathetic neurotransmission in intrascapular brown adipose tissue was hypothesized to be one of the other probable mechanisms for weight loss [14].
Porter et al. indicated that UCP1 played a role in brown adipose tissue thermogenesis, but it did not explain the increase in energy expenditure in tissues, especially liver [11]. This emphasizes the need for further research on UCP levels in these tissues. Several research indicate the probable role of UCP in cachexia and could be the cause for unexplained increase in energy expenditure [15, 16], which also would impact exercise capability of the individual [17]. Interestingly, Ang II was known to induce cachexia in old rats and restrict growth in young rats by progressive muscle atrophy and lipolytic effects [18, 19].
The aim of the current study was to investigate if the Ang II-induced weight loss seen in previous studies was attributed to increased energy expenditure, caused by elevated UCP3 mRNA expression in the skeletal muscle tissue. Sarcosine–angiotensin II (N-methyl glycine–angiotensin II) was used to induce CHF wasting instead of Ang II due to it being a potent analog, which has a higher affinity for the AT1 receptor than Ang II, thus potentiating its effect [20, 21].
2 Materials and methods
2.1 Animals
All experiments were performed with animal ethics committee approval (La Trobe University) (01/22L). Adult female Sprague Dawley rats, weighing 250–350 g, were sourced from the University of Melbourne, Australia. Thirty-three rats were used (11 pair-fed control, 12 ad libitum, and 10 [1-sarcosine]–angiotensin II-infused rats). Food was provided daily, consisting of barastoc rat chow ration (Ridley AgriProducts Pty Ltd., VIC, Australia) and distilled water.
Body weight, feed intake (in grams), water intake (in milliliters), fecal excretion, and urine excretion (in milliliters) were determined daily. All these were noted in three periods divided into 4-, 6-, and 8-day intervals. The periods included 4 days prior to surgery (pre-infusion period of a 4-day interval prior to the day of surgery). Known as the infusion period is the 5 days after surgery, including the surgery day (6-day interval), and days 7 to 14 known as the recovery period consisting of an 8-day interval. The energy and moisture content were determined using the dried and weighed feces and feed (Fig. 1).
2.2 Surgery and osmotic mini-pump implantation
The osmotic mini-pumps (Alzet model 2001) were filled with 200 μl of 1-sarcosine (SAR)–Ang II and infused at a rate of 500 ng/kg live body weight/min (1.0 μl of infusate per hour ± 0.03 μl). Angiotensin was dissolved in saline that was acidified with 0.01 M acetic acid, and the sterility of the infusate was maintained by pumping the solution through a 0.22-μM filter. For anesthesia, an intraperitoneal (lower left quarter) injection of 60 mg/kg ketamine (100 mg/mL) and 12 mg/kg xylazine (20 mg/mL)) were used. A midscapular incision was made, and the osmotic pump was inserted with the flow modulator facing away from the site. The wound was closed using Michel clips (10 × 3 mm) and sutured with 2.0 Dexon.
2.3 Organ sample collection for weight and RNA extraction
Organs such as the liver, heart, kidney, lungs, and spleen were removed, leaving the carcass (body with visceral organs removed). The tissue samples of the skeletal muscle, liver, heart, spleen, and adipose tissue were placed in 1-mL RNA and then frozen at −70 °C for subsequent mRNA analysis.
2.4 Carcass homogenization and moisture content
The weight of the major organs was noted after emptying the whole carcasses of their viscera. The carcass was weighed and then frozen at −20 °C. A meat grinder (Porkret, Czech Republic; 2-mm die cast size) was used to homogenize the carcass and organs, which were diced frozen into small cubes of 10 × 10 × 10 mm. In order to evaluate the moisture content, a subsample of each rat homogenate was then dried at 60 °C until the weight is stable.
2.5 Organic matter and gross energy determination
Two sample types were used to analyze ash, feed, and carcass. The residual organic matter was removed by firing the crucibles at 550 °C for 1 h. The samples were placed in the crucibles, weighed, and then fired at 550 °C for 5 h. The covariation of the average was 8.4 %. A PARR 1261 bomb calorimeter (PARR Instrument Co., IL, USA) was used to measure the gross energy (in megajoules per kilogram) of feed and carcasses. The dried sample was converted into a pellet (∼0.5 g) and placed in the bomb for combustion. The coefficient of variation was 0.19 %.
2.6 Kjeldhal nitrogen (crude protein)
The Kjeldhal method was employed to determine crude protein for body composition of the rat carcass by using Kjeltec Auto 1035. The dried homogenate was powdered and ∼0.5 g was used for protein analysis. Later, the tube was heated to 550 °C on a programmed heating block for 1 h following the addition of 5 mL of concentrated H2SO4 (ACS reagent 98 % purity). Catalyzation was facilitated by adding a selenium tablet, and accuracy and recovery was determined using a standard of ammonium sulfate. Nitrogen percent values were multiplied by 6.25 to determine protein content. The coefficient of variation was 0.44 % of the mean.
2.7 Adipose tissue determination with Soxhlet apparatus
A filter paper (Whatman 541) was used to hold the dried homogenized carcass tissue. The residual H2O was removed by placing it in an oven at 70 °C for 24 h, and later kept in a desiccator. The parcel was weighed and placed in a Soxhlet apparatus. Absolute chloroform/absolute methanol (2:1) was the solvent mixture used for fatty acid extraction. The coefficient of variation was 8.16 %.
2.8 Energy expenditure per period
For each period, rats were sacrificed to obtain energy content of the carcass use for calculating energy expenditure for that period. The “initial carcass (megajoules)” is the energy content (gross energy) of the carcass at the commencement of the period (4 days prior to surgery, day of surgery, date of infusion cessation, and last day of recovery). The following equation was used to calculate the energy expenditure per period (carcass):
2.9 Uncoupling protein mRNA expression
Muscle tissues were collected to extract mRNA for analyzing glyceraldehyde 3-phosphate dehydrogenase (GAPDH; control) and UCP3. The samples were placed in RNAlater (Ambion, Inc.), allowing it to perfuse the tissue for 2 h at room temperature, following which they were stored at −70 °C. RNA yield was determined by measuring absorbance at 260 nm and purity (i.e., 1:2:1) for the amount of carbohydrate, DNA/RNA, and protein present at 230/260/280 nm, respectively. Four primer pairs were designed using published amino acid sequences of UCP3 species from the National Centre for Biotechnology Information (NCBI) website. The primers used in real-time PCR were designed and manufactured by Gene Works Pty Ltd (Adelaide, Australia). The iScript One-step RT-PCR kit with SYBR Green was used for reverse transcription and PCR.
2.10 Statistical analysis
Univariate or multivariate analysis was performed to determine the mean, standard error, and standard deviation. Least squares difference, Bonferroni, and Tukey’s tests were performed using p < 0.05. SPSS 12.0.1 for Windows (www.spss.com) was used to process the statistical analysis.
3 Results
The initial weights in all the groups were similar. Rapid weight loss (p < 0.05) was noted in the SAR–Ang II group when compared to the ad libitum and pair-fed groups during the infusion period. Although there was a gradual re-increase in the body weight of Ang II group from day 10 in line with the pair-fed subjects, it was not a significant difference. The regain of weight may be due to compensatory growth (Fig. 2).
The Ang II group displayed less fat content (p < 0.05) in comparison to the controls with no variation in other body compositional parameters. A negative body weight change (p < 0.01; both per gram percent of initial body weight and per gram body weight) was noted in the rats infused with Ang II when compared to controls and pair-fed groups (Tables 1 and 2).
Higher energy expenditure was observed in Ang II rats than the other two groups when the expenditure is expressed per gram of body weight. However, this was substantially higher (p < 0.05) when expressed per gram of skeletal muscle. Although body composition changes may be linked to calorie restriction, an additional component of pair-fed independent weight loss was also investigated.
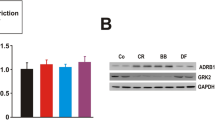
The weights of the liver, kidney, and heart expressed in grams are listed in Table 3. Kidney in the pair-fed group had lower mass (in grams; p < 0.05) than the controls during the infusion period. The weight of the liver was higher in the SAR–Ang II rats during the infusion period than pair-fed and controls. Further, the kidney was larger in the Ang II group when compared to the other two groups in both the infusion and post-infusion phase. Similar results were observed in the infusion period with respect to heart weight (p < 0.05) in SAR–Ang II and pair-fed groups in comparison to the controls. Moreover, an increase in the UCP3 mRNA expression (p < 0.05) in skeletal muscle was noted in the SAR–Ang II and pair-fed groups than the controls (Fig. 3).
4 Discussion
Weight loss during SAR–Ang II-induced CHF may be connected with lower food intake, but another metabolic component may be present. The level of UCP3 mRNA was measured in the skeletal muscle in combination with determination of energy expenditure from feed and carcass in order to further understand the impact of SAR–Ang II on energy metabolism. Although weight loss was observed in the SAR–Ang II group, this could have been due to decreased feed intake as was observed in pair-fed rats, yet a new identified component of weight loss was also seen independent of anorexia. The loss of weight was consistent among muscle, fat, and bone components, suggesting that the reduction in weight may be due to increased metabolic activity. The weight loss induced by SAR–Ang II infusion has generally been attributed to reduced food intake, loss of appetite, and lower energy intake as per other studies [9, 11, 22].
Decreased feed intake via suppressed appetite, coupled with increased energy expenditure is thought to occur via hypothalamic neurons that regulate orexigenic/anorexigenic neuropeptides (i.e., neuropeptide-Y, orexin, and corticotropin-releasing hormone) [23, 24]. Increased expenditure leading to weight loss, which is independent of anorexia maybe due in part to uncoupling protein or another protein such as proteolysis inducing factor (PIF) which uses intracellular Ca2+ as a signaling pathway, and molecular control by a G-protein [25]. Porter and Portraz [26] proposed that weight loss progressed after cessation of angiotensin II infusion due to upregulation of UCP1 in BAT tissue. The current study indicated that a component of reduced weight in the Ang II group may be attributed to an increase in the energy expenditure, but also associated with reduced feed intake. Similar findings were reported in an earlier study wherein increased UCP1 mRNA expression was found in the brown adipose tissue [11]. Another study indicated the effect of intercerebral ventricular Ang II infusions transiently lowering food intake [22]. The relevance of this study is that Ang II decreases feed intake and impacts body weight through calorie restriction although there is a rise in energy expenditure on per gram body weight basis.
Interestingly, the Ang II-infused rats ate less than half the feed as ad libitum, but still had significantly higher energy expenditure per gram body weight. The average body weight of pair-fed and Ang II group was 277.9 and 244.9 g, respectively, at the end of infusion period. However, the total energy expenditure in the Ang II rats was significantly greater indicating that dissipation of the increased energy could be attributed to a futile cycle, i.e., uncoupling proteins. The significance of this finding is it indicates that calorie intake by CHF cachexia patients may not be the only reason for weight gain/loss and highlights the presence of an independent metabolic factor independent of calorie intake or physical activity.
The Ang II-infused rats had significantly higher energy expenditure when compared to both pair-fed and control rats, when expressed as per gram of body weight. A similar trend was noted when energy expenditure was observed on per gram of body protein; however, the difference was not significant when compared to controls. Although this requires further investigation, the degree of adipose tissue loss would also impact the equation and this relationship may not be completely linear. Moreover, another finding was that Ang II rats had ∼33 % more skeletal muscle energy expenditure than pair-fed group although pair-fed rats were 11.8 % heavier at day 5. This implied that there was comparable skeletal muscle energy expenditure between the Ang II rats and controls although the former group ate 50 % less. This serves as conclusive evidence that the energy expenditure is directly elevated by Ang II, especially within skeletal muscle. The present study findings indicate that wasting of adipose tissue, which may occur due to infusion of Ang II in rats, is possibly owing to variation in levels of catabolic hormones that regulate these tissues. We observed that SAR–Ang II infusion induces entire body wasting and not specifically the skeletal muscle.
Further, increased energy expenditure may involve action by hormonal (NE, IGF-I, and leptin) and cellular signaling, resulting in reduced adipose and skeletal muscle tissue. This was consistent with the findings of other studies [13]. Increased energy expenditure noted in Ang II group was similar to that of CHF cachetic patients [2], possibly due to an increase in UCP1 mRNA expression in brown adipose tissue and also other metabolic regulatory factors such as UCP2 and UCP3. An earlier trial demonstrated that resting metabolic rate was ∼18 % higher in CHF patients than in pair-fed controls when indexed per kilogram of fat-free mass [27]. This result suggests that increase in energy expenditure causes negative energy balance, leading to weight loss of both skeletal muscle and adipose tissue.
Although heart weight was unchanged in this study, it has been observed in another study that heart weight increases in Ang II rats with infusion time (p < 0.05) than pair-fed and controls. Huentelman et al. showed that infusion of 200 ng kg−1 min−1 Ang II for 4 weeks resulted in a significant increase in heart weight to body weight ratio [28]. Similarly, liver weight has been observed to be increased (p < 0.05) during left ventricle myofilament dysfunction in the rat [9], but not observed in this study.
Although UCP1 was not measured in the present study, UCP3 has been described to be expressed in skeletal muscle and white adipose tissue and thus be a more direct measure of “metabolism leak” in these tissues, and involved in wasting and weight loss [29, 30]. Further exploration is needed to better understand the tissue-specific elevations in UCPs and other molecular targets to ameliorate muscle wasting such as peroxisome proliferator-activated receptor γ agonists, angiotensin II antagonists, ACE inhibitors, and also testosterone, which modulates postreceptor pathways of insulin, GH, and IGF-1 [31]. Moreover, Ang II infusion significantly increases ROS production and UCP2 mRNA expression. The role of UCPs in chronic diseases such as CHF is to counteract ROS generation [32, 33]. ROS is certainly a hallmark of Ang II-induced cardiac cachexia, related to skeletal muscle atrophy via the ubiquitin–proteasome and elevated expression of the E3 ligases atrogin-1/MuRF-1 and nicotinamide adenine dinucleotide phosphate oxidase) [34]. Considering this, ROS therapy has been shown to be beneficial in Ang II-induced cachexia [35]. Phytotherapeutic treatment using herbal species such as Schizandra chinensis may be effective to reduce ROS levels [36], and hypotensive extracts from Hawthorn fruit (Crataegus monogyna) containing anti-oxidants hyperoside, isoquercitrin, epicatechin, chlorogenic acid, quercetin, rutin, and protocatechuic acid [37] may have the dietary potential to reduce hypertension, ameliorate Ang II-induced cachexia, and modulate UCP protein activity.
5 Conclusions
Infusion of SAR–Ang II in rats led to reduction in body weight through wasting and impairment of appetite, which may be partially attributed to increased energy expenditure, probably induced by UCP3. Both the Ang II and PF groups exerted elevated UCP3 mRNA when compared to ad libitum group and this change could be attributed to decreased feed intake and not a direct angiotensin II effect. Moreover, energy expenditure per body gram was elevated in the Ang II group and not pair-fed, and this UCP3 elevation was due to reduced feed intake and not a direct association of elevated energy expenditure. Although several actions of Ang II may have resulted in wasting in the current study model of CHF, not all mechanisms have been investigated and a conclusion cannot be drawn in direct association with SAR–angiotensin II infusion. An important observation is that UCPs could serve as a link to a complex cascade governing energy expenditure and therefore weight loss in chronic illnesses such as CHF but further investigation is needed to establish an association. Hence, this study may be used as a guide for further research to investigate all the probable mechanisms underlying energy expenditure using gene expression analysis. The findings also emphasize the importance of continuously using this model to analyze the origin of increased energy expenditure, key regulators of body weight composition, and probable treatment strategies.
References
Donohoe CL, Ryan AM, Reynolds JV. Cancer cachexia: mechanisms and clinical implications. Gastroenterol Res Pract. 2011;2011:601434. doi:10.1155/2011/601434.
Toth MJ, Matthews DE. Whole-body protein metabolism in chronic heart failure: relationship to anabolic and catabolic hormones. JPEN J Parenter Enteral Nutr. 2006;30:194–201.
Poehlman ET, Scheffers J, Gottlieb SS, Fisher ML, Vaitekevicius P. Increased resting metabolic rate in patients with congestive heart failure. Ann Intern Med. 1994;121:860–2.
Toth MJ, Gottlieb SS, Fisher ML, Poehlman ET. Daily energy requirements in heart failure patients. Metabolism. 1997;46:1294–8.
Ortiz RM, Kobori H, Conte D, Navar LG. Angiotensin II-induced reduction in body mass is Ang II receptor mediated in association with elevated corticosterone. Growth Horm IGF Res. 2010;20:282–8. doi:10.1016/j.ghir.2010.03.003.
Amitani M, Asakawa A, Amitani H, Inui A. Control of food intake and muscle wasting in cachexia. Int J Biochem Cell Biol. 2013;45:2179–85. doi:10.1016/j.biocel.2013.07.016.
Yoshida T, Galvez S, Tiwari S, Rezk BM, Semprun-Prieto L, Higashi Y, et al. Angiotensin II inhibits satellite cell proliferation and prevents skeletal muscle regeneration. J Biol Chem. 2013;288:23823–32.
Müller-Fielitz H, Markert A, Wittmershaus C, Pahlke F, Jöhren O, Raasch W. Weight loss and hypophagia after high-dose AT1-blockade is only observed after high dosing and depends on regular leptin signalling but not blood pressure. Naunyn Schmiedebergs Arch Pharmacol. 2011;383:373–84. doi:10.1007/s00210-011-0602-5.
Brink M, Wellen J, Delafontaine P. Angiotensin II causes weight loss and decreases circulating insulin-like growth factor I in rats through a pressor-independent mechanism. J Clin Invest. 1996;97:2509–16.
Brink M, Price SR, Chrast J, Bailey JL, Anwar A, Mitch WE, et al. Angiotensin II induces skeletal muscle wasting through enhanced protein degradation and down-regulates autocrine insulin-like growth factor I. Endocrinology. 2001;142:1489–96.
Porter JP, Anderson JM, Robison RJ, Phillips AC. Effect of central angiotensin II on body weight gain in young rats. Brain Res. 2003;959:20–8.
Song YH, Li Y, Du J, Mitch WE, Rosenthal N, Delafontaine P. Muscle-specific expression of IGF-1 blocks angiotensin II-induced skeletal muscle wasting. J Clin Invest. 2005;115:451–8.
Cassis LA, Marshall DE, Fettinger MJ, Rosenbluth B, Lodder RA. Mechanisms contributing to angiotensin II regulation of body weight. Am J Physiol. 1998;274:E867–76.
English V, Cassis L. Facilitation of sympathetic neurotransmission contributes to angiotensin regulation of body weight. J Neural Transm. 1999;106:631–44.
Bing C, Russell ST, Beckett EE, Collins P, Taylor S, Barraclough R, et al. Expression of uncoupling proteins-1, -2 and -3 mRNA is induced by an adenocarcinoma-derived lipid-mobilizing factor. Br J Cancer. 2002;86:612–8.
Bing C, Russell S, Becket E, Pope M, Tisdale MJ, Trayhurn P. Adipose atrophy in cancer cachexia: morphologic and molecular analysis of adipose tissue in tumour-bearing mice. Br J Cancer. 2006;95:1028–37.
Adams V, Anker SD, Schuler G. Muscle metabolism and exercise capacity in cachexia. Curr Pharm Des. 2011;17:3838–45.
Brink M, Price SR, Chrast J, Bailey JL, Anwar A, Mitch WE, et al. Angiotensin II induces skeletal muscle wasting through enhanced protein degradation and down-regulates autocrine insulin-like growth factor I. Endocrinology. 2001;142:1489–96.
Schulze PC, Späte U. Insulin-like growth factor-1 and muscle wasting in chronic heart failure. Int J Biochem Cell Biol. 2005;37:2023–35.
Bihoreau C, Monnot C, Davies E, Teutsch B, Bernstein KE, Corvol P, et al. Mutation of Asp74 of the rat angiotensin II receptor confers changes in antagonist affinities and abolishes G-protein coupling. Proc Natl Acad Sci U S A. 1993;90:5133–7.
Cordopatis P, Manessi-Zoupa E, Theodoropoulos D, Bossé R, Bouley R, Gagnon S, et al. Methylation in positions 1 and 7 of angiotensin II. A structure-activity relationship study. Int J Pept Protein Res. 1994;44:320–4.
Porter JP, Potratz KR. Effect of intracerebroventricular angiotensin II on body weight and food intake in adult rats. Am J Physiol Regul Integr Comp Physiol. 2004;287:R422–8.
Yoshida T, Semprun-Prieto L, Wainford RD, Sukhanov S, Kapusta DR, Delafontaine P. Angiotensin II reduces food intake by altering orexigenic neuropeptide expression in the mouse hypothalamus. Endocrinology. 2012;153:1411–20. doi:10.1210/en.2011-1764.
Yoshida T, Tabony AM, Galvez S, Mitch WE, Higashi Y, Sukhanov S, et al. Molecular mechanisms and signaling pathways of angiotensin II-induced muscle wasting: Potential therapeutic targets for cardiac cachexia. Int J Biochem Cell Biol. 2013;45:2322–32. doi:10.1016/j.biocel.2013.05.035.
Mirza KA, Tisdale MJ. Role of Ca2+ in proteolysis-inducing factor (PIF)-induced atrophy of skeletal muscle. Cell Signal. 2012;24:2118–22. doi:10.1016/j.cellsig.2012.07.016.
Porter JP, Potratz KR. Effect of intracerebroventricular angiotensin II on body weight and food intake in adult rats. Am J Physiol Regul Integr Comp Physiol. 2004;287:R422–8.
Poehlman ET, Scheffers J, Gottlieb SS, Fisher ML, Vaitekevicius P. Increased resting metabolic rate in patients with congestive heart failure. Ann Intern Med. 1994;121:860–2.
Huentelman MJ, Grobe JL, Vazquez J, Stewart JM, Mecca AP, Katovich MJ, et al. Protection from angiotensin II-induced cardiac hypertrophy and fibrosis by systemic lentiviral delivery of ACE2 in rats. Exp Physiol. 2005;90:783–90.
Bing C, Brown M, King P, Collins P, Tisdale MJ, Williams G. Increased gene expression of brown fat uncoupling protein (UCP)1 and skeletal muscle UCP2 and UCP3 in MAC16-induced cancer cachexia. Cancer Res. 2000;60:2405–10.
Busquets S, Almendro V, Barreiro E, Figueras M, Argilés JM, López-Soriano FJ. Activation of UCPs gene expression in skeletal muscle can be independent on both circulating fatty acids and food intake. Involvement of ROS in a model of mouse cancer cachexia. FEBS Lett. 2005;579:717–22.
Trobec K, von Haehling S, Anker SD, Lainscak M. Growth hormone, insulin-like growth factor 1, and insulin signaling-a pharmacological target in body wasting and cachexia. J Cachexia Sarcopenia Muscle. 2011;2:191–200.
Sanders PM, Tisdale MJ. Role of lipid-mobilising factor (LMF) in protecting tumour cells from oxidative damage. Br J Cancer. 2004;90:1274–8.
Guo P, Nishiyama A, Rahman M, Nagai Y, Noma T, Namba T, et al. Contribution of reactive oxygen species to the pathogenesis of left ventricular failure in Dahl salt-sensitive hypertensive rats: effects of angiotensin II blockade. J Hypertens. 2006;24:1097–104.
Sukhanov S, Semprun-Prieto L, Yoshida T, Michael Tabony A, Higashi Y, Galvez S. Angiotensin II, oxidative stress and skeletal muscle wasting. Am J Med Sci. 2011;342:143–7. doi:10.1097/MAJ.0b013e318222e620.
Russell ST, Eley H, Tisdale MJ. Role of reactive oxygen species in protein degradation in murine myotubes induced by proteolysis-inducing factor and angiotensin II. Cell Signal. 2007;19:1797–806.
Ko SH, Choi SW, Ye SK, Yoo S, Kim HS, Chung MH. Comparison of anti-oxidant activities of seventy herbs that have been used in Korean traditional medicine. Nutr Res Pract. 2008;2:143–51. doi:10.4162/nrp.2008.2.3.143.
Zhang Z, Chang Q, Zhu M, Huang Y, Ho WK, Chen Z. Characterization of antioxidants present in hawthorn fruits. J Nutr Biochem. 2001;12:144–52.
Acknowledgments
The authors of this manuscript certify that they comply with the ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia, and Muscle 2010;1:7-8 (von Haehling S, Morley JE, Coats AJ, and Anker SD).
Conflict of interest
Simon Cichello, Richard Weisinger, Joannes Schuijers, and Mark Jois declare that they have no conflict of interest, neither financial or personal relationship, with a third party whose interests could be positively or negatively influenced by this article’s content.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Cichello, S.A., Weisinger, R.S., Schuijers, J. et al. 1-Sarcosine–angiotensin II infusion effects on food intake, weight loss, energy expenditure, and skeletal muscle UCP3 gene expression in a rat model. J Cachexia Sarcopenia Muscle 5, 239–246 (2014). https://doi.org/10.1007/s13539-014-0133-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13539-014-0133-2