Abstract
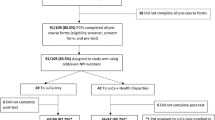
Our aim was to examine the responsiveness of a lung cancer screening brief knowledge measure (LCS-12). Eligible participants were aged 55–80 years, current smokers or had quit within 15 years, and English speaking. They completed a baseline pretest survey, viewed a lung cancer screening video-based patient decision aid, and then filled out a follow-up posttest survey. We performed a paired samples t-test, calculated effect size, and calculated absolute and relative percent improvement for each item. Participants (n = 30) were primarily White (63%) with less than a college degree (63%), and half were female (50%). Mean age was 61.5 years (standard deviation [SD] = 4.67) and average smoking history was 30.4 pack-years (range = 4.6–90.0). Mean score on the 12-item measure increased from 47.3% correct on the pretest to 80.3% correct on the posttest (mean pretest score = 5.67 vs. mean posttest score = 9.63; mean score difference = 3.97, SD = 2.87, 95% CI = 2.90, 5.04). Total knowledge scores improved significantly and were responsive to the decision aid intervention (paired samples t-test = 7.57, p < .001; Cohen’s effect size = 1.59; standard response mean [SRM] = 1.38). All individual items were responsive, yet two items had lower absolute responsiveness than the others (item 8: “Without screening, is lung cancer often found at a later stage when cure is less likely?” pretest correct = 83.3% vs. posttest = 96.7%, responsiveness = 13.4%; and item 10: “Can a CT scan find lung disease that is not cancer?” pretest correct = 80.0% vs. posttest = 93.3%, responsiveness = 13.3%). The LCS-12 knowledge measure may be a useful outcome measure of shared decision making for lung cancer screening.
Similar content being viewed by others
References
Wender R et al (2013) American Cancer Society lung cancer screening guidelines. CA Cancer J Clin 63(2):106–117
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66(1):7–30
Aberle DR et al (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365(5):395–409
Bach PB et al (2012) Benefits and harms of CT screening for lung cancer: a systematic review. J Am Med Assoc 307(22):2418–2429
Moyer VA (2014) Screening for lung cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 160(5):330–338
Decision memo for screening for lung cancer with low dose computed tomography (LDCT) (CAG-00439 N). 2015 [cited 2016 August 15]; Available from: https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId = 274
Volk RJ, Hawk E, Bevers TB (2014) Should CMS cover lung cancer screening for the fully informed patient? J Am Med Assoc 312(12):1193–1194
Sepucha K et al (2007) An approach to measuring the quality of breast cancer decisions. Patient Educ Couns 65(2):261–269
Sepucha KR et al (2013) Establishing the effectiveness of patient decision aids: key constructs and measurement instruments. BMC Medical Informatics and Decision Making 13(2):1–11
Sepucha KR et al (2014) Development and evaluation of a new survey instrument to measure the quality of colorectal cancer screening decisions. BMC Medical Informatics and Decision Making 14(1):1–9
Sepucha KR et al (2008) Developing instruments to measure the quality of decisions: early results for a set of symptom-driven decisions. Patient Educ Couns 73(3):504–510
Sepucha KR et al (2011) Decision quality instrument for treatment of hip and knee osteoarthritis: a psychometric evaluation. BMC Musculoskelet Disord 12(1):1–12
Stacey D et al (2014) Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 1. doi:10.1002/14651858.CD001431.pub4
Volk RJ et al (2013) Ten years of the International Patient Decision Aid Standards Collaboration: evolution of the core dimensions for assessing the quality of patient decision aids. BMC Medical Informatics and Decision Making 13(2):1–7
Elwyn G et al (2006) Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ 333. doi:10.1136/bmj.38926.629329.AE
Lowenstein LM et al (2016) A brief measure of Smokers’ knowledge of lung cancer screening with low-dose computed tomography. Preventive Medicine Reports 4:351–356
Harris PA et al (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Guyatt G, Walter S, Norman G (1987) Measuring change over time: assessing the usefulness of evaluative instruments. J Chronic Dis 40(2):171–178
Hays RD, Hadorn D (1992) Responsiveness to change: an aspect of validity, not a separate dimension. Qual Life Res 1(1):73–75
Husted JA et al (2000) Methods for assessing responsiveness: a critical review and recommendations. J Clin Epidemiol 53(5):459–468
Cohen J (1977) Statistical power analysis for the behavioural sciences. Academic Press, New York
Beaton DE, Hogg-Johnson S, Bombardier C (1997) Evaluating changes in health status: reliability and responsiveness of five generic health status measures in workers with musculoskeletal disorders. J Clin Epidemiol 50(1):79–93
Fitzpatrick R et al (1993) A comparison of the sensitivity to change of several health status instruments in rheumatoid arthritis. J Rheumatol 20(3):429–436
Liang MH, Fossel AH, Larson MG (1990) Comparisons of five health status instruments for orthopedic evaluation. Med Care 28(7):632–642
Garratt AM et al (1994) SF 36 health survey questionnaire: II. Responsiveness to changes in health status in four common clinical conditions. Quality in Health Care 3(4):186–192
Trikalinos, T.A., et al. 2014 Decision Aids for Cancer Screening and Treatment. AHRQ Publication No. 15-EHC002-EF [Text] 2014/12; Available from: http://www.ncbi.nlm.nih.gov/pubmed/
Acknowledgements
We would like to acknowledge Andrea P. Hempstead and Vincent F. Richards for their help with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors, Methodology Committee, or the other funders.
Sources of Support
This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Award CER-1306-03385 and by The University of Texas MD Anderson Cancer Center Duncan Family Institute for Cancer Prevention and Risk Assessment. Ashley Housten was supported by the National Cancer Institute of the National Institutes of Health under Award No. R25CA057730 (PI: Shine Chang, PhD) and by the Cancer Center Support Grant CA016672 (PI: Ronald DePinho, MD).
Rights and permissions
About this article
Cite this article
Housten, A.J., Lowenstein, L.M., Leal, V.B. et al. Responsiveness of a Brief Measure of Lung Cancer Screening Knowledge. J Canc Educ 33, 842–846 (2018). https://doi.org/10.1007/s13187-016-1153-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-016-1153-8