Abstract
Carcinosarcoma or sarcomatoid carcinoma is a highly malignant variant of squamous cell carcinoma, which comprises 2 to 3 % of all laryngeal cancer. It is considered to be a biphasic tumour, composed of a squamous cell carcinoma (in situ or invasive) and spindle cell carcinoma with sarcomatous appearance. We present a case of huge carcinosarcoma of larynx in a 34 year-old male who developed severe stridor and dysphagia. The diagnosis was confirmed histopathologically, hence the disease was treated through total laryngectomy followed by adjuvant chemotherapy and radiotherapy. The patient is well and hearty for the past one and a half years.
Similar content being viewed by others
Introduction
Carcinosarcoma of the larynx is a rare tumour and comprises 2 to 3 % of all laryngeal cancers [1]. In the literature, a variety of terms have been used to designate spindle cell carcinoma including carcinosarcoma, pseudosarcoma, sarcomatoid squamous cell carcinoma,pleomorphic carcinoma and polypoid carcinoma. Carcinosarcoma is a biphasic tumour composed of a squamous cell carcinoma either in situ or invasive and a malignant spindle cell component with a mesenchymal appearance of epithelial origin. Squamous cell carcinoma is the most common malignant tumour of the larynx, and spindle cell (sarcomatoid) carcinoma is considered to be a highly malignant variant of it. It is usually present as a large pedunculated,polypoidal neoplasm protruding from the mucosal surface [2, 3]. The predisposing factors are the same as squamous cell carcinoma including tobacco, alcohol abuse, poor oral hygiene and previous irradiation to the site from which tumour arises. Since, majority of these tumours are polypoidal or pedunculated and tend to cause obstructive symptoms, these tumours are often detected at an early stage [1, 5]. We report a case of such tumour with an unusual presentation of large polypoidal mass obliterating entire larynx and laryngopharynx. After three inconclusive biopsy reports the diagnosis of carcinosarcoma was made on fourth attempt of biopsy by laryngofissure approach.
Case Report
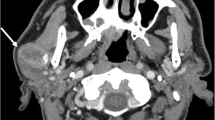
A 34 year old male presented to the department of Otolaryngology with complaints of progressive stridor, loss of voice and dysphagia for two months. Patient was being treated by general physician without getting any relief of symptoms. Finally he transported to our institution with severe stridor. The patient was cyanosed, perspired, and had strenuous breathing pattern. There was no lump in neck and direct videolaryngoscopy revealed huge whitish mass obliterating larynx up to vallecula. To secure airway, immediate tracheostomy was done, which eliminated all of his breathing problems. History revealed that the patient was heavy and chronic smoker with a habit of alcohol intake. Further examination revealed no palpable neck mass or laryngeal widening. The laryngeal crepitus was absent. Rest of Ear, Nose, Throat, Head, Neck and systemic examination were within normal limits. Haematological, biochemical profile and viral markers of the patient were normal. Since, the larynx was completely obliterated by the mass, hence Magnetic Resonance Imaging (MRI) of base of skull to clavicle was advised that showed 6.5 × 4.5 × 3.0 cm intense homogeneously enhancing polypoidal soft tissue mass in endolaryngeal region (Fig. 1a, b). The lesion had broad based attachment along the anterolateral aspect of ary-epiglottic fold of left side obliterating entire laryngeal and laryngopharyngeal region from T3 vertebral level to T6 level. The direct laryngeal biopsy was taken three times but inconclusive in each report. Finally, most of the mass was removed by laryngofissure approach and send for histopathological examination (Fig. 2). Grossly, there were bits of greyish pink friable soft tissue aggregating to 6 × 5 × 3 cm (Fig. 3). The histopathology sections showed mostly necrotic tissue with some spindle cells in a myxomatous background suggestive of mesenchymal malignant tumour. On the basis of above histopathological report and MRI findings, total laryngectomy was done and specimen was send for final histopathological reporting. Histopathological examination showed sheets of oval to spindle cells having moderately pleomorphic vesicular nucleus and intervening bands of fibrous tissue (Fig. 4). Surface epithelium was ulcerated with areas of fibrinoid necrosis. Mitotic count was >20 per 10 hpf. A diagnosis of malignant spindle cell tumour with a possibility of sarcomatoid squamous cell carcinoma was suggested. On Immunohistochemistry, Cytokeratin, Desmin, SMA, S-100, CD99, CD10 and HMB45 were non reactive. Vimentin and EMA were immunoreactive with score of 3+ and 2+ respectively (Fig. 5a, b). Thus, a diagnosis of spindle cell (sarcomatoid)carcinoma was confirmed. This was followed by radiotherapy. Patient is doing well for the past one and a half years.
Discussion
Squamous cell carcinoma is considered to be the most common type of malignant laryngeal tumour [1]. Spindle cell carcinoma or Carcinosarcoma is a highly malignant variant of squamous cell carcinoma. It is a rare tumour with a reported incidence of 2 to 3 % of all laryngeal cancers. This is a biphasic tumour composed of squamous cell carcinoma (in situ or invasive) and spindle cell carcinoma with sarcomatous appearance [2]. Spindle cell carcinoma is considered to be a monoclonal epithelial neoplasm with the sarcomatous component derived from squamous epithelium with divergent mesenchymal differentiation [3]. Although the exact cause is not known, it is strongly associated with a history of cigarette smoking and alcohol abuse as in our case. It is more common in males as compared to females (12:1 ratio), and is usually seen in the 6th and 7th decades of life. Spindle cell carcinoma most commonly affects the glottis (70 % cases), and the patients present with hoarseness, dyspnoea, cough, and dysphagia of less than 1-year duration [1]. Majority of these tumours are characterised as being polypoidal or pedunculated (98.9 %) that are often less than 2 cm in size [4]. These tumours are often extensively ulcerated, with surface fibrin deposition. Our patient had an unusual presentation with a huge and highly aggressive mass of broad base attachment to ary-epiglottic fold obliterating entire larynx and laryngopharynx.
In the past, spindle cell carcinoma has been thought to be a collision tumour between carcinoma and sarcoma. Virchow was the first person to introduce the term carcinosarcoma for this group of lesions. Kittle. E.H. in the beginning of 20th century described that many authors were of the opinion that spindle cell component is actually epithelial cells being transformed into mesenchymal cells.
This carcinoma is unusual because it manifests extensive divergent cellular differentiation with mononucleate spindle cells and multinucleate giant cells. The characteristic histomorphology is that of a conventional squamous cell carcinoma admixed with a population of atypical spindle cells. The squamous cell component is usually scant, and a thorough sampling is often required to demonstrate it. It may be invasive or in situ, and, according to some authors, only severely dysplastic squamous epithelium may be identified [5]. The difficulty in finding and identifying the squamous component may be related to the extensive surface ulceration that is frequently encountered. The sarcoma-like portion is prominent and extensive and can assume multiple patterns. Generally, an atypical spindle cell component resembling fibrosarcoma is present. Collagen is sparse but may occasionally be more prominent, as seen in our case. The sarcoma-like element may be loose and myxoid; a vascular, granulation tissue-like element may be present near the surface of tumour. Mitoses are often frequent and may be atypical. Bizarre, hyperchromatic, and multinucleated cells are common.In the absence of a histologically recognisable component of conventional squamous cell carcinoma, immunohistochemical and/or ultrastructural evidence of epithelial differentiation is required for a definitive diagnosis [6].
Epithelial markers include keratin (AE1/AE3, CK1, 8, 9), EMA, KI, and K18. Mesenchymal markers include vimentin, desmin, S-100, osteopontin, and BMP [3, 4, 7]. Immunohistochemically,the conventional carcinomatous component almost always stains for keratin. The spindle component generally stains for vimentin, and some individual tumour cells have been shown to stain for both keratin and vimentin, using an alkaline phosphatase double labelling technique [8]. However, not all cases have keratin-positive spindle cells by conventional immunohistochemical techniques and keratin staining may only be focal [5, 8]. Histologic appearance and the proportion of conventional squamous cell carcinoma have no significant bearing on clinical outcome,although keratin immunopositivity of the spindle cell has been reported to be adversely associated with the survival [9, 10]. Our case was Cytokeratin, SMA, Desmin negative and EMA and Vimentin positive.
The treatment of spindle cell carcinoma is mostly influenced by the location, vocal cord mobility and stage of tumour including metastasis. Other factors that are important include laryngeal preservation, good voice control post treatment, and a lower risk of treatment complications [4, 9]. The majority of spindle cell tumours are detected early,in stage T1 or T2, due to obstruction of larynx causing symptoms and thus have a better prognosis [4]. Tumours that are in stage T2 or less can be managed conservatively with limited field irradiation and conservative treatment to preserve the patient’s voice. Tumours that are in stage T3-T4 can be treated with local resection, partial laryngectomy, total laryngectomy with or without lymph node dissection followed by combination of radiation and chemotherapy [4]. Spindle cell carcinoma of the larynx has a very good prognosis with 5-year survival of 65–95 % [1]. Poor prognostic factors include tumour diagnosed at higher stages, large size(>3 cm) with predominance of epithelial component, non-glottic tumour, fixed vocal cord, history of radiotherapy and metastasis to regional lymph nodes or distant sites [4].
Our patient was presented in very late stage of the disease. In spite of sufficient tissue excision the diagnosis was made only after doing biopsy by laryngofissure and removal of almost entire mass. Hence there was no local or distant metastasis, the patient was managed by total laryngectomy followed by radiotherapy and chemotherapy.
References
Volker HU, Scheich M, Holler S et al (2007) Differential diagnosis of laryngeal spindle cell carcinoma and inflammatory myofibroblastic tumour-report of two cases with similar morphology. Diagn Pathol 2:1–7
Cardesa A, Zidar N (2005) Spindle cell carcinoma. In: Barnes L, Eveson JW, Reichart P, Sidransky D (eds) WHO classification of tumours. Pathology and genetics of head and neck tumours. IARC press, Lyon, p. 127
Katase N, Tamamura R, Gunduz M et al (2008) A spindle cell carcinoma presenting with osseous metaplasia in the gingiva: a case report with immunohistochemical analysis. Head Face Med 4:28. doi:10.1186/1746-160X-4-28
Thompson LDR, Wieneke JA, Miettinen M, Heffner DK (2002) Spindle cell (sarcomatoid) carcinomas of the larynx: a clinicopathologic study of 187 cases. Am J Surg Pathol 26:153–170
Ellis GL, Langloss JM, Heffner DK et al (1987) Spindle-cell carcinoma of the aerodigestive tract. An immunohistochemical analysis of 21 cases. Am J Surg Pathol 11:335–342
Pilch BZ (2007) Larynx and Trachea. In: Fletcher CDM (ed) Diagnostic histopathology of Tumors Ed, 3rd edn. Churchill Livingstone, an imprint of Elsevier Inc, p. 164
Lewis JE, Olsen KD, Sebo TJ (1997) Spindle cell carcinoma of the larynx: review of 26 cases including DNA content and immunohistochemistry. Hum Pathol 28:664–673
Zarbo RJ, Crissman JD, Venkat H et al (1986) Spindle cell carcinoma of the upper aerodigestive tract mucosa. An immunohistologic and ultrastructural study of 18 biphasic tumours and comparison with seven monophasic tumours. Am J Surg Pathol 10:741–743
Leventon GS, Evans HL (1981) Sarcomatoid squamous cell carcinoma of the mucous membranes of the Head and neck: a clinicopathologic study of 20 cases. Cancer 48:994–1003
Oslen KD, Lewis JE, Suman VJ (1997) Spindle cell carcinoma of the larynx and hypopharynx. Otolaryngol Head Neck Surg 116:47–52
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Singh, R.K., Sinha, R., Singh, A. et al. Huge Carcinosarcoma of the Endolarynx: a Rare Tumour with Unusual Presentation. Indian J Surg Oncol 8, 227–230 (2017). https://doi.org/10.1007/s13193-015-0447-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-015-0447-3