Abstract
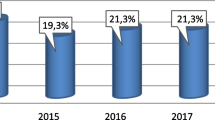
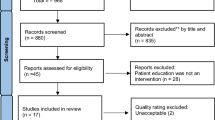
Upper extremity lymphedema occurs in one of five women after breast cancer treatment and causes significant morbidity. Women often report being uninformed regarding awareness of lymphedema and other side effects after the cancer surgery. The aim of the study was to assess the postoperative information and education about lymphedema in patients with lymphedema related to breast cancer surgery in the rehabilitation unit of a tertiary hospital. One hundred eighty patients who had admitted to lymphedema rehabilitation unit between September 2013 and February 2015 were recruited to the study. The demographic properties of women, duration, and grade of lymphedema were recorded. The patients were asked whether they had received any information about awareness of lymphedema or whether they have been educated for reducement of the risk of lymphedema after the breast cancer surgery. One hundred eighty women with a mean age of 52.9 ± 10.7 years (27–53) and with a mean lymphedema duration of 19.8 ± +39.4 months were included. Ninety-eight (54.4 %) patients had grade 1, 80 (44.4 %) patients had grade 2, and 2 (1.11 %) patients had grade 3 lymphedema. Among the participants, only 35 (19.5 %) had reported that they had received information or education about lymphedema. One hundred forty-five patients (80.5 %) were not informed or trained about the development of lymphedema. The degree and duration of lymphedema were lower in patients that had been informed or educated about lymphedema as compared to the patients who had not been informed or educated, but the difference was not statistically significant (p = 0.052). Only a minor group of patients (19 %) had received information and education about lymphedema and there is an unmet need for education or information about lymphedema after breast cancer treatment, especially in developing countries. The nonsignificant correlation between education and the degree and duration of lymphedema was thought to be related with the incongrous numbers of the subgroups. In conclusion with the growing population of breast cancer survivors, patient awareness and education about postoperative lymphedema risk after the cancer surgery is warranted.
Similar content being viewed by others
References
Yılmaz HH, Yazıhan N, Tunca D, Sevinç A, Olcayto EÖ, Özgül N, Tuncer M (2011) Cancer trends and incidence and mortality patterns in Turkey. Jpn J Clin Oncol 41(1):10–16
Rourke LL, Hunt KK, Cormier JN (2010) Breast cancer and lymphedema: a current overview for the healthcare provider. Women’s Health (Land England) 6(3):399–406
Shah C, Arthur D, Riutta J, Whitworth P, Vicini FA (2012) Breast-cancer related lymphedema: a review of procedure-specific incidence rates, clinical assessment aids, treatment paradigms and risk reduction. Breast J 18(4):357–361
Keast DH, Despatis M, Allen JO, Brassard A (2015) Chronic oedema/lymphedema:under-recognized and under-treated. Int Wound J 12(3):328–333
Çal A, Bahar Z (2016) Women’s barriers to prevention of lymphedema after breast surgery and home care needs: a qualitative study. Cancer Nurs. doi:10.1097/NCC.0000000000000326
Deng J, Fu MR, Armer JM, Cormier JN, Radina ME et al (2015) Factors associated with reported infection and lymphedema symptoms among individuals with extremity lymphedema. Rehabil Nurs 40(5):310–319
Sherman KA, Koelmeyer L (2011) The role of information sources and objective risk status on lymphedema risk-minimization behaviors in women recently diagnosed with breast cancer. Oncol Nurs Forum 38(1):E27–E36
Morcos BB, Al Ahmad F, Anabtawi I, Abu Sba AM, Shabani Y, Yaseen R (2013) Lymphedema. A significant health problem for women with breast cancer in Jordan. Saudi Med J 34(1):62–66
Tam EK, Shen L, Munneke JR, Ackerson LM, Partee PN et al (2012) Clinician awareness and knowledge in a large, integrated health care delivery setting. Breast Cancer Res Treat 131:1029–38
Choi KJ, Kim HD, Sim YJ, Kim GC, Yu BC et al (2015) A survey of status of awareness of lymphedema in breast cancer patients in Busan-Gyeongnam, Korea. Ann Rehabil Med 39(4):609–615
Kwan ML, Shen L, Munneke JR, Tam EK, Partee PN et al (2012) Patient awareness and knowledge of breast cancer related lymphedema in a large, integrated health care delivery system. Breast Cancer Res Treat 135:591–602
Fu MR, Chen CM, Haber J, Guth AA, Axelrod D (2010) The effect of providing information about lymphedema on the cognitive and symptom outcomes of breast cancer survivors. Ann Surg Oncol 17(7):1847–1853
Yıldız A, Karayurt O (2011) Difficulties experienced by the women with breast cancer experience due to lymphedema. J Breat Health 7:154–162
Herberger K, Blome C, Sandner A, Altheide F, Heyer K, Müntner KC et al (2013) Quality of care of patients with chronic lymphoedema in Germany. Dermatology 226:238–246
Paskett ED, Dean JA, Oliveri JM, Harrop JP (2012) Cancer-related lymphedema risk factors, diagnosis, treatment and impact: a review. J Clin Oncol 30(30):3726–3733
Ridner SH, Bonner CM, Deng J, Siclair VG (2012) Voices from the shadows:living with lymphedema. Cancer Nurs 35(1):18–26
Ganz PA, Yip CH, Gralow JR, Distelhorst SR, Albain KS et al (2013) Supportive care after curative treatment for breast cancer (survivorship care): resource allocations in low-middle in-come countries. A breast Health Global Initiative 2013 consensus statement. Breast 22(5):606–615
International Society of Lymphology (ISL) (2009) The diagnosis and treatment of peripheral lymphedema. 2009 consensus document of the ISL. Lymphology 42:51–60
Tagor R, Jayasinghe UW, Koelmayer L, Unq O, Boyagen J (2006) Reliability and validity of arm volume measurements for assessment of lymphedema. Phys Ther 86(2):205–214
Starritt EC, Joseph D, McKinnon JG et al (2004) Lymphedema after complete axillary node dissection for melanoma. Assessment using a new, objective definition. Annals Surg 240:866–874
Brenner E, Putz D, Moriggi B (2007) Stemmer’s (Kaposi-Stemmer) sign-30 years later. Case report and literature review. Phlebologie 36(6):320–324
Turkish Cancer Statistics Database (2011) Department of Cancer, Turkish Ministry of Health. www.saglik.gov.tr/belge/1-15486/dunya-ve-turkiyede-kanser.html. Accessed 04 Feb 2012
Ozmen V (2008) Breast cancer in the world and Turkey. J Breast Health 4(2):2–5
Birkballe S, Karlsmark T, Noerregaard S, Gottrup F (2012) A new concept of multidisciplinary lymphedema centre: established in connection to a department of dermatology and the Copenhagen Wound Healing Center. Br J Dermatol 167(1):116–122
Shah C, Ermis C, Vicini F (2013) Developing a breast cancer-related lymphedema program: the William Beamont Hospital experience. Breast J 19(1):119–120
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the institutional ethical board. All participants signed an informed consent form before including to the study.
Conflict of Interest
None
Funding
None
Rights and permissions
About this article
Cite this article
Borman, P., Yaman, A., Yasrebi, S. et al. The Importance of Awareness and Education in Patients with Breast Cancer-Related Lymphedema. J Canc Educ 32, 629–633 (2017). https://doi.org/10.1007/s13187-016-1026-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-016-1026-1