Abstract
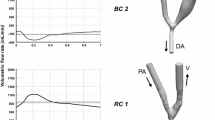
During hemodialysis, arteriovenous (AV) grafts tends to result in intimal hyperplasia (IH) at the venous anastomosis which leads to graft failure. It is well documented that hemodynamic factors have been implicated in IH, as well as pathogenesis of graft stenosis. In this paper, we investigate the flow rate and angle of injection of a venous needle on damaging the hemodialysis graft. Such damage is mainly caused by hemodynamics rather than the actual physical puncture of the needle. By computational fluid dynamic analysis of flow through the AV grafts, we demonstrate that slower flow rate of the needle preserve a larger region of low wall shear stress (WSS). High needle flow angle and fast flow rate tends to induce high shearing of blood against the graft wall, and therefore resulting in a concentrated region of high WSS. Despite that, the increased flow rate causes more significant change to wall shear stress gradient than the flow angle. Obviously, it is important to optimize the injection rate since a high angle can reduce the size of the injection puncture and have smaller injury for the vessel walls; but a slower injection rate may delay hemodialysis. Therefore, the ideal angle and flow rate of needle is sought in this study.








Similar content being viewed by others
References
Joyce AT, Iacoviello JM, Nag S, Sajjan S, Jilinskaia E, Throop D, Pedan A, Ollendorf DA, Alexander CM (2004) End-stage renal disease-associated managed care costs among patients with and without diabetes. Diabetes Care 27(12):2829–2835. doi:10.2337/diacare.27.12.2829
Pisoni RL, Young EW, Dykstra DM, Greenwood RN, Hecking E, Gillespie B, Wolfe RA, Goodkin DA, Held PJ (2002) Vascular access use in Europe and the United States: results from the DOPPS. Kidney Int 61(1):305–316
Mangrum A, Okusa MD (2007) Mechanisms underlying vascular access dysfunction. Drug Discov Today Dis Mech 4(3):147–151
Moncada S, Higgs EA (2006) The discovery of nitric oxide and its role in vascular biology. Br J Pharmacol 147(S1):S193–S201
Dimmeler S, Fleming I, Fisslthaler B, Hermann C, Busse R, Zeiher AM (1999) Activation of nitric oxide synthase in endothelial cells by Akt-dependent phosphorylation. Nature 399(6736):601–605
Belhassen L, Pelle G, Sediame S, Bachir D, Carville C, Bucherer C, Lacombe C, Galacteros F, Adnot S (2001) Endothelial dysfunction in patients with sickle cell disease is related to selective impairment of shear stress-mediated vasodilation. Blood 97(6):1584–1589. doi:10.1182/blood.V97.6.1584
Fulker D, Kang M, Simmons A, Barber T (2013) The flow field near a venous needle in hemodialysis: a computational study. Hemodial Int 17(4):602–611. doi:10.1111/hdi.12029
Huynh TN, Chacko BK, Teng X, Brott BC, Allon M, Kelpke SS, Thompson JA, Patel RP, Anayiotos AS (2007) Effects of venous needle turbulence during ex vivo hemodialysis on endothelial morphology and nitric oxide formation. J Biomech 40(10):2158–2166. doi:10.1016/j.jbiomech.2006.10.028
Unnikrishnan S, Huynh TN, Brott BC, Ito Y, Cheng CH, Shih AM, Allon M, Anayiotos AS (2005) Turbulent flow evaluation of the venous needle during hemodialysis. J Biomech Eng 127(7):1141–1146. doi:10.1115/1.2112927
Davies PF, Remuzzi A, Gordon EJ, Dewey CF, Gimbrone MA (1986) Turbulent fluid shear-stress induces vascular endothelial-cell turnover invitro. Proc Natl Acad Sci USA 83(7):2114–2117. doi:10.1073/pnas.83.7.2114
Wu J, Liu G, Huang W, Ghista DN, Wong KKL (2015) Transient blood flow in elastic coronary arteries with varying degrees of stenosis and dilatations: CFD modelling and parametric study. Comput Methods Biomech Biomed Eng 18(16):1835–1845. doi:10.1080/10255842.2014.976812
O’Callaghan S, Walsh M, McGloughlin T (2006) Numerical modelling of Newtonian and non-Newtonian representation of blood in a distal end-to-side vascular bypass graft anastomosis. Med Eng Phys 28(1):70–74. doi:10.1016/j.medengphy.2005.04.001
Yilmaz F, Gundogdu MY (2008) A critical review on blood flow in large arteries; relevance to blood rheology, viscosity models, and physiologic conditions. Korea Aust Rheol J 20(4):197–211
Lee S-W, Smith DS, Loth F, Fischer PF, Bassiouny HS (2007) Importance of flow division on transition to turbulence within an arteriovenous graft. J Biomech 40(5):981–992. doi:10.1016/j.jbiomech.2006.03.024
Van Tricht I, De Wachter D, Tordoir J, Vanhercke D, Verdonck P (2005) Experimental analysis of the hemodynamics in punctured vascular access grafts. Asaio J 51(4):352–359. doi:10.1097/01.mat.0000169126.91756.1d
Wong KK, Thavornpattanapong P, Cheung SC, Tu J (2013) Numerical stability of partitioned approach in fluid-structure interaction for a deformable thin-walled vessel. Comput Math Methods Med 2013(3):437–452
Wong KK, Thavornpattanapong P, Cheung SC, Sun Z, Tu J (2012) Effect of calcification on the mechanical stability of plaque based on a three-dimensional carotid bifurcation model. BMC Cardiovasc Disord 12(1):1–18
Schwab S, Besarab A, Beathard G, Brouwer D, Levine M, Mccann R, Shermann R, Trerotola S (2001) NKF-K/DOQI clinical practice guidelines for vascular access: update 2000. Am J Kidney Dis 37(1):S137–S181
Rothera C, McCallum C, Huang S, Heidenheim P, Lindsay RM (2011) The influence of between-needle cannulation distance on the efficacy of hemodialysis treatments. Hemodial Int 15(4):546–552. doi:10.1111/j.1542-4758.2011.00569.x
Lee T, Barker J, Allon M (2006) Needle infiltration of arteriovenous fistulae in hemodialysis: Risk factors and consequences. Am J Kidney Dis 47(6):1020–1026. doi:10.1053/j.ajkd.200602.181
Grigioni M, Daniele C, Morbiducci U, D’Avenio G, Di Benedetto G, Del Gaudio C, Barbaro V (2002) Computational model of the fluid dynamics of a cannula inserted in a vessel: incidence of the presence of side holes in blood flow. J Biomech 35(12):1599–1612. doi:10.1016/s0021-9290(02)00231-2
Park JY, Park CY, Min BG (2007) A numerical study on the effect of side hole number and arrangement in venous cannulae. J Biomech 40(5):1153–1157. doi:10.1016/j.jbiomech.2006.04.005
DeWachter DS, Verdonck PR, Verhoeven RF, Hombrouckx RO (1996) Red cell injury assessed in a numeric model of a peripheral dialysis needle. Asaio J 42(5):M524–M529
Liu G, Wu J, Ghista DN, Huang W, Wong KKL (2015) Hemodynamic characterization of transient blood flow in right coronary arteries with varying curvature and side-branch bifurcation angles. Comput Biol Med 64:117–126. doi:10.1016/j.compbiomed.2015.06.009
Fulker D, Simmons A, Kabir K, Kark L, Barber T (2016) The hemodynamic effects of hemodialysis needle rotation and orientation in an idealized computational model. Artif Organs 40(2):185–189. doi:10.1111/aor.12521
Acknowledgements
This work was supported by grants from National Natural Science Foundation of China (11372364, and 10902130), National Program on Key Basic Research Project (973 Program) of China (2014CB541600), Fundamental Research Funds for the Central Universities (CDJZR11230012, 106112016CDJZR235517), and Foundation for University Key young Teacher of Chongqing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Ethical approval
All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
Rights and permissions
About this article
Cite this article
Yang, L., Yin, A. & Liu, W. Variation of flow rate and angle of injected venous needle on influencing intimal hyperplasia at the venous anastomosis of the hemodialysis graft. Australas Phys Eng Sci Med 40, 239–248 (2017). https://doi.org/10.1007/s13246-017-0526-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-017-0526-6