Abstract
Metformin is typically the first pharmacologic treatment recommended for type 2 diabetes mellitus (T2DM), but many patients do not achieve glycemic control with metformin alone and eventually require combination therapy with other agents. Canagliflozin, a sodium glucose co-transporter 2 (SGLT2) inhibitor, was assessed in a comprehensive Phase 3 clinical development program consisting of ~10,000 participants, of which ~80% were on background therapy that consisted of metformin alone or in combination with other antihyperglycemic agents (AHAs; e.g., pioglitazone, sulfonylurea, and insulin). In addition, the efficacy and safety of canagliflozin and metformin as the initial combination therapy and canagliflozin monotherapy were assessed versus metformin in treatment-naïve patients with T2DM. Across studies in patients with T2DM who were on metformin alone or in combination with other AHAs, canagliflozin 100 and 300 mg provided improvements in glycated hemoglobin for up to 104 weeks. Canagliflozin was also associated with reductions in body weight and systolic blood pressure when added to background therapy consisting of metformin alone or with other AHAs. Canagliflozin was generally well tolerated, with increased incidence of adverse events (AEs) related to the mechanism of SGLT2 inhibition (i.e., genital mycotic infections, urinary tract infections, and osmotic diuresis-related AEs). Consistent with its insulin-independent mechanism of action, canagliflozin was associated with low rates of hypoglycemia when background therapy did not include sulfonylurea or insulin. Due to its favorable efficacy and safety profile, these results suggest that adding canagliflozin to a background regimen consisting of metformin or implementing treatment with a fixed-dose regimen of canagliflozin and metformin would provide an effective and safe treatment regimen for T2DM management.
Funding: Janssen Global Services, LLC.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) is characterized by chronic hyperglycemia and is closely associated with comorbidities, including obesity, hypertension, and dyslipidemia, and an increased risk of cardiovascular disease and mortality [1–4]. The interplay of these factors can complicate T2DM management; therefore, therapeutics that control weight and blood pressure (BP) in addition to blood glucose would be beneficial [2].
The first pharmacologic intervention typically recommended for the treatment of T2DM is metformin [5–7], which works primarily by decreasing hepatic glucose production [5, 8]. Metformin may also reduce endogenous glucose production by delaying intestinal glucose absorption [8], and recent evidence suggests that metformin’s action in the gut is responsible for its glucose-lowering effect [9]. Metformin has a well-established efficacy and safety profile, is not associated with hypoglycemia or weight gain, may reduce the risk of myocardial infarction and death, and is inexpensive [5, 6, 10]. Despite these advantages, many patients are unable to control their blood glucose levels with metformin alone and require combination therapy with other antihyperglycemic agents (AHAs) [5, 11, 12]. Some of the AHAs frequently used for combination therapy have undesirable effects, such as weight gain, hypoglycemia, and decreased efficacy over time [5, 11, 12].
Sodium glucose co-transporter 2 (SGLT2) inhibitors lower the renal threshold for glucose (RTG) in patients with T2DM, thus increasing urinary glucose excretion and leading to mild osmotic diuresis and a net caloric loss [5, 13]. This mechanism is independent of insulin and complementary to those of other classes of AHAs, including metformin [5, 13]. In addition to improving glycemic control, SGLT2 inhibitors have been associated with modest weight loss and BP reductions in patients with T2DM [14]. SGLT2 inhibitors are additionally associated with improvements in measures of beta-cell function, including glucose sensitivity and insulin secretion [15–17]. Along with potentially having favorable effects on components of T2DM, the benefits of this class may also improve cardiovascular outcomes in patients with T2DM [18, 19]. Due to their favorable efficacy and tolerability profile, the American Diabetes Association recommends adding an SGLT2 inhibitor in patients whose T2DM is inadequately controlled with metformin [6], and the American Association of Clinical Endocrinologists Glycemic Control Algorithm identifies SGLT2 inhibitors as the first choice of oral medications for add-on therapy in patients inadequately controlled on metformin [7].
Canagliflozin, an SGLT2 inhibitor, is approved in many countries for the treatment of adults with T2DM [20], and a fixed-dose combination of canagliflozin and metformin, is also available for the treatment of adults with T2DM [21]. When administered as an add-on treatment to metformin, canagliflozin was associated with reductions in glycated hemoglobin (HbA1c), weight loss, and BP lowering in a broad range of patients in Phase 2 [22, 23] and Phase 3 studies [24–26]. These effects were also observed in a Phase 3 study of the initial combination therapy with canagliflozin plus metformin [27]. The benefits noted in these studies were similar to those seen in other Phase 3 studies when canagliflozin was administered to patients on a background of metformin plus pioglitazone [28], metformin plus sulfonylurea [29, 30], or metformin plus insulin [31]. This review summarizes the efficacy and safety of canagliflozin when used in combination with metformin in Phase 3 studies in patients with T2DM.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Overview of Clinical Studies of Canagliflozin in Combination with Metformin
Table 1 provides an overview of the designs and patient populations of the Phase 3 studies, in which canagliflozin was administered with metformin alone or in combination with another AHA (i.e., pioglitazone, sulfonylurea, and insulin) in patients with T2DM. Key efficacy analyses in these studies included changes from baseline in HbA1c, body weight, and systolic BP. Safety was assessed based on adverse event (AE) reports.
Two randomized, double-blind, Phase 3 studies evaluated the efficacy and safety of canagliflozin 100 and 300 mg as add-on to metformin [24–26]. A 52-week study in 1284 participants evaluated the efficacy and safety of canagliflozin versus placebo at week 26 and versus sitagliptin 100 mg at week 52 (ClinicalTrials.gov Identifier, NCT01106677) [24]. Safety analyses included participants who received canagliflozin 100 or 300 mg or sitagliptin 100 mg over 52 weeks and those who switched from placebo to sitagliptin after 26 weeks (placebo/sitagliptin group). The second study (NCT00968812) evaluated canagliflozin 100 and 300 mg versus glimepiride in 1450 participants at 52 weeks [25] and 104 weeks [26]. A separate randomized, double-blind, Phase 3 study evaluated the efficacy and safety of the initial combination therapy with canagliflozin 100 or 300 mg plus metformin versus metformin alone in 1186 drug-naïve patients over 26 weeks (NCT01809327) [27]. This study also evaluated the efficacy and safety of canagliflozin 100 and 300 mg monotherapy versus metformin [27].
A randomized, double-blind, Phase 3 study evaluated canagliflozin 100 and 300 mg as add-on to metformin plus pioglitazone in 342 patients over 52 weeks (NCT01106690) [28]. Patients assigned to placebo were switched to sitagliptin 100 mg after 26 weeks. Efficacy comparisons were made versus placebo at week 26 and versus sitagliptin 100 mg at week 52. Safety data at week 52 included patients in the placebo group who were switched to sitagliptin at week 26.
Two randomized, double-blind, Phase 3 studies evaluated the efficacy and safety of canagliflozin as add-on to metformin plus sulfonylurea. A placebo-controlled study in 469 patients evaluated the efficacy and safety of canagliflozin 100 and 300 mg as add-on to metformin plus sulfonylurea over 52 weeks (NCT01106625) [29]. A separate head-to-head study evaluated the efficacy and safety of canagliflozin 300 mg versus sitagliptin 100 mg as add-on to metformin plus sulfonylurea over 52 weeks (NCT01137812) [30].
An 18-week, randomized, double-blind, placebo-controlled study of canagliflozin 100 and 300 mg as add-on therapy to metformin or metformin plus sulfonylurea was conducted in Asian patients with T2DM in China, Malaysia, and Vietnam (NCT01381900) [32]. Of 676 participants, 330 were receiving metformin monotherapy (metformin stratum) and 346 were receiving metformin plus sulfonylurea (metformin plus sulfonylurea stratum) at baseline.
An 18-week, prespecified substudy of the ongoing CANagliflozin cardioVascular Assessment Study (CANVAS; NCT01032629) evaluated the efficacy and safety of canagliflozin 100 and 300 mg compared with placebo in 432 patients with T2DM and a history or high risk of cardiovascular disease whose background therapy consisted of metformin plus insulin ≥30 IU/day (basal and/or bolus) [31].
Glycemic Efficacy
Combination with Metformin Alone
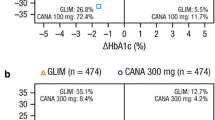
Figure 1 presents the least squares (LS) mean changes in HbA1c in the core periods of Phase 3 studies of canagliflozin added to metformin alone or in combination with other AHAs and in the initial combination therapy study. In the study of canagliflozin versus placebo/sitagliptin, canagliflozin 100 and 300 mg significantly lowered HbA1c versus placebo at week 26 (p < 0.001) [24]. At week 52, canagliflozin 100 mg demonstrated noninferiority and canagliflozin 300 mg demonstrated superiority in lowering HbA1c versus sitagliptin [24].
Changes from baseline in HbA1c in Phase 3 studies of canagliflozin in combination with metformin ± other AHAs [24–32]. a p < 0.001 versus PBO; b p = 0.001 versus MET; c p = 0.001 versus CANA 100 mg; d p = 0.001 versus CANA 300 mg; e Noninferiority p = 0.001 versus MET. AHA antihyperglycemic agent, CANA canagliflozin, GLIM glimepiride, HbA1c glycated hemoglobin, LS least squares, MET metformin, PBO placebo, PIO pioglitazone, SE standard error, SITA sitagliptin, SU sulfonylurea
At week 52, canagliflozin 100 mg demonstrated noninferiority and canagliflozin 300 mg demonstrated superiority in lowering HbA1c in the head-to-head study versus glimepiride [25]. At week 104, HbA1c reductions were −0.65%, −0.74%, and −0.55% with canagliflozin 100 and 300 mg and glimepiride, respectively [26].
In the metformin stratum of the study in Asian patients, HbA1c reductions from baseline at week 18 were significantly larger with canagliflozin 100 and 300 mg compared with placebo (p < 0.001) [32].
In the initial combination therapy study, canagliflozin 100 mg/metformin and canagliflozin 300 mg/metformin significantly lowered HbA1c versus metformin monotherapy at week 26 (p = 0.001) [27].
Combination with Metformin Plus Other AHAs
In the placebo-controlled add-on to metformin plus pioglitazone study, significant reductions in HbA1c were seen with canagliflozin 100 and 300 mg versus placebo at week 26 (p < 0.001) [28]. At week 52, reductions in HbA1c with canagliflozin 100 and 300 mg were −0.92% and −1.03%, respectively.
In the placebo-controlled add-on to metformin plus sulfonylurea study, canagliflozin 100 and 300 mg significantly lowered HbA1c versus placebo over 26 weeks (p < 0.001) [29]. Reductions in HbA1c with canagliflozin 100 and 300 mg versus placebo were sustained over 52 weeks (−0.74%, −0.96%, and 0.01%, respectively). In the head-to-head study of canagliflozin as add-on to metformin plus sulfonylurea, canagliflozin 300 mg demonstrated superiority in HbA1c lowering versus sitagliptin 100 mg over 52 weeks [30]. Among patients in the metformin plus sulfonylurea stratum of the study in Asian patients, reductions in HbA1c were significantly larger with canagliflozin 100 and 300 mg compared with placebo at week 18 (p < 0.001) [32].
In the subset of CANVAS patients whose background therapy consisted of metformin plus insulin, canagliflozin 100 and 300 mg significantly lowered HbA1c compared with placebo over 18 weeks (p < 0.001) [31].
Body Weight Reductions
Combination with Metformin Alone
Figure 2 depicts LS mean percent changes in body weight in the core periods of Phase 3 studies of canagliflozin in combination with metformin. In the study versus placebo/sitagliptin, canagliflozin provided significant body weight reductions at week 26 compared with placebo (p < 0.001) [24]; reductions were sustained at week 52 (p < 0.001) [24].
Changes from baseline in body weight in Phase 3 studies of canagliflozin in combination with metformin ± other AHAs [24–32]. a Absolute changes from baseline in kg are shown in parentheses; b p < 0.001 versus PBO; c p < 0.001 versus SITA 100 mg; d p < 0.0001 versus GLIM; e p = 0.001 versus MET; f p = 0.016 versus MET; g p = 0.002 versus MET. AHA antihyperglycemic agent, CANA canagliflozin, GLIM glimepiride, LS least squares, MET metformin, PBO placebo, PIO pioglitazone, SE standard error, SITA sitagliptin, SU sulfonylurea
In the active-controlled study versus glimepiride, significant body weight reductions were seen with canagliflozin 100 and 300 mg compared with an increase with glimepiride at week 52 (p < 0.0001) [25]. Body weight reductions with canagliflozin 100 and 300 mg versus glimepiride were sustained at week 104; changes from baseline were −4.1%, −4.2%, and 0.9% (−3.6, −3.6, and 0.8 kg), respectively [26].
In the metformin stratum of the study in Asian patients, greater reductions in body weight were seen with canagliflozin 100 and 300 mg compared with placebo at week 18 (p < 0.001) [32].
At week 26 in the initial combination therapy study, significantly greater weight loss was seen with canagliflozin 100 mg/metformin and canagliflozin 300 mg/metformin than with metformin alone (p = 0.001) [27].
Combination with Metformin Plus Other AHAs
Significant reductions in body weight were seen with canagliflozin 100 and 300 mg versus placebo as add-on to metformin plus pioglitazone at week 26 (p < 0.001) [28]. At week 52, body weight reductions with canagliflozin 100 and 300 mg were sustained (−2.7% and −3.7% [−2.5 and −3.6 kg], respectively).
In the placebo-controlled add-on to metformin plus sulfonylurea study, canagliflozin 100 and 300 mg significantly lowered body weight versus placebo over 26 weeks (p < 0.001) [29]. At week 52, reductions in body weight were −2.2%, −3.2%, −0.9% (−2.0, −3.1, and −1.0 kg) with canagliflozin 100 and 300 mg and placebo, respectively. In the head-to-head study of canagliflozin as add-on to metformin plus sulfonylurea, canagliflozin 300 mg significantly lowered body weight versus sitagliptin 100 mg over 52 weeks (p < 0.001) [30]. Among Asian patients in the metformin plus sulfonylurea stratum, significant reductions in body weight were seen with canagliflozin 100 and 300 mg compared with placebo at week 18 (p < 0.001) [32].
In the subset of CANVAS patients on metformin plus insulin, canagliflozin 100 and 300 mg significantly lowered body weight compared with placebo over 18 weeks (p < 0.001) [31].
Changes in Systolic BP
Combination with Metformin Alone
Figure 3 depicts LS mean changes in systolic BP in the core periods of Phase 3 studies of canagliflozin in combination with metformin. In the study of canagliflozin versus placebo/sitagliptin, significant reductions in systolic BP were seen with canagliflozin 100 and 300 mg versus placebo at week 26 (p < 0.001) [24]. Significant systolic BP reductions were also seen at week 52 with canagliflozin 100 and 300 mg compared with sitagliptin 100 mg (p < 0.001).
Changes from baseline in systolic BP in Phase 3 studies of canagliflozin in combination with metformin ± other AHAs [24–32]. a p < 0.001 versus PBO; b p < 0.001 versus SITA 100 mg; c p = NS versus MET; d p < 0.01 versus PBO; e p < 0.025 versus PBO. AHA antihyperglycemic agent, BP blood pressure, CANA canagliflozin, GLIM glimepiride, LS least squares, MET metformin, NS not significant, PBO placebo, PIO pioglitazone, SE standard error, SITA sitagliptin, SU sulfonylurea
In the study of canagliflozin versus glimepiride, canagliflozin 100 and 300 mg were associated with reductions in systolic BP versus glimepiride at week 52 [25] and week 104 (−2.0, −3.1, and 1.7 mmHg, respectively) [26].
In Asian patients, reductions in systolic BP were numerically greater with canagliflozin 100 and 300 mg compared with placebo in the metformin stratum at week 18 [32].
At week 26 in the initial combination therapy study, canagliflozin 100 mg/metformin and canagliflozin 300 mg/metformin were associated with numerically larger reductions in systolic BP compared with metformin monotherapy [27].
Combination with Metformin Plus Other AHAs
Significant reductions in systolic BP were seen with canagliflozin 100 and 300 mg versus placebo as add-on to metformin plus pioglitazone at week 26 (p < 0.01 and p < 0.025, respectively) [28]. At week 52, reductions in systolic BP were −3.4 and −3.7 mmHg with canagliflozin 100 and 300 mg, respectively.
In the placebo-controlled add-on to metformin plus sulfonylurea study, canagliflozin 100 and 300 mg provided numerical reductions in systolic BP versus placebo over 26 weeks [29]. At week 52, changes in systolic BP were −3.7, −2.9, and 0.1 mmHg with canagliflozin 100 and 300 mg and placebo, respectively. In the head-to-head study of canagliflozin as add-on to metformin plus sulfonylurea, canagliflozin 300 mg significantly lowered systolic BP versus sitagliptin 100 mg over 52 weeks (p < 0.001) [30]. In the metformin plus sulfonylurea stratum of the study in Asian patients, larger changes in systolic BP were seen with canagliflozin 100 and 300 mg compared with placebo at week 18 [32].
In the subset of CANVAS patients on metformin plus insulin, reductions in systolic BP were seen with canagliflozin 100 and 300 mg compared with placebo at week 18 (p < 0.001 for canagliflozin 300 mg versus placebo) [31].
Efficacy of Canagliflozin Monotherapy Versus Metformin
The initial combination study also evaluated the efficacy and safety of canagliflozin 100 and 300 mg monotherapy versus metformin in treatment-naïve patients with T2DM [27]. Canagliflozin 100 and 300 mg demonstrated noninferiority in lowering HbA1c versus metformin at week 26 (noninferiority p = 0.001; Fig. 1). Body weight reductions were significantly greater with canagliflozin 100 and 300 mg versus metformin (p = 0.016 and p = 0.002, respectively; Fig. 2). Reductions in systolic BP were also observed with canagliflozin 100 and 300 mg compared with metformin (Fig. 3).
Safety of Canagliflozin in Combination with Metformin
Overall Safety and Selected AEs
Canagliflozin was generally well tolerated, with similar safety and tolerability profiles seen across studies in combination with metformin [24–32]. Table 2 summarizes safety data in Phase 3 studies of canagliflozin in combination with metformin alone, and Table 3 summarizes safety data in the studies of canagliflozin in combination with metformin and other AHAs. In addition to providing the overall incidence of AEs, the tables show the incidence of selected AEs related to SGLT2 inhibition, including urinary tract infections, genital mycotic infections, osmotic diuresis-related AEs, and volume depletion-related AEs. Overall, the frequency of AEs leading to discontinuation and serious AEs was generally low with canagliflozin versus comparators [24–32]. The incidence of genital mycotic infections and osmotic diuresis-related AEs was generally higher with canagliflozin versus comparators. Rates of volume depletion-related AEs, including postural dizziness and orthostatic hypotension, were low across groups in each study.
Gastrointestinal-related AEs, such as diarrhea, nausea, and vomiting, which are commonly associated with metformin, were generally similar across groups in each study [24–32]. At week 26 in the initial combination therapy study, the incidence of gastrointestinal-related AEs was 4.6%, 4.6%, and 4.2% with canagliflozin 100 mg/metformin, canagliflozin 300 mg/metformin, and metformin, respectively; rates were 1.7% with canagliflozin 100 mg and 2.9% with canagliflozin 300 mg [27].
Diabetic ketoacidosis was rare in the canagliflozin clinical development program [33]. No serious AEs of diabetic ketoacidosis were seen with canagliflozin when it was added to background therapy consisting of metformin alone or in combination with pioglitazone [33]. There was one serious AE of ketoacidosis with canagliflozin 300 mg in the initial combination therapy study [33]. This event occurred in a 62-year-old man on the 18th day of treatment. Confounding factors were: an abscessed boil of the anterior abdominal wall that required dissection and antibiotics; chronic pancreatitis, which was detected by abdominal ultrasound; and heart failure class II and treatment with indapamide. There was one serious AE of ketoacidosis with canagliflozin 100 mg in the placebo-controlled add-on to metformin plus sulfonylurea study [33]. The event occurred in a 47-year-old woman who had nearly 50-kg weight loss over 2 years and was subsequently diagnosed with type 1 diabetes. There were no serious AEs of diabetic ketoacidosis in the subset of patients from the CANVAS trial who were on metformin plus insulin during the 18-week treatment period.
An interim safety analysis of the overall CANVAS study identified an increased risk for lower limb amputation with canagliflozin (7.3, 5.4, and 3.0 per 1000 patient-years with canagliflozin 100 and 300 mg and placebo, respectively) [34]. This safety signal was not observed in a pooled analysis of 12 completed Phase 3 and Phase 4 studies representing a broad patient population on background metformin or other AHAs (data on file), or in an analysis of the CANVAS-R (renal outcomes; NCT01989754) study. In pooled Phase 3 studies, an increased risk for fracture, primarily in the upper and lower extremities, was observed with canagliflozin, which was driven by a higher incidence in patients from the CANVAS study [35]. Additional data regarding the risk for amputation and fracture with canagliflozin will be available upon completion of the CANVAS and CANVAS-R studies in 2017.
Hypoglycemia
As an SGLT2 inhibitor, canagliflozin reduces reabsorption of filtered glucose and lowers RTG, thereby increasing urinary glucose excretion and lowering elevated plasma glucose concentrations in patients with T2DM [20, 36]. The risk of hypoglycemia with canagliflozin is expected to be low because RTG typically remains above the threshold for hypoglycemia (~3.9 mmol/L) in patients with T2DM, and very little urinary glucose excretion occurs when plasma glucose levels are below RTG [20].
In Phase 3 studies of canagliflozin, documented hypoglycemia episodes were defined as biochemically documented episodes (concurrent fingerstick glucose or plasma glucose ≤3.9 mmol/L with or without symptoms) and severe episodes (requiring the assistance of another individual or resulting in seizure or loss of consciousness) [24–32]. In general, patients who were not on background therapy that included sulfonylurea had a low incidence of hypoglycemia with canagliflozin 100 and 300 mg that was generally slightly higher versus placebo and active comparators. The incidence of severe hypoglycemia episodes was low across groups in patients who were not on background sulfonylurea or insulin (Tables 2 and 3).
Of note, in the study of canagliflozin versus glimepiride, the incidence of documented hypoglycemia episodes at week 52 was significantly lower for canagliflozin 100 and 300 mg versus glimepiride (5.6%, 4.9%, and 34.2%, respectively; p < 0.0001) [25]. The frequency of severe hypoglycemia was also lower with canagliflozin 100 mg (two patients [0.4%]) and 300 mg (three patients [0.6%]) than with glimepiride (15 patients [3.1%]). At week 104, the proportion of patients with documented hypoglycemia episodes remained lower with canagliflozin 100 and 300 mg than with glimepiride (6.8%, 8.2%, and 40.9%, respectively) [26]. No additional severe hypoglycemia events with canagliflozin were reported after week 52.
As add-on to metformin versus placebo/sitagliptin, the incidence of documented hypoglycemia episodes at week 52 was higher with both canagliflozin doses compared with sitagliptin 100 mg and with placebo/sitagliptin [24]. The reason for the higher incidence of documented episodes of hypoglycemia with canagliflozin versus sitagliptin and placebo/sitagliptin in this study is unknown, although the greater HbA1c lowering seen with canagliflozin may have contributed to this difference. However, as add-on to metformin plus sulfonylurea, the incidence of hypoglycemia with canagliflozin 300 mg was similar to sitagliptin (43.2% and 40.7%, respectively), despite a nearly 0.4% larger reduction in HbA1c with canagliflozin [30].
Fasting Plasma Lipids and Laboratory Parameters
Across studies, canagliflozin was generally associated with reductions in triglycerides and increases in high-density lipoprotein cholesterol and low-density lipoprotein cholesterol [24–32]. In addition, no clinically meaningful changes in most laboratory parameters, including alanine aminotransferase, aspartate aminotransferase, bilirubin, blood urea nitrogen, creatinine, urate, and hemoglobin, were seen with canagliflozin across studies [24–32]. Treatment with canagliflozin in combination with metformin was associated with a transient reduction in estimated glomerular filtration rate (eGFR) that attenuated over time [24–32]. In the 104-week study as add-on to metformin versus glimepiride [26], canagliflozin was associated with a slower rate in decline in eGFR compared with glimepiride, suggesting a potential renoprotective effect for canagliflozin [37]. In addition, canagliflozin provided reductions in albumin-to-creatinine ratio (ACR) in the studies where ACR was assessed [25, 26, 37–40]. The ongoing Canagliflozin and Renal Events in Diabetes With Established Nephropathy Clinical Evaluation (CREDENCE; NCT02065791) study will provide further insight into the renal effects of canagliflozin in patients with T2DM and renal impairment.
Conclusion
Improving glycemic control is the cornerstone of diabetes management, as improvements in blood glucose levels can decrease the risk of diabetes-related complications. SGLT2 inhibitors may be suitable alternative therapeutic agents for combination therapy with metformin due to their favorable glycemic efficacy and added benefits of weight loss and BP reduction. Treatment with canagliflozin in combination with metformin was associated with reductions in HbA1c, body weight, and systolic BP versus placebo and active comparators across Phase 3 studies of up to 104 weeks in duration. Canagliflozin was generally well tolerated, with an increased incidence of AEs related to the mechanism of SGLT2 inhibition and low rates of hypoglycemia. As genital mycotic infections were more common in male and female patients with a prior history of infections and in uncircumcised males, awareness of these potential AEs with canagliflozin is important for these patient populations. Patients susceptible to the volume depletion effects of canagliflozin (i.e., older patients, patients with moderate renal impairment, and those taking loop diuretics) should be monitored while on canagliflozin treatment. The favorable efficacy and safety profile suggest that adding canagliflozin to a background treatment regimen consisting of metformin alone or in combination with other AHAs, or implementing treatment with a fixed-dose combination of canagliflozin and metformin would provide an effective and safe alternative treatment regimen for T2DM management.
References
Defronzo RA. Pathogenesis of type 2 diabetes mellitus. Med Clin North Am. 2004;88:787–835, ix.
Niswender K. Diabetes and obesity: therapeutic targeting and risk reduction—a complex interplay. Diabetes Obes Metab. 2010;12:267–87.
Sarwar N, Gao P, Seshasai SR, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–22.
Di Angelantonio E, Kaptoge S, Wormser D, et al. Association of cardiometabolic multimorbidity with mortality. JAMA. 2015;314:52–60.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–9.
American Diabetes Association. Standards of medical care in diabetes—2016. Diabetes Care. 2016;39:S1–108.
Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2016 executive summary. Endocr Pract. 2016;22:84–113.
Ferrannini E. The target of metformin in type 2 diabetes. N Engl J Med. 2014;371:1547–8.
Buse JB, Defronzo RA, Rosenstock J, et al. The primary glucose-lowering effect of metformin resides in the gut, not the circulation: results from short-term pharmacokinetic and 12-week dose-ranging studies. Diabetes Care. 2016;39:198–205.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89.
Cook MN, Girman CJ, Stein PP, Alexander CM, Holman RR. Glycemic control continues to deteriorate after sulfonylureas are added to metformin among patients with type 2 diabetes. Diabetes Care. 2005;28:995–1000.
Cook MN, Girman CJ, Stein PP, Alexander CM. Initial monotherapy with either metformin or sulphonylureas often fails to achieve or maintain current glycaemic goals in patients with type 2 diabetes in UK primary care. Diabet Med. 2007;24:350–8.
Chao EC, Henry RR. SGLT2 inhibition—a novel strategy for diabetes treatment. Nat Rev Drug Discov. 2010;9:551–9.
Mudaliar S, Polidori D, Zambrowicz B, Henry RR. Sodium-glucose cotransporter inhibitors: effects on renal and intestinal glucose transport: from bench to bedside. Diabetes Care. 2015;38:2344–53.
Polidori D, Mari A, Ferrannini E. Canagliflozin, a sodium glucose co-transporter 2 inhibitor, improves model-based indices of beta cell function in patients with type 2 diabetes. Diabetologia. 2014;57:891–901.
Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124:509–14.
Ferrannini E, Muscelli E, Frascerra S, et al. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest. 2014;124:499–508.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Wu JH, Foote C, Blomster J, et al. Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular events, death, and major safety outcomes in adults with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2016;4:411–9.
Rosenthal N, Meininger G, Ways K, et al. Canagliflozin: a sodium glucose co-transporter 2 inhibitor for the treatment of type 2 diabetes mellitus. Ann N Y Acad Sci. 2015;1358:28–43.
INVOKAMET® (canagliflozin and metformin hydrochloride) tablets for oral use [package insert]. Titusville: Janssen Pharmaceuticals, Inc; Revised December 2015.
Rosenstock J, Aggarwal N, Polidori D, et al. Dose-ranging effects of canagliflozin, a sodium-glucose cotransporter 2 inhibitor, as add-on to metformin in subjects with type 2 diabetes. Diabetes Care. 2012;35:1232–8.
Qiu R, Capuano G, Meininger G. Efficacy and safety of twice-daily treatment with canagliflozin, a sodium glucose co-transporter 2 inhibitor, added on to metformin monotherapy in patients with type 2 diabetes mellitus. J Clin Transl Endocrinol. 2014;1:54–60.
Lavalle-González FJ, Januszewicz A, Davidson J, et al. Efficacy and safety of canagliflozin compared with placebo and sitagliptin in patients with type 2 diabetes on background metformin monotherapy: a randomised trial. Diabetologia. 2013;56:2582–92.
Cefalu WT, Leiter LA, Yoon KH, et al. Efficacy and safety of canagliflozin versus glimepiride in patients with type 2 diabetes inadequately controlled with metformin (CANTATA-SU): 52 week results from a randomised, double-blind, phase 3 non-inferiority trial. Lancet. 2013;382:941–50.
Leiter LA, Yoon KH, Arias P, et al. Canagliflozin provides durable glycemic improvements and body weight reduction over 104 weeks versus glimepiride in patients with type 2 diabetes on metformin: a randomized, double-blind, phase 3 study. Diabetes Care. 2015;38:355–64.
Rosenstock J, Chuck L, Gonzalez-Ortiz M, Merton K, Craig J, Capuano G. Initial combination therapy with canagliflozin plus metformin versus each component as monotherapy in drug-naive type 2 diabetes. Diabetes Care. 2016;39:353–62.
Forst T, Guthrie R, Goldenberg R, et al. Efficacy and safety of canagliflozin over 52 weeks in patients with type 2 diabetes on background metformin and pioglitazone. Diabetes Obes Metab. 2014;16:467–77.
Wilding JP, Charpentier G, Hollander P, et al. Efficacy and safety of canagliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sulphonylurea: a randomised trial. Int J Clin Pract. 2013;67:1267–82.
Schernthaner G, Gross JL, Rosenstock J, et al. Canagliflozin compared with sitagliptin for patients with type 2 diabetes who do not have adequate glycemic control with metformin plus sulfonylurea: a 52-week, randomized trial. Diabetes Care. 2013;36:2508–15.
Rosenstock J, Matthews DR, Desai M, Capuano G, Meininger G, Canovatchel W. Impact of canagliflozin added-on to insulin and metformin in type 2 diabetes: a substudy of the CANVAS trial. Poster presented at: 75th Scientific Sessions of the American Diabetes Association (ADA); June 5–9, 2015; Boston, MA.
Ji L, Han P, Liu Y, et al. Canagliflozin in Asian patients with type 2 diabetes on metformin alone or metformin in combination with sulphonylurea. Diabetes Obes Metab. 2015;17:23–31.
Erondu N, Desai M, Ways K, Meininger G. Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care. 2015;38:1680–6.
US Food and Drug Administration. FDA drug safety communication: interim clinical trial results find increased risk of leg and foot amputations, mostly affecting the toes, with the diabetes medicine canagliflozin (Invokana, Invokamet); FDA to investigate. http://www.fda.gov/Drugs/DrugSafety/ucm500965.htm. Accessed 22 July 2016.
Watts NB, Bilezikian JP, Usiskin K, et al. Effects of canagliflozin on fracture risk in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab. 2016;101:157–66.
Wilding JP. The role of the kidneys in glucose homeostasis in type 2 diabetes: clinical implications and therapeutic significance through sodium glucose co-transporter 2 inhibitors. Metabolism. 2014;63:1228–37.
Heerspink HJ, Desai M, Jardine M, Balis D, Meininger G, Perkovic V. Canagliflozin slows progression of renal function decline independently of glycemic effects. J Am Soc Nephrol. 2016. doi:10.1681/ASN.2016030278.
Neal B, Perkovic V, de Zeeuw D, et al. Efficacy and safety of canagliflozin, an inhibitor of sodium glucose co-transporter 2, when used in conjunction with insulin therapy in patients with type 2 diabetes. Diabetes Care. 2015;38:403–11.
Yale JF, Bakris G, Cariou B, et al. Efficacy and safety of canagliflozin in subjects with type 2 diabetes and chronic kidney disease. Diabetes Obes Metab. 2013;15:463–73.
Yale JF, Bakris G, Cariou B, et al. Efficacy and safety of canagliflozin over 52 weeks in patients with type 2 diabetes mellitus and chronic kidney disease. Diabetes Obes Metab. 2014;16:1016–27.
Acknowledgments
Sponsorship and article processing charges for this study were funded by Janssen Global Services, LLC. Editorial assistance was provided to the authors by Kimberly Dittmar, PhD, of MedErgy, and was funded by Janssen Global Services, LLC. The authors were involved at all stages of manuscript development and maintained full control over the scientific content. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Disclosures
Rong Qiu is a full-time employee of Janssen Research & Development, LLC. Dainius Balis is a full-time employee of Janssen Research & Development, LLC. George Capuano is a full-time employee of Janssen Research & Development, LLC. John Xie is a full-time employee of Janssen Research & Development, LLC. Gary Meininger is a full-time employee of Janssen Research & Development, LLC.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/44E6F060333FA026.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Qiu, R., Balis, D., Capuano, G. et al. Canagliflozin: Efficacy and Safety in Combination with Metformin Alone or with Other Antihyperglycemic Agents in Type 2 Diabetes. Diabetes Ther 7, 659–678 (2016). https://doi.org/10.1007/s13300-016-0201-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-016-0201-z