Abstract
Objective
We aimed to determine performance of sequential organ failure assessment (SOFA) and Sepsis in Obstetrics Score (SOS), in women with pregnancy-associated sepsis (PAS) with respect to critical care admission and mortality.
Methods
Obstetric patients with PAS fulfilling any 2 of the quick SOFA (qSOFA) criteria were enrolled as cases. The various parameters of SOFA and SOS were recorded at admission and compared for outcomes.
Results
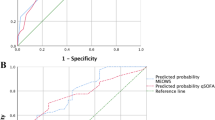
Critical care was required in 32 (50.7%) patients and associated mortality was high (31.7%). For our study population, a threshold of SOFA ≥ 6 had the best combination of sensitivity (84.4%) and specificity (61.3%) for critical care admission. For SOS, a cut-off value of ≥ 6 gave best sensitivity (64%) and specificity (40%) for the same.
Conclusions
SOFA was far more predictive of patient's critical condition as well as mortality compared to SOS. SOFA was superior to SOS in determining critical care admission and mortality for PAS.
Similar content being viewed by others
References
Ali A, Lamont RF. Recent advances in the diagnosis and management of sepsis in pregnancy. F1000Res. 2019;8.
Woodd SL, Montoya A, Barreix M, Pi L, Calvert C, Rehman AM, Chou D, Campbell OMR. Incidence of maternal peripartum infection: a systematic review and meta-analysis. PLoS Med. 2019;16:e1002984.
Mohamed-Ahmed O, Nair M, Acosta C, Kurinczuk JJ, Knight M. Progression from severe sepsis in pregnancy to death: a UK population-based case-control analysis. BJOG. 2015;122:1506–15.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315:801–10.
Bonet M, Nogueira Pileggi V, Rijken MJ, Coomarasamy A, Lissauer D, Souza JP, et al. Towards a consensus definition of maternal sepsis: results of a systematic review and expert consultation. Reprod Health. 2017;14:67.
Albright CM, Mehta ND, Rouse DJ, Hughes BL. Sepsis in pregnancy: identification and management. J Perinat Neonatal Nurs. 2016;30:95–105.
Albright CM, Has P, Rouse DJ, Hughes BL. Internal validation of the sepsis in obstetrics score to identify risk of morbidity from sepsis in pregnancy. Obstet Gynecol. 2017;130:747–55.
Bowyer L, Robinson HL, Barrett H, Crozier TM, Giles M, Idel I, et al. SOMANZ guidelines for the investigation and management sepsis in pregnancy. Aust N Z J Obstet Gynaecol. 2017;57:540–51.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304–77.
Bonet M, Souza JP, Abalos E, Fawole B, Knight M, Kouanda S, et al. The global maternal sepsis study and awareness campaign (GLOSS): study protocol. Reprod Health. 2018;15:16.
Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, et al. ICU admission, discharge, and triage Guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016;44:1553–602.
Oud L. Pregnancy associated severe sepsis. Curr Opin Obstet Gynecol. 2016;28:73–8.
Oliveira-Neto AF, Parpinelli MA, Costa ML, Souza RT, Ribeiro do Valle C, Sousa MH, et al. Prediction of severe maternal outcome among pregnant and puerperal women in obstetric ICU. Crit Care Med. 2019;47:e136–e143143.
Jain S, Guleria K, Suneja A, Vaid NB, Ahuja S. Use of the sequential organ failure assessment score for evaluating outcome among obstetric patients admitted to the intensive care unit. Int J Gynaecol Obstet. 2016;132:332–6.
Aarvold AB, Ryan HM, Magee LA, von Dadelszen P, Fjell C, Walley KR. Multiple organ dysfunction score is superior to the obstetric-specific sepsis in obstetrics score in predicting mortality in septic obstetric patients. Crit Care Med. 2017;45:e49–e57.
Aoyama K, D'Souza R, Pinto R, Ray JG, Hill A, Scales DC, Lapinsky SE, Seaward GR, Hladunewich M, Shah PS, Fowler RA. Risk prediction models for maternal mortality: a systematic review and meta-analysis. PLoS ONE. 2018;13:e0208563.
Vasquez DN, Das Neves AV, Vidal L, Moseinco M, Lapadula J, Zakalik G, et al. Characteristics, outcomes, and predictability of critically ill obstetric patients: a multicenter prospective cohort study. Crit Care Med. 2015;43:1887–97.
Funding
Nil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for Publication
The work submitted has not been published before; that it is not under consideration for publication anywhere else; that its publication has been approved by all co-authors, if any, as well as by the responsible authorities and at the institute where the work has been carried out.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Ethical Clearance
Institutional Ethical committee, University College of Medical Sciences, Delhi-110031 dated 17 October 2017.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dr. Rachna Agarwal, MS (Obstetrics & Gynaecology) is Professor at Department of Obstetrics & Gynaecology, University College of Medical Sciences & Guru Teg Bahadur Hospital, Delhi, India; Dr. Penzy Goyal, MBBS is Postgraduate student at Department of Obstetrics & Gynaecology, University College of Medical Sciences & Guru Teg Bahadur Hospital, Delhi, India; Dr. Medha Mohta, MD (Anaesthesia) is Director Professor at Department of Anaesthesia, University College of Medical Sciences & Guru Teg Bahadur Hospital, Delhi, India; Dr. Rajarshi Kar, MD (Biochemistry) is Associate Professor, Department of Biochemistry, University College of Medical Sciences & Guru Teg Bahadur Hospital, Delhi, India.
Rights and permissions
About this article
Cite this article
Agarwal, R., Goyal, P., Mohta, M. et al. Comparison of Sequential Organ Failure Assessment (SOFA) and Sepsis in Obstetrics Score (SOS) in Women with Pregnancy-Associated Sepsis with Respect to Critical Care Admission and Mortality: A Prospective Observational Study. J Obstet Gynecol India 71, 45–51 (2021). https://doi.org/10.1007/s13224-020-01375-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-020-01375-9