Abstract
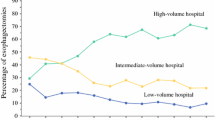
Esophageal cancer incidence is rapidly increasing in the western countries. Adenocarcinoma has recently become the most frequent subtype because of the changes in lifestyle. As observed for other types of surgery, even for esophageal surgery better results have been observed in centers with high volume of activity. Countries with formal policies of centralization, as Great Britain and The Netherlands, have got lower mortality and longer survival than those obtained before the centralization program introduction and of those countries without centralization programs. However, concerns about accessibility to high volume hospitals for lower level social strata have emerged in different countries. In Italy most of the esophagectomies for cancer are performed in very low volume centers with limited experience. High volume centers with >20 cases/year are few but, even if managing patients with more severe comorbidities have got a lower mortality and a shorter length of stay. The Aim of this paper is to identify the organizational, structural and volume requirements for accreditation of a center as an esophageal surgery center. Special attention must be given to a multidisciplinary approach involving different highly skilled specialists with the creation of a multidisciplinary team and individualized diagnostic and therapeutic pathways.
Similar content being viewed by others
References
Bollschweiller E, Wolfgarten E, Gutschow C et al (2001) Demographic variations in the rising incidence of esophageal adenocarcinoma in white males. Cancer 92:549–555
Pohl H, Welch HG (2005) The role of over diagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst 97:142–146
Kamangar F, Dores GM, Anderson WF (2006) Patterns of cancer incidence, mortality and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol 24:2137–2150
Glickmann JN (2003) Section II: pathology and pathologic staging of esophageal cancer. Semin Thorac Cardiovasc Surg 15:167–179
Eslick GD (2009) Epidemiology of esophageal cancer. Gastroenterol Clin North Am 38:17–25
Jamieson GG, Mathew G, Ludemann R et al (2004) Postoperative mortality following oesophagectomy and problems in reporting its rate. Br J Surg 91:943–947
Kohn GP, Galanko JA, Meyers MO et al (2009) National trends in esophageal surgery: are outcomes as good as we believe? J Gastrointest Surg 13:1900–1910
Ngpal K, Ahmed K, Vats A et al (2010) Is minimally invasive surgery beneficial in the management of esophageal cancer? A meta-analysis. Surg Endosc 24:1621–1629
Dantoc MM, Cox MR, Eslick GD (2012) Does minimally invasive esophagectomy (MIE) provide for comparable oncologic outcomes to open techniques? A systematic review. J Gastrointest Surg 16:486–494
Luft HS, Bunker JP, Enthoven AC (1979) Should operations be regionalized? The empirical relation between surgical volume and mortality. N Engl J Med 301:1364–1369
Markar SR, Karthikesalingam A, Thrumurthy S et al (2012) Volume-outcome relationship in surgey for esophageal malignancy: systematic review and meta-analysis 2000–2011. J Gastrointest Surg 16:1055–1063
Wouters MW, Wijnhoven BP, Karim-Kos HE et al (2007) High-volume vs low-volume for esophageal resections for cancer: the essential role of case-mix adjustment based on clinical data. Ann Surg Oncol 15:80–87
Finley CJ, Jacks L, Keshavjee S et al (2011) The effect of regionalization on outcome in esophagectomy: a canadian national study. Ann Thorac Surg 92:485–490
So YK, Jong HP, Sung GK et al (2010) Disparities in utilization of high-volume hospitals for cancer surgery: results of a Korean population-based study. Ann Surg Oncol 17:2806–2815
Munasinghe A, Markar SR, Mamidann R et al (2015) Is time to centralize high-risk cancer care in the United States? Comparison of outcome of esophagectomy between England and the United States. Ann Surg 262:79–85
Wouters MW, Karim-Kos HE, le Cessie HE et al (2009) Centralization of esophageal cancer Surgery: does it improve clinical outcome? Ann Surg Oncol 16:1789–1798
Sun M, Karakiewicz PI, Sammon JD et al (2014) Disparities in selective referral for cancer surgery: implication for the current healthcare delivery system. BMJ Open 4:e003921. doi:10.1136/bmjopen-2013-003921
Lyratzopoulos G, Barbiere JM, Gajperia C et al (2009) Trends and variation in management of oesophagogastric cancer patients: a population-based survey. BMC Health Serv Res 9:231. doi:10.1186/1472-6963-9-231
Henneman D, Dikken JL, Putter H et al (2014) Centralization of esophagectomy: how far should we go? Ann Surg Oncol 21:4068–4074
Meguid RA, Weiss ES, Chang DC et al (2009) The effect of volume on esophageal cancer resections: what constitutes acceptable resection volumes for centers of excellence? J Thorac Cardiovasc Surg 137:23–29
Palser TR, Cromwell DA, Hardwick RH et al (2009) Re-organization of oesophago-gastric cancer care in England: progress and remaining challenges. BMC Health Serv Res. 12(9):204. doi:10.1186/1472-6963-9-204
Fumagalli U, Bersani M, Russo A et al (2013) Volume and outcome after esophageal cancer surgery: the experience of the Region of Lombardy—Italy. Updates Surg 65:271–275
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The Authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Parise, P., Elmore, U., Fumagalli, U. et al. Esophageal surgery in Italy. Criteria to identify the hospital units and the tertiary referral centers entitled to perform it. Updates Surg 68, 129–133 (2016). https://doi.org/10.1007/s13304-016-0374-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-016-0374-z