Abstract
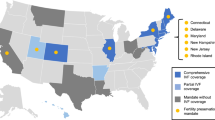
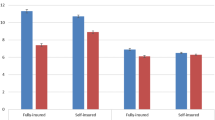
Over the last several decades, both delay of childbearing and fertility problems have become increasingly common among women in developed countries. At the same time, technological changes have made many more options available to individuals experiencing fertility problems. However, these technologies are expensive, and only 25% of health insurance plans in the United States cover infertility treatment. As a result of these high costs, legislation has been passed in 15 states that mandates insurance coverage of infertility treatment in private insurance plans. In this article, we examine whether mandated insurance coverage for infertility treatment affects utilization. We allow utilization effects to differ by age and education, since previous research suggests that older, more-educated women should be more likely to be directly affected by the mandates than younger women and less-educated women, both because they are at higher risk of fertility problems and because they are more likely to have private health insurance, which is subject to the mandate. We find robust evidence that the mandates do have a significant effect on utilization for older, more-educated women that is larger than the effects found for other groups. These effects are largest for the use of ovulation-inducing drugs and artificial insemination.
Similar content being viewed by others
Notes
Although not all fertility treatments are expensive, the less expensive treatments are generally more likely to be covered by health insurance in the absence of mandates, in part because some of them can legitimately be billed under categories covered by most insurance plans.
Effects on health insurance coverage could result either from reduced offering of insurance or reduced take-up.
Intuitively, if the effect of the policy is small for the relevant group relative to the residual variance and zero (or close to zero) elsewhere, or if the subgroup is small, a test for an overall policy effect is more likely than a test for a subgroup-specific policy effect to fail to reject a null hypothesis of zero effect.
This progression is also evident in our data from the NSFG. For example, of the women in the NSFG who reported receiving IVF, about 80% reported receiving male and female testing, 65% also received ovulation-inducing drugs, and 46% also reported artificial insemination. These and other numbers are reported in Table 2 and are discussed in greater detail in the Data and Methodology section.
For additional detail on the mandates, see Schmidt (2005).
An alternative possibility is that the mandates could have a larger impact for younger than older women (conditional on needing treatment), since older women are more likely to have higher incomes and therefore presumably have lower price elasticities of demand. Chambers et al. (2009) reported price elasticities of demand for IVF from developed countries but did not calculate the elasticities by age or education. However, at the same time, younger women face a longer time frame before they become unable to have a child for biological reasons after menopause, and they also may be less likely to be aware of their possible impaired fecundity. In addition, for two women with the same biological ability to have children at each age, the younger woman will still be less likely than the older woman to have difficulty conceiving because of the age-related decline in fecundity.
Data on timing of the first fertility visit is available only for the 1995 and 2002 NSFGs. Fully 30% of all women who ever used ovulation-inducing drugs, 42% of women who used artificial insemination, and 54% of women who ever used IVF have never had a live birth (authors’ tabulations of NSFG data). While some share of these women are likely still getting treatment and may go on to eventually have a live birth, others most likely have been unable to conceive or carry a live birth to term even with treatment. This suggests that a large share of potential treatments might be missed in data that look only at live births. If we limit this calculation to women who had no first birth after their first infertility treatment and have not had a visit for infertility treatment in the past year, assuming that these women might be the most likely to have given up trying to conceive, we see that 15% of those getting any medical help to get pregnant, 16% of those who took ovulation-inducing drugs, and 20% of those getting insemination fall into this category.
One exception is a recent study by Mookim et al. (2008), who used claims data from a set of large firms in 2001–2004 to look at a variety of treatment uses and their impact on outcomes. While they, too, captured a large set of treatments, as with the research on use of ART, their data are from a post-mandate period for most states.
Medically, a woman is defined to be infertile after one year of unsuccessful efforts to become pregnant if she is younger than 35, or after six months of unsuccessful efforts if she is 35 or older.
However, since ERISA exempts self-insured plans, having private insurance is a necessary but not sufficient condition for having a mandate affect one’s coverage of infertility treatment. Unfortunately, no publicly available data allow us to test whether older, highly educated women are more likely than younger or less-educated women to have private insurance from a plan that does not self-insure. A recent study using firm-based data suggests that about 50% of covered workers in 2001 were in plans that were self-insured, and that this number had declined slightly since 1993 (Gabel et al. 2003).
This same group of women is also likely to have higher levels of income with which they could presumably pay for infertility treatments out of pocket. However, the median family income for white women with at least some college education in 2001 was approximately $58,000, which likely would not easily enable a family to pay for infertility treatments out of pocket, given estimates that suggest that the median cost per live delivery resulting from IVF is $56,419 (Collins 2001). More recent estimates from a comparison of developed countries suggest that the gross cost of a single IVF cycle as a percentage of annual disposable income was highest in the United States, at 50%, compared with, for example, 12% in Japan (Chambers et al. 2009).
Claims data, such as those used by Mookim et al. (2008), also include information on various treatments, but only for women with insurance that reimburses them for it. As far as we know, such data are also not publicly available for a period before the mandates.
Simple t tests lead us to reject equality of means across group (high/low education by age 30 and older/age under 30) for all of the outcomes we examine, with p values all well below .01.
All of our dependent variables are binary indicators, and some of their averages are small, which might lead to concerns about the use of least squares. We verified that these results are robust to functional form by estimating the corresponding logistic regressions and calculating marginal effects. Results are quite similar in both magnitude and statistical significance and are available from the authors on request.
We cannot observe private insurance coverage in all waves of our data and likely would not want to use it as a control in any case because it could conceivably respond to the mandates.
Note that if there are offsetting effects in some groups, or small effects in groups that are a larger share of the population, it might be difficult to detect these larger effects for highly educated women when pooling all the data and identifying the policy in a differences-in-differences setting. We have examined this by estimating straight differences-in-differences regressions where the mandate variables are only allowed to vary by state and year. In these analyses, the effects for the overall population are small in magnitude compared with those reported in Tables 4 and 5 for the highly educated older women, and are statistically insignificant. We have also estimated regressions restricted to various subgroups of the population defined by age (education), in which we interact the mandate with education (age). These results are all reported in Online Resource 1.
Previous work by Bundorf et al. (2008) and others has focused primarily on categorizing mandates as “cover including IVF” and “cover excluding IVF.” We do not use this as a primary specification because of concerns raised in a recent study by Conley and Taber (2011) about overrejection in differences-in-differences models with state-level clustering when only a few states change treatment status (only three states are “cover excluding IVF” states). We estimated this as an alternate specification, and the results for ovulation-inducing drugs are significant for “cover including IVF” mandates and slightly larger (0.03 versus 0.024) than the estimated effect for “cover excluding IVF” mandates.
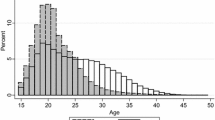
The NSFG is a complex sample survey. Although all waves of the NSFG used were designed to provide data that were nationally representative of the U.S. female population aged 15–44, there have been numerous changes in sample design over time. In particular, different surveys oversampled different groups (e.g., black women in all NSFG waves, but Hispanic women in only 1995 and 2002, and teen women in only 1982). As a result, we use the population weights provided by the NSFG to ensure that the results are population-representative.
The coefficient on medical help to get pregnant has a 95% confidence interval of [0.009, 0.072], which excludes the point estimate for medical help to prevent miscarriage. Similarly, the upper bound for the 95% confidence interval for the miscarriage variable coefficient excludes the coefficient on help to get pregnant. We cannot perform a seemingly unrelated regression test, since women may report medical help to get pregnant or medical help to avoid miscarriage, or both.
Our findings cannot determine whether mandates hasten fertility for women who would have children anyway; allow women to conceive who would not be able to otherwise; or create a form of moral hazard in which they encourage women to wait longer to start trying to conceive, relying on infertility treatment as insurance. Although these are important issues, the NSFG data, despite their many advantages, do not contain information on when women start trying to conceive, how long they had treatment, or whether the treatment itself resulted in a live birth.
One possibility is that in offer states, women receive advice but then realize that they are not covered for more-expensive treatments and thus stop treatment.
Some of these women with no first birth are likely in the middle of treatment and may yet have a child. This is an upper bound on the share of women who are unsuccessful despite obtaining infertility treatment. If we limit this calculation to those women who had no first birth after their first infertility treatment and have not had a visit for infertility treatment in the past year, assuming that these women might be the most likely to have given up trying to conceive, we see that 14% of all women and 15% of the older, more-educated women fall into this category. Of the remaining women, 43% of all women and 46% of the older, more-educated women had a first birth after their first visit; and 29% of both sets of women had already had a first birth before the first visit and may therefore have been seeking treatment for secondary infertility. We cannot determine the outcomes for the women with any first birth before their first visit. We have not further examined these timing variables because they are reported only in the last two waves of the NSFG.
References
Acs, G., Long, S. H., Marquis, M. S., & Short, P. F. (1996). Self-insured employer health plans: Prevalence, profile, provisions, and premiums. Health Affairs, 15, 266–278.
Agency for Healthcare Research and Quality, Center for Financing, Access and Cost Trends. (2005). 2003 Medical Expenditure Panel Survey-Insurance Component Table II.D.1(2003) Average Total Family Premium (in dollars) per enrolled employee at private-sector establishments that offer health insurance by firm size and state: United States, 2003. Retrieved from http://meps.ahrq.gov/mepsweb/data_stats/summ_tables/insr/state/series_2/2003/tiid1.ht
American Society of Reproductive Medicine (ASRM). (2003). Patient fact sheet: Frequently asked questions about infertility. Retrieved from http://www.asrm.org/awards/index.aspx?id=3012
Bao, Y., & Sturm, R. (2004). The effects of state mental health parity legislation in perceived quality of insurance coverage, perceived access to care, and use of mental health specialty care. Health Services Research, 39, 1361–1378.
Bitler, M. (2010). Effects of increased access to infertility treatment on infant and child health outcomes: Evidence from health insurance mandates. Unpublished manuscript, Department of Economics, University of California–Irvine.
Bitler, M., & Carpenter, C. (2011). Insurance mandates and mammography (NBER Working Paper No. 16669). Cambridge, MA: National Bureau of Economic Research.
Bitler, M., & Schmidt, L. (2006). Health disparities and infertility: Impacts of state-level insurance mandates. Fertility and Sterility, 85, 858–865.
Bitler, M., & Zavodny, M. (2010). The effect of Medicaid eligibility expansions on fertility. Social Science & Medicine, 71, 918–924.
Blackburn, M. L., Bloom, D., & Neumark, D. (1993). Fertility timing, wages, and human capital. Journal of Population Economics, 93, 1–30.
Blackwell, R. E., & William M. Mercer Actuarial Team. (2000). Hidden costs of infertility treatment in employee health benefits plans. American Journal of Obstetrics and Gynecology, 182, 891–895.
Buckles, K. (2006). Stopping the biological clock: Fertility therapies and the career/family tradeoff. Unpublished manuscript, Department of Economics, University of Notre Dame, Notre Dame, IN.
Bunce, V. C., & Wieske, J. P. (2010). Health insurance mandates in the states 2010 (CAHI Policy Brief). Alexandria, VA: Council for Affordable Health Insurance Policy.
Bundorf, M. K., Chun, N., Goda, G. S., & Kessler, D. P. (2009). Do markets respond to quality information? The case of fertility clinics. Journal of Health Economics, 28, 718–727.
Bundorf, M. K., Henne, M., & Baker, L. (2008). Mandated health insurance benefits and the utilization and outcomes of infertility treatment (NBER Working Paper No. 12820). Cambridge, MA: National Bureau of Economic Research.
Chambers, G. M., Sullivan, E. A., Ishihara, O., Chapman, M. G., & Adamson, G. D. (2009). The economic impact of assisted reproductive technology: A review of selected developed countries. Fertility and Sterility, 91, 2281–2294.
Chandra, A., & Stephen, E. H. (2005). Infertility and medical care for infertility: Trends and differentials in national self-reported data. Bethesda, MD: Presented at the NIH Conference on Health Disparities and Infertility.
Collins, J. (2001). Cost-effectiveness of IVF. Seminars in Reproductive Medicine, 19, 279–289.
Conley, T. G., & Taber, C. R. (2011). Inference with “difference in differences” with a small number of policy changes. Review of Economics and Statistics, 93, 113–125.
Connolly, M. P., Griesinger, G., Ledget, W., & Postma, M. J. (2009). The impact of introducing patient co-payments in Germany on the use of IVF and ICSI: A price elasticity of demand assessment. Human Reproduction, 24, 2796–2800.
Dehejia, R., & Lleras-Muney, A. (2004). Booms, busts and babies’ health. Quarterly Journal of Economics, 119, 1091–1130.
Gabel, J., Jensen, G. A., & Hawkins, S. (2003). Self-insurance in times of growing and retreated managed care. Health Affairs, 22, 202–210.
Gelbach, J. B., Klick, J., & Wexler, L. (2009). Passive discrimination: When does it make sense to pay too little? University of Chicago Law Review, 76, 797–857.
Gleicher, N. (2000). Cost-effective infertility care. Human Reproduction Update, 6, 190–199.
Gocial, B. (1995). Primary therapy for tubal disease: Surgery versus IVF. International Journal of Fertility and Menopausal Studies, 40, 297–302.
Gruber, J. (1994). State-mandated benefits and employer-provided health insurance. Journal of Public Economics, 55, 433–464.
Hamilton, B., & McManus, B. (2005). Infertility treatment markets: The effects of competition and policy. Unpublished manuscript, Olin School of Business, Washington University, St. Louis, MO.
Henne, M. B., & Bundorf, M. K. (2008). Insurance mandates and trends in infertility treatments. Fertility and Sterility, 89, 66–73.
Jain, T., Harlow, B. L., & Hornstein, M. D. (2002). Insurance coverage and outcomes of in vitro fertilization. New England Journal of Medicine, 347, 661–666.
Jensen, G. A., Rost, K., Burton, R. P. D., & Bulycheva, M. (1998). Mental health insurance in the 1990s: Are employers offering less to more? Health Affairs, 17, 201–208.
Jones, H. W., Jr., & Allen, B. D. (2009). Strategies for designing an efficient insurance fertility benefit: A 21st century approach. Fertility and Sterility, 91, 2295–2297.
Kaestner, R., & Simon, K. I. (2002). Labor market consequences of state health insurance regulation. Industrial and Labor Relations Review, 56, 136–159.
Liu, Z., Dow, W. H., & Norton, E. C. (2004). Effect of drive-through delivery laws on postpartum length of stay and hospital charges. Journal of Health Economics, 23, 129–155.
Martin, J. A., Hamilton, B. E., Sutton, P. D., Ventura, S. J., Menacker, F., & Kirmeyer, S. (2006). Births: Final data for 2004 (National Vital Statistics Reports 55(1)). Hyattsville, MD: National Center for Health Statistics.
Mathews, T. J., & Hamilton, B. E. (2002). Mean age of mother: 1970–2000 (National Vital Statistics Reports 51(1)). Hyattsville, MD: National Center for Health Statistics.
Menken, J. (1985). Age and fertility: How late can you wait? Demography, 22, 469–483.
Miller, A. R. (2011). The effects of motherhood timing on career path. Journal of Population Economics, 24, 1071–1100.
Mookim, P. G., Ellis, R. P., & Kahn-Lang, A. (2008). Infertility treatment, ART and IUI procedures and delivery outcomes: How important is selection? Unpublished manuscript, Department of Economics, Boston University, Boston, MA.
Neumann, P. J., Gharib, S. D., & Weinstein, M. C. (1994). The cost of a successful delivery with in vitro fertilization. New England Journal of Medicine, 331, 239–243.
New York Times. (2001, September 1). Insurers offering pregnancy benefits now must cover fertility. Retrieved from http://www.nytimes.com/2001/09/01/nyregion/insurers-offering-pregnancy-benefits-now-must-cover-fertility.html
Nyboe Andersen, A., Goosens, V., Ferraretti, A. P., Bhattacharya, S., Felberbaum, R., de Mouzon, J., & Nygren, K. G. (2008). Assisted reproductive technology in Europe, 2004: Results generated from European registers by ESHRE. Human Reproduction, 23, 756–771.
Oyer, P. (2008). Salary or benefits? Research in Labor Economics, 28, 429–467.
Pacula, R. L., & Sturm, R. (2000). Mental health parity legislation: Much ado about nothing. Health Services Research, 35, 263–275.
Practice Committee of the American Society of Reproductive Medicine. (2008). The role of tubal reconstructive surgery in the era of assisted reproductive technologies. Fertility and Sterility, 90(Suppl. 3), S250–S253.
RESOLVE. (2003). Insurance coverage of infertility treatments. Bethesda MD: RESOLVE: The National Infertility Association.
Rothschild, M., & Stiglitz, J. E. (1976). Equilibrium in competitive insurance markets: An essay on the economics of imperfect information. Quarterly Journal of Economics, 90, 629–649.
Schmidt, L. (2005). Effects of infertility insurance mandates on fertility. Unpublished manuscript, Department of Economics, Williams College, Williamstown, MA.
Schmidt, L. (2007). Effects of infertility insurance mandates on fertility. Journal of Health Economics, 26, 431–446.
Stephen, E. H., & Chandra, A. (2000). Use of infertility services in the United States: 1995. Family Planning Perspectives, 32, 132–137.
Weinstein, M., Wood, J. W., Stoto, M. A., & Greenfield, D. D. (1990). Components of age-specific fecundability. Population Studies, 44, 447–467.
William M. Mercer Company. (1997). Women’s health issues: Infertility as a covered benefit.
Wright, V. C., Chang, J., Jeng, G., Chen, M., & Macaluso, M. (2007). Assisted reproductive technology surveillance—United States, 2004. MMWR Surveillance Summaries, 56(SS06), 1–22.
Wright, V. C., Schieve, L. A., Reynolds, M. A., & Jeng, G. (2003). Assisted reproductive technology surveillance—United States, 2000. MMWR Surveillance Summaries, 52(SS09), 1–16.
Acknowledgments
Bitler gratefully acknowledges financial support from the National Institute of Child Health and Human Development (NICHD) (R03 HD046485). Schmidt gratefully acknowledges financial support from NICHD (R03 HD047544). All errors or omissions are our own. We thank Tom Buchmueller, Kitt Carpenter, Stacy Dickert-Conlin, Tracy Gordon, Steven Haider, Mireille Jacobson, Darius Lakdawalla, Kenneth Land, Purvi Sevak, Kosali Simon, two anonymous referees and seminar participants at Michigan State University and the Center for Studies in Demography and Ecology at the University of Washington for helpful comments, and Chris Rogers and Anjani Chandra for their generous assistance with the NSFG data.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Materials
Below is the link to the electronic supplementary material.
ESM 1
(PDF 35 kb)
Rights and permissions
About this article
Cite this article
P. Bitler, M., Schmidt, L. Utilization of Infertility Treatments: The Effects of Insurance Mandates. Demography 49, 125–149 (2012). https://doi.org/10.1007/s13524-011-0078-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13524-011-0078-4