Abstract
Objective
To explore clinicians’ knowledge and consideration of radiation, in relation to their referral practice and use of referral guidelines for imaging.
Methods
A questionnaire was handed out to 213 clinicians in Norway; all responded: 77 general practitioners, 71 hospital physicians and 65 non-physicians (55 manual physiotherapists, 10 chiropractors). Questions concerned weighting of radiation dose, guideline use, referrals unlikely to affect treatment, doses from imaging procedures, ranking of imaging as radiation source, and deterministic and stochastic effects. For radiation knowledge, a total score was aggregated.
Results
The mean radiation knowledge score was 30.4/71. Most respondents underestimated doses from high-dose imaging, e.g., barium enema (94.7%), chest CT (57.7%) and abdominal CT (52.7%). Limited radiation knowledge was not compensated by using guidelines. Only 20% of physicians and 72% of non-physicians used referral guidelines. Non-physicians weighted radiation dose as being more important than physicians when referring; they also reported fewer referrals as being unlikely to affect treatment. Such referrals and not using guidelines were related to lower weighting of radiation dose but not to radiation knowledge.
Conclusion
Limited radiation knowledge and guideline use indicate suboptimal justification of referrals. When justifying imaging, weighting of radiation dose may play a larger role than detailed radiation knowledge.
Similar content being viewed by others
Introduction
The increasing volume of medical imaging and particularly multislice computed tomography (CT) during the last few decades has turned radiation protection into one of the main concerns of the radiological community [1–4]. Justification and optimisation are cornerstones of radiation protection [5, 6], and this report deals with justification.
To be able to justify a radiation-based medical imaging procedure—that is, to weigh its costs against its benefits [6]—the referring clinician needs to know the magnitude of the radiation dose given and the possible detrimental effects of this exposure. To some degree, the lack of such knowledge could be compensated for by using referral guidelines [7–9] in the justification process.
Former studies have revealed that referring physicians possess limited knowledge about ionising radiation and its carcinogenic potential [10–22], and that referral guidelines are not widely used [23–26]. However, we have little data on radiation knowledge and use of referral guidelines among referring non-physicians, e.g., chiropractors [27, 28]. We also lack data on how knowledge and attitudes about radiation issues may relate to referral practice. Further data could help to design strategies for improving different clinicians’ justification processes and referral practices.
Accordingly, we explored general practitioners’, hospital physicians’ and non-physicians’ (1) radiation knowledge, (2) weighting of radiation dose when referring, (3) use of referral guidelines, (4) rate of and reasons for referrals unlikely to affect treatment, and (5) if this rate and their guideline use is related to their radiation knowledge and weighting. We hypothesised that clinicians who put less emphasis on radiation issues order imaging unlikely to affect treatment more often and use referral guidelines less often.
Materials and methods
In this study from Norway, hospital physicians, general practitioners, manual physiotherapists and chiropractors filled in an anonymous questionnaire. Manual physiotherapists acquired a referral licence for all techniques in 2006 and chiropractors in 1991 [29]. The study did not require approval from a research ethics committee.
Our questionnaire was based on literature review, a pilot study of six respondents and individual interviews with four clinicians to test face validity. It was handed out to 71 hospital physicians at all grades during their morning meetings at a 500-bed general hospital and to 77 general practitioners, 55 manual physiotherapists and 10 chiropractors during lectures at nation- or countywide courses of general interest within their fields, not related to radiation issues. All clinicians attending the actual meetings/ lectures were asked to fill in the questionnaire, which took about 15 min. They were not informed about the questionnaire session in advance. The first author supervised this session to ensure unaided answers.
The questions concerned, in this order: respondents’ age and gender, their weighting of (six-point scale) radiation dose and four other factors (Table 1) when referring for imaging, whether they knew of (yes/no) and had used (yes/no) referral guidelines, if they referred for imaging that most unlikely would affect treatment (yes/no), their approximate rate of such referrals (1, 5, 10, 20 or 50%) and the importance of (four-point scale) six listed reasons for such referrals (Table 1).
The next question was about effective dose, in number of chest x-rays (0–1, 1–10, 10–50 or 50–200) from 12 imaging procedures including radiography, fluoroscopy, CT, magnetic resonance imaging (MRI) and ultrasound [30] (Table 1). Respondents then had to rank the contribution of medical imaging to the mean effective dose for a Norwegian, compared with that of radon in homes, background gamma radiation, pollution from Sellafield in England and food pollution from the Chernobyl nuclear plant accident [31]. Finally, respondents were asked if they knew the terms deterministic and stochastic effects; if so, they should categorise six effects as either deterministic or stochastic [5].
We constructed a total radiation knowledge score ranging from 0 to 71. For the 12 imaging procedures, a correct dose gave 3 points and the closest wrong dose 1 point, yielding a maximum of 36 points. Ranking of radiation sources gave a maximum of 18 points. Ranking radon first and imaging second gave 9 points each, and the closest wrong rank gave 4 points. Knowing the terms stochastic and deterministic gave 5 points, and categorising the six detrimental effects correctly gave 2 points each, resulting in a maximum of 17 points. Missing data gave 0 points, and a total radiation knowledge score was noted for all participants.
For continuous normal distributed data, we used Student’s t-test and for categorical data, Wilcoxon signed rank test, Kruskal-Wallis, Mann-Whitney, Friedman’s and chi-squared tests, and Spearman's rho, as appropriate (see Results). Multiple linear regression analysis was used to examine factors that could influence radiation knowledge. Data were analysed using SPSS (version 16, SPSS Inc., Chicago, IL). A two-tailed p < 0.05 was accepted as statistically significant.
Results
All invited clinicians (n = 213) participated in the study. Their mean age (range) was 44.6 (26–73) years. There was a male predominance (66%–75%) within all three main respondent groups (77 general practitioners, 71 hospital physicians and 65 non-physicians).
Radiation knowledge
The total score of radiation knowledge was mean 30.4 (SD 8.5) or 42.8% of the maximum. Analysed with a multiple linear regression analysis, total score did not correlate with age, but differed between men and women (mean 31.4 vs. 28.2, p = 0.01) and among the three main respondent groups (p = 0.03, Table 2). Age, sex and group explained only 6.4% of the variation in this score (R2 = 0.064).
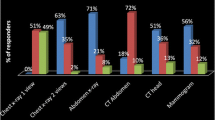
Most respondents underestimated radiation doses from high dose imaging: for barium enema 94.7%, barium meal 68.3%, chest CT 57.6%, intravenous pyelography 55.1% and abdominal CT 52.7% (Fig. 1a). The dose from paranasal sinus CT (Fig. 1b) was overestimated by 94.8%. For thoracic spine and pelvic radiography (Fig. 1c), similar proportions underestimated (21.6%, 18.7%) and overestimated dose (19.7%, 19.1%). According to 10.5% and 4.8% of respondents, MRI and ultrasound, respectively, implied some radiation dose. Dose estimates were given by 205–208 (96%–98%) of the 213 participants.
When ranking the magnitude of five different radiation sources for an average Norwegian, 38 (18.2%) out of 209 respondents correctly ranked medical imaging (1.1 mSv/year) as second after radon (3.0 mSv/year); 72 (34.4%) ranked imaging too high and 99 (47.4%) too low.
Only 34 (16.7%) out of 204 respondents stated they knew the terms deterministic and stochastic effects. When categorising six different detrimental effects as either stochastic or deterministic, these 34 respondents’ mean score was 6.8/12; chance would yield 6/12.
Weighting of radiation dose when referring
Considering a referral for imaging, respondents in the total sample weighted radiation dose as more important than the patient’s wish (p < 0.001, Wilcoxon signed rank test), but less important than the impact of the imaging on the patient’s diagnosis, treatment or future health (p < 0.001, Friedman’s test) (Table 3). Non-physicians rated radiation dose as more important than did general practitioners (p < 0.001, Mann-Whitney test) and hospital physicians (p = 0.001, Mann-Whitney test). Complete ratings were given by 212 (99.5%) of the respondents.
Use of referral guidelines
Only 58.0% (123/212) reported that they knew of referral guidelines, and 35.7% (76/213) had made use of such guidelines. The proportion that had used guidelines was higher for non-physicians (72.3%) than for general practitioners (19.5%) and hospital physicians (19.7%) (p < 0.001, chi-squared tests).
Referrals unlikely to affect treatment
As many as 88.3% of the general practitioners, 83.1% of the hospital physicians and 56.9% of the non-physicians referred for imaging that would be most unlikely to affect treatment (p < 0.001, chi-squared test). General practitioners reported a higher percentage of such referrals (median 10%) than did hospital physicians (5%, p = 0.04, chi-squared test) and non-physicians (5%, p < 0.001, chi-squared test).
Compared with the other four listed reasons for referrals that hardly affect treatment (Table 1), “normal findings will reassure the patient” and to “give the patient the feeling of being taking seriously” were rated as more important (p < 0.001, Friedman’s test). “Patient expectations” was rated as more important by general practitioners than by hospital physicians and non-physicians (p < 0.001, Mann-Whitney test). Non-physicians rated “lack of time”, “expectations from relatives” and to “compensate for insufficient clinical examination” as less important reasons than general practitioners and hospital physicians (p < 0.001, Mann-Whitney test).
Radiation issues in relation to referrals and guideline use
Lower weighting of radiation dose was related to admitting referrals unlikely to affect treatment (Figs. 2 and 3) and not having used guidelines (Fig. 4). However, the total radiation knowledge score was similar for clinicians denying (n = 49) and admitting (n = 164) referrals unlikely to affect treatment (mean 28.7 vs. 31.0, p = 0.10, Student’s t-test), did not correlate with their rate of such referrals (r = 0.14, p = 0.85, Spearman rho), and was similar for those who had and those who had not used guidelines (mean 29.4 vs. 31.0, p = 0.18, Student’s t-test).
Weighting the importance of radiation dose in relation to admitting referrals that are most unlikely to affect treatment (r = 0.14, p = 0.037, Spearman rho). 1 = very important, 6 = not important. Box-and-whisker plot where the grey box represents the interquartile range, the middle horizontal line the median and the whiskers the range. Numbered points are outliers
Weighting the importance of radiation dose in relation to percentage of referrals being most unlikely to affect treatment (r = 0.21, p = 0.005, Spearman rho). 1 = very important, 6 = not important. Box-and-whisker plot where the grey box represents the interquartile range, the middle horizontal line the median and the whiskers the range. Numbered points are outliers
Weighting the importance of radiation dose in relation to using referral guidelines (r = 0.18, p = 0.009, Spearman rho). 1 = very important, 6 = not important. Box-and-whisker plot where the grey box represents the interquartile range, the middle horizontal line the median and the whiskers the range. Numbered points are outliers
Discussion
In this study, all three respondent groups possessed limited radiation knowledge, and 80% of the physicians did not use referral guidelines. Respondents who weighted radiation dose lower when referring reported less guideline use and more referrals as being unlikely to affect treatment. Non-physicians reported fewer such referrals, more use of referral guidelines and more weight on radiation dose.
Strengths and limitations
A 100% participation rate and the unprepared, unaided responses to our questionnaire yielded more valid data on radiation knowledge than achievable in a postal or e-mail survey. However, the use of questionnaires has inherent limitations, as some answers reflect respondents’ subjective opinions. In the present study, respondents’ self report on their own practice should be interpreted with care, e.g., it may be biased by a wish to answer “correctly”. Such bias was reduced by avoiding respondent identifiers on the questionnaire and hardly explains the most salient differences and relations.
Since responses had to be unprepared and supervised, it was not feasible to recruit respondents randomly from their respective professional groups to achieve a representative sample. Our respondents may nevertheless be fairly comparable to their groups on a national level. Mean age in the study sample vs. the national population was 48.1 vs. 46.8 years for general practitioners and 40.0 vs. 43.3 years for hospital physicians [32]. Hospital physicians were recruited at morning meetings for all residents, junior and senior physicians at a general hospital with common subspecialties (Table 2). General practitioners and non-physicians were recruited from courses of general interest.
Discussion of findings
Our study confirmed that clinicians often underestimate radiation doses [10–22]. However, clinicians overestimated doses too, and some even reported radiation from MRI and ultrasound, as has also been found in other studies [10–12, 17, 19, 22]. Similarly, physicians in a former study overestimated the teratogenic risk from ionising imaging [33]. Thus, balanced information on radiation doses and risks seems mandatory.
Despite their slightly poorer radiation knowledge, non-physicians put more weight on radiation dose when referring. One reason for this may be that non-physicians face mostly benign conditions, where radiation dose is more relevant than in cases of for example malignancy. A less likely reason, but one that we cannot rule out, is that some manual physiotherapists may have rated radiation dose higher to show that they deserve their recently acquired referral licence.
Although concurring with previous findings [24, 25, 34], it was remarkable that only 20% of the physicians had used referral guidelines. Clearly, few physicians used the Norwegian translation of the EU Commission Guidelines available on the web [35]. The much higher proportion (72%) of non-physicians using guidelines could be partly explained by the fact that the manual physiotherapists have developed their own guidelines [36] and that sub-specialists may be more familiar with their own adapted guidelines than with general guidelines on the same topic [26]. More use of referral guidelines among manual physiotherapists may also be partly due to their relatively short experience with imaging referrals.
Respondents’ rates of referrals unlikely to affect treatment were smaller than some reported rates of unjustified imaging (5–10% vs. 20%) [37–39]. Our respondents may have underestimated their own rates, but the rate of unjustified and/or treatment-irrelevant imaging in Norway is not known.
As limited radiation knowledge was not compensated for by using referral guidelines, relevant information may have lacked in the justification process. Our study was not designed to examine the effect of efforts to improve this process. Yet, a higher weighting of radiation dose when referring was related to more guideline use and fewer referrals regarded as being unlikely to affect treatment. We therefore believe that increased weighting of radiation dose can help to optimise referral practice.
Implications and conclusions
Our findings do not necessarily apply in other health care systems, and they need confirmation in further studies. Nonetheless, these results have implications that may be of value to those attempting to improve the justification of imaging in cooperation with clinicians.
First, referring clinicians, both non-physicians and physicians, need information about radiation protection and the detrimental effects of radiation. To prevent overuse as well as underuse of medical imaging, this information must be balanced.
Second, referral guidelines should be more actively distributed and implemented [40–42]. For example, as a start, one could incorporate such guidelines into every hospital’s computerised referral system, giving real-time, easily accessible decision support for referring clinicians [24, 42–46].
Third, interventions to improve referral practice should target clinicians’ attitudes and not only their knowledge. Clinicians’ weighting of radiation dose seems more important to their referral practice than their detailed radiation knowledge.
Fourth, different interventions may be required for non-physicians and physicians, as they may differ in their attitudes towards radiation issues and in pre-existing guideline use and referral practice.
In conclusion, scarce radiation knowledge and limited use of referral guidelines indicate that the process of justifying imaging referrals needs to be improved. In this process, weighting of radiation dose played a larger role than detailed radiation knowledge. We found support for the hypothesis that clinicians who put less weight on radiation issues order imaging unlikely to affect treatment more often and use referral guidelines less often. Non-physicians used guidelines more often than physicians and weighted radiation dose as being more important. Efforts to improve the justification of radiation-based medical imaging should nevertheless raise awareness of radiation protection issues among all groups of referring clinicians.
References
Borretzen I, Lysdahl KB, Olerud HM (2007) Diagnostic radiology in Norway trends in examination frequency and collective effective dose. Radiat Prot Dosim 124:339–347
Brenner DJ, Hall EJ (2007) Computed tomography–an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, Shah ND, Nasir K, Einstein AJ, Nallamothu BK (2009) Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 361:849–857
Lauer MS (2009) Elements of danger–the case of medical imaging. N Engl J Med 361:841–843
The International Commission on Radiological Protection (2007) Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP 37(2–4):1–332
The International Commission on Radiological Protection (2007) Radiation protection in medicine. ICRP Publication 105. Ann ICRP 37(6):1–64
The Royal College of Radiologists (2007) Making the best use of clinical radiology services, 6th ed., London
European Commission (2007) Referral Guidelines for imaging, Luxembourg. Available via http://ec.europa.eu/energy/nuclear/radioprotection/publication/doc/118_update_en.pdf. Accessed 12 Oct 2009
American College of Radiology. ACR Appropriateness Criteria. Available via http://www.acr.org/SecondaryMainMenuCategories/quality_safety/app_criteria.aspx. Accessed 30 Sept 2009
Thomas KE, Parnell-Parmley JE, Haidar S, Moineddin R, Charkot E, BenDavid G, Krajewski C (2006) Assessment of radiation dose awareness among pediatricians. Pediatr Radiol 36:823–832
Soye JA, Paterson A (2008) A survey of awareness of radiation dose among health professionals in Northern Ireland. Br J Radiol 81:725–729
Shiralkar S, Rennie A, Snow M, Galland RB, Lewis MH, Gower-Thomas K (2003) Doctors’ knowledge of radiation exposure: questionnaire study. BMJ 327:371–372
Rice HE, Frush DP, Harker MJ, Farmer D, Waldhausen JH (2007) Peer assessment of pediatric surgeons for potential risks of radiation exposure from computed tomography scans. J Pediatr Surg 42:1157–1164
Renston JP, Connors AF Jr, DiMarco AF (1996) Survey of physicians’ attitudes about risks and benefits of chest computed tomography. South Med J 89:1067–1073
Quinn AD, Taylor CG, Sabharwal T, Sikdar T (1997) Radiation protection awareness in non-radiologists. Br J Radiol 70:102–106
Lee CI, Haims AH, Monico EP, Brink JA, Forman HP (2004) Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology 231:393–398
Jacob K, Vivian G, Steel JR (2004) X-ray dose training: are we exposed to enough? Clin Radiol 59:928–934
Heyer CM, Peters S, Lemburg S, Nicolas V (2007) Awareness of radiation exposure of thoracic CT scans and conventional radiographs: what do non-radiologists know? Rofo 179:261–267
Gumus Cesur (2009) Turkish pediatric surgeons knowledge on radiation exposure of patients during diagnostic imaging. Turkie Klinikerie J Med Sci
Finestone A, Schlesinger T, Amir H, Richter E, Milgrom C (2003) Do physicians correctly estimate radiation risks from medical imaging? Arch Environ Health 58:59–61
Correia MJ, Hellies A, Andreassi MG, Ghelarducci B, Picano E (2005) Lack of radiological awareness among physicians working in a tertiary-care cardiological centre. Int J Cardiol 103:307–311
Arslanoglu A, Bilgin S, Kubal Z, Ceyhan MN, Ilhan MN, Maral I (2007) Doctors’ and intern doctors’ knowledge about patients’ ionizing radiation exposure doses during common radiological examinations. Diagn Interv Radiol 13:53–55
Mankad K, Bull M (2005) Awareness of ‘Making the best use of a Department of Clinical Radiology’ amongst physicians. Clin Radiol 60:618–619
Bautista AB, Burgos A, Nickel BJ, Yoon JJ, Tilara AA, Amorosa JK (2009) Do clinicians use the American College of radiology appropriateness criteria in the management of their patients? AJR Am J Roentgenol 192:1581–1585
Newton J, Knight D, Woolhead G (1996) General practitioners and clinical guidelines: a survey of knowledge, use and beliefs. Br J Gen Pract 46:513–517
Tunis SR, Hayward RS, Wilson MC, Rubin HR, Bass EB, Johnston M, Steinberg EP (1994) Internists’ attitudes about clinical practice guidelines. Ann Intern Med 120:956–963
Ammendolia C, Bombardier C, Hogg-Johnson S, Glazier R (2002) Views on radiography use for patients with acute low back pain among chiropractors in an Ontario community. J Manipulative Physiol Ther 25:511–520
Ammendolia C, Cote P, Hogg-Johnson S, Bombardier C (2007) Do chiropractors adhere to guidelines for back radiographs? A study of chiropractic teaching clinics in Canada. Spine (Phila Pa 1976) 32:2509–2514
Act of 28. Feb 1997 no. 19 National Insurance Act. Ministry of Health and Social Affairs, Oslo. Available via http://www.lovdata.no/all/nl-19970228-019.html. Accessed 12 Oct 2009
Friberg EG, Widmark A, Olerud HM, Tynes , Saxebøl, G (2005) Guidance for use of medical X-ray and MR equipment subjected to approval. Guidance to “Regulations for radiation protection and use of radiation”. Guidance No.5. In Norwegian. Norwegian Radiation Protection Authority, Østerås
Norwegian Radiation Protection Authority Web site. Available via http://www.nrpa.no/index.asp? Accessed 1 Oct 2009
Norwegian Medical Association Web site. Available via http://www.legeforeningen.no/id/146323. Accessed 12 Oct 2009
Ratnapalan S, Bona N, Chandra K, Koren G (2004) Physicians’ perceptions of teratogenic risk associated with radiography and CT during early pregnancy. AJR Am J Roentgenol 182:1107–1109
Kumar S, Mankad K, Bhartia B (2007) Awareness of making the best use of a Department of Clinical Radiology amongst physicians in Leeds Teaching Hospitals, UK. Br J Radiol 80:140
Norwegian Radiology Society Web site. Available via http://www.radiologforeningen.no/external/guidelines/INDEX.html. Accessed 12 Oct 2009
Manuellterapeutenes servicekontor (2007) Retningslinjer for bildediagnostisk utredning (Guidelines for diagnostic imaging workup). In Norwegian. Available via http://www.manuellterapi.no/dokumenter/RL_bildediagnostisk_utredning_20070000.pdf Accessed 12 Oct 2009
Royal College of Radiologists Working Party (1992) A multicentre audit of hospital referral for radiological investigation in England and Wales. World Hosp 28:7–13
Royal College of Radiologists Working Party (1992) Influence of the Royal College of Radiologists’ guidelines on hospital practice: a multicentre study. BMJ 304:740–743
Almén A, Leitz W, Richter S. (2009) National Survey on Justification of CT-examinations in Sweden. 2009:3. Swedish Radiation Safety Authority.
Matowe L, Ramsay CR, Grimshaw JM, Gilbert FJ, Macleod MJ, Needham G (2002) Effects of mailed dissemination of the Royal College of Radiologists’ guidelines on general practitioner referrals for radiography: a time series analysis. Clin Radiol 57:575–578
Remedios D, McCoubrie P, The Royal College Of Radiologists Guidelines Working Party (2007) Making the best use of clinical radiology services: a new approach to referral guidelines. Clin Radiol 62:919–920
Grimshaw JM, Winkens RA, Shirran L, Cunningham C, Mayhew A, Thomas R, Fraser C (2005) Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst RevCD005471
Mendelson RM, Murray CP (2007) Towards the appropriate use of diagnostic imaging. Med J Aust 187:5–6
Sistrom CL (2005) The ACR appropriateness criteria: translation to practice and research. J Am Coll Radiol 2:61–67
Amis ES Jr, Butler PF, Applegate KE, Birnbaum SB, Brateman LF, Hevezi JM, Mettler FA, Morin RL, Pentecost MJ, Smith GG, Strauss KJ, Zeman RK (2007) American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol 4:272–284
Prevedello LM, Sodickson AD, Andriole KP, Khorasani R (2009) IT tools will be critical in helping reduce radiation exposure from medical imaging. J Am Coll Radiol 6:125–126
Acknowledgements
We would like to thank Are Hugo Pripp, PhD, Biostatistics Unit, Research Services Department, Oslo University Hospital, Oslo, for his assistance with statistical issues.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Borgen, L., Stranden, E. & Espeland, A. Clinicians’ justification of imaging: do radiation issues play a role?. Insights Imaging 1, 193–200 (2010). https://doi.org/10.1007/s13244-010-0029-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13244-010-0029-4