Abstract
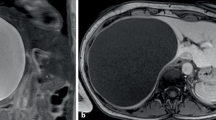
Laparoscopic liver surgery has gained widespread acceptance and nowadays it is suggested even for malignant disease. Although the benefits on short-term outcomes have been proven, data on oncological safety are still lacking. The aim of this study is to assess oncologic results after ultrasound-guided laparoscopic liver resection (LLR) or open liver resection (OLR) for colorectal metastases. 37 consecutive patients undergoing LLR between 01/2004 and 03/2014 were matched at a ratio of 1:1 with 37 OLR. Matching criteria were male sex, number and diameter of liver metastases, segment location, synchronous presentation, site and stage of primary tumor, positive lymph nodes of the primary, and concomitant extrahepatic disease. Demographic characteristics were similar among groups. Parenchymal transection time was longer in the LLR group (68 ± 38.2 SD vs 40 ± 33.7 SD, p = 0.01). Mortality was nil in LLR and OLR. Overall morbidity was significantly lower in LLR (13.5 vs 37.8 %, p = 0.02), although severe complications were similar among the two groups. Patients undergoing LLR were discharged earlier (5 ± 2.3 SD vs 8 ± 6.6 SD days, p < 0.001). The median margin width was 5 (0–40) mm in LLR vs 8 (0–25) mm in OLR, p = 0.897. R1 resection was recorded in four LLR and three OLR (p = 1). Overall recurrences were similar among groups. Eight patients with hepatic or extrahepatic recurrence among LLR underwent surgery vs four of OLR (p = 0.03). After a median follow-up of 35.7 months in LLR and 47.9 months in OLR, 3-year overall survival was 91.8 % LLR and 74.8 % OLR (p = 0.14). 3-year disease-free survival was 69.1 % LLR and 65.9 % OLR (p = 0.53). Multivariate analysis showed that postoperative complications [HR 3.42 (95 % CI 1.32–8.89)] and multiple metastases [HR 3.84 (95 % CI 1.34–10.83)] were independent predictors of worse survival (p = 0.01). Ultrasound-LLR for colorectal hepatic metastases is safe, ensuring oncologic outcomes comparable to OLR.


Similar content being viewed by others
References
Wakabayashi G, Cherqui D, Geller DA et al (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261:619–629
Lee KF, Cheung YS, Chong CN et al (2007) Laparoscopic versus open hepatectomy for liver tumors: a case control study. Hong Kong Med J 13:442–462
Lersutel M, Chrqui D, Laurent A et al (2003) Laparoscopic versus open left lateral hepatic lobectomy: a case control study. J Am Coll Surg 196:236–242
Polignano FM, Quyn AJ, de Figueiredo RS et al (2008) Laparoscopic versus open liver segmentectomy: prospective, case-matched, intention-to-treat analysis of clinical outcomes and cost effectiveness. Surg Endosc 22:2564–2570
Dagher I, Di Giuro G, Dubrez J et al (2009) Laparoscopic versus open right hepatectomy: a comparative study. Am J Surg 198:173–177
Simillis C, Constantidinides VA, Tekkis PP et al (2007) Laparoscopic versus open hepatic resections for benign and malignant neoplasm—a meta-analysis. Surgery 141:203–211
Mirnezami R, Mirnezami AH, Chandrakumaran K et al (2011) Short- and long term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB 13:295–308
Castaing D, Vibert E, Ricca L et al (2009) Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg 250:849–855
Abu Hilal M, Underwood T, Zuccaro M et al (2010) Short- and medium-term results of totally laparoscopic resection for colorectal liver metastases. Brit J Surg 97:927–933
Welsh FKS, Tekkis PP, John TG et al (2010) Open liver resection for colorectal metastases: better short and long-term outcomes in patients potentially suitable for laparoscopic liver resection. HPB 12:188–194
Viganò L, Ferrero A, Amisano M et al (2013) Comparison of laparoscopic and open intraoperative ultrasonography for staging liver tumours. Br J Surg 100:535–542
Ferrero A, Lo Tesoriere R, Russolillo N et al (2015) Ultrasound-guided laparoscopic liver resections. Surg Endosc 29:1002–1005
Viganò L, Langella S, Ferrero A et al (2013) Colorectal cancer with synchronous resectable liver metastases: monocentric management in a hepatobiliary referral center improves survival outcomes. Ann Surg Oncol 20:938–945
Buell HF, Cherqui D, Geller DA et al (2009) The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg 250(825):830
Viganò L, Jaffary SA, Ferrero A et al (2011) Liver resection without pedicle clamping: feasibility and need for “salvage clamping”. Looking for the right clamping policy. Analysis of 512 consecutive resections. J Gastrointest Surg 15:1820–1828
The Brisbane 2000 Terminology of Liver Anatomy and Resection, Terminology Committee of The International Hepato-Pancreato-Biliary Association (2000) HPB 2:333–339
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Capussotti L, Ferrero A, Viganò L et al (2006) Bile leakage and liver resection: where is the risk? Arch Surg 141:690–694
Ferrero A, Viganò L, Polastri R et al (2007) Postoperative liver dysfunction and future remnant liver: where is the limit? Results of a prospective study. World J Surg 31:1643–1651
Aldrighetti L, Pulitano C, Catena M et al (2008) A prospective evaluation of laparoscopic versus open left lateral hepatic sectionectomy. J Gastrointest Surg 12:457–462
Lee KF, Wong J, Cheung YS et al (2010) Resection margin in laparoscopic hepatectomy: a comparative study between wedge resection and anatomic left lateral sectionectomy. HPB 12:649–653
Postriganova N, Kakaryan AM, Rosok BI et al (2014) Margin status after laparoscopic resection of colorectal liver metastases: does a narrow resection margin have an influence on survival and local recurrence? HPB 16:822–829
Montalti R, Tomassini F, Laurent S et al (2014) Impact of surgical margins on overall and recurrence-free survival in parenchymal-sparing laparoscopic liver resections of colorectal metastases. Surg Endosc. doi:10.1007/s00464-014-3999-3
Gigot JF, Glineur D, Azagra JS et al (2002) Laparoscopic liver resection for malignant liver tumors. Preliminary results of a multicentric European study. Ann Surg 1:90–97
Santambrogio R, Opocher A, Ceretti P et al (2007) Impact of intraoperative ultrasonography in laparoscopic surgery. Surg End 21:181–188
Bodingbauer M, Tamandl D, Schmid K et al (2007) Size of surgical margin does not influence recurrence rates after curative liver resection for colorectal cancer liver metastases. Br J Surg 94:1133–1138
Muratore A, Ribero D, Zimmitti G et al (2010) Resection margin and recurrence-free survival after liver resection of colorectal metastases. Ann Surg Oncol 17:1324–1329
Ah J, Muirhead W, Zaitoun AM et al (2012) Comparison of liver parenchymal ablation and tissue necrosis in a cadaveric bovine model using the Harmonic Scalpel, the Liga-Sure, the Cavitron Ultrasonic Surgical Aspirator and the Aquamantys devices. HPB 14:828–832
O’Rourke N, Shaw I, Nathanson L et al (2004) Laparoscopic resection of hepatic colorectal metastases. HPB 6:230–235
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they don’t have any conflict of interest.
Ethical standard
All procedures in our paper were in accordance with the ethical standards of the Mauriziano Hosptital ethical committee as well as national research committee and with the 1964 Helsinki declaration and its later amendments.
Research involving human participants and/or animals
This article does not contain studies with human participant or animal performed by any of the authors.
Informed consent
For this type of study consent form is not required.
Rights and permissions
About this article
Cite this article
Langella, S., Russolillo, N., D’Eletto, M. et al. Oncological safety of ultrasound-guided laparoscopic liver resection for colorectal metastases: a case–control study. Updates Surg 67, 147–155 (2015). https://doi.org/10.1007/s13304-015-0325-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-015-0325-0