Abstract
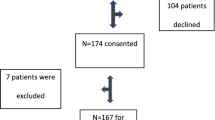
This study aims to assess the efficacy of a radiation therapy (RT) education video for patients referred for treatment. The investigators produced a 23-min guide to radiation therapy DVD, combining didactic material and patient narratives. Patients (n = 32) had not yet received their initial consultation. Baseline awareness about cancer and treatment was assessed by surveys including the rapid estimate of adult literacy in medicine. Knowledge about RT was assessed before and after viewing the video with a separate 21 question survey. Differences in benefit for sociodemographic subgroups including age, gender, ethnicity, income, education, and health literacy level were explored. Baseline assessments identified 78 % of patients regardless of sociodemographic status had “little” to “no” basic knowledge of RT. The mean number of correct responses in the 21 question survey assessing how RT works improved from 9.8 to 11.1 after watching the video (p < 0.0001; 95 % CI: 1.3–3.0), a statistically significant benefit that was present among all sociodemographic subgroups, but more prominent among those with a greater than high school education (p = 0.002). Patient satisfaction with the video was high. Knowledge among cancer patients regarding RT is poor, regardless of sociodemographic factors. This pilot study demonstrates the utility of a brief video to universally improve patient awareness about RT. While patients may ultimately learn about RT during their course of treatment, we advocate for any tools that can improve patient knowledge at the time of initial consultation as this is typically the time they are asked to acknowledge informed consent for treatment.

Similar content being viewed by others
References
The American Society for Radiation Oncology Fast Facts About Radiation Therapy. https://www.astro.org/News-and-Media/Media-Resources/FAQs/Fast-Facts-About-Radiation-Therapy/Index.aspx. Accessed 18 Feb 2013
Dunn J, Steginga SK, Rose P, Scott J, Allison R (2004) Evaluating patient education materials about radiation therapy. Patient Educ Couns 52:325–332
Jahraus D, Sokolosky S, Thurston N, Guo D (2002) Evaluation of an education program for patients with breast cancer receiving radiation therapy. Cancer Nurs 25:266–275
Hahn CA, Fish LJ, Dunn RH, Halperin EC (2005) Prospective trial of a video educational tool for radiation oncology patients. Am J Clin Oncol 28:609–612
Du W, Mood D, Gadgeel S, Simon MS (2009) An educational video to increase clinical trials enrollment among breast cancer patients. Breast Cancer Res Treat 117:339–347
Partin M, Nelson D, Radosevich D, Nugent S, Flood A, Dillon N, Holtzman J, Haas M, Wilt T (2004) Randomized trial examining the effect of two prostate cancer screening educational interventions on patient knowledge, preferences, and behaviors. J Gen Intern Med 19:835
Stanton AL (2005) Outcomes from the Moving Beyond Cancer psychoeducational, randomized, controlled trial with breast cancer patients. J Clin Oncol 23:6009
Matsuyama RK, Grange C, Lyckholm LJ, Utsey SO, Smith TJ (2007) Cultural perceptions in cancer care among African-American and Caucasian patients. J Natl Med Assoc 99(10):1113–1119
Matsuyama RK, Grange C, Lyckholm LJ, Smith TJ (2007) African-American and Caucasian female patients’ cancer and treatment information needs and preferred information sources. J Clin Oncol. ASCO Annual Meeting Proceedings Part I. Vol 25, no 18S (June 20 Supplement): 9073
Matsuyama RK, Wilson-Genderson M, Kuhn L, Moghanaki D, Vachhani H, Paasche-Orlow M (2011) Education level, not health literacy, associated with information needs for patients with cancer. Patient Educ Couns 85(3):e229–e236
Matsuyama RK, Kuhn LA, Molisani A, Wilson-Genderson MC (2013) Cancer patients’ information needs the first nine months after diagnosis. Patient Educ Couns 90:96–102
Davis TC, Crouch MA, Long SW, Jackson RH, Bates P, George RB, Bairnsfather LE (1991) Rapid assessment of literacy levels of adult primary care patients. Fam Med 23:433–435
Department of Health and Human Services (2012) Annual update of the HHS poverty guidelines. Fed Regist 77:4034, 77 Fed. Reg 4034
SAS Institute Inc (2004) SAS 9.1
Rutten LJ, Squiers L, Hesse B (2006) Cancer-related information seeking: hints from the 2003 Health Information National Trends Survey (HINTS). J Health Commun 11(Suppl 1):147–156
Squiers L, Finney Rutten LJ, Treiman K, Bright MA, Hesse B (2005) Cancer patients’ information needs across the cancer care continuum: evidence from the cancer information service. J Health Commun 10(Suppl 1):15–34
Smith TJ, Dow LA, Virago E, Khatcheressian J, Lyckholm LJ, Matsuyama R (2010) Giving honest information to patients with advanced cancer maintains hope. Oncology (Williston Park) 24:521–525
Smith TJ, Dow LA, Virago EA, Khatcheressian J, Matsuyama R, Lyckholm LJ (2011) A pilot trial of decision aids to give truthful prognostic and treatment information to chemotherapy patients with advanced cancer. J Support Oncol 9:79–86
Guleser GN, Tasci S, Kaplan B (2012) The experience of symptoms and information needs of cancer patients undergoing radiotherapy. J Cancer Educ Off J Am Assoc Cancer Educ 27:46–53
Siminoff LA, Graham GC, Gordon NH (2006) Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Educ Couns 62:355–360
Brock TP, Smith SR (2007) Using digital videos displayed on personal digital assistants (PDAs) to enhance patient education in clinical settings. Int J Med Inform 76:829–835
O’Hara L, Shue C, Marini D, Flanagan J, McKenzie J (2008) Diabetes and low health literacy: designing a mediated intervention to enhance patient–physician communication. Comm Ed 59(3):360–373
Pepe MV, Chodzko-Zajko WJ (1997) Impact of older adults’ reading ability on the comprehension and recall of cholesterol information. J Health Educ (USA) 28:21–27
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding in part by: Massey Cancer Center, Richmond, VA, USA and The American Cancer Society (MSRGT-08-143-01-CPPB #).
Appendices
Appendix 1
Understanding how radiation treatment is delivered
Not at all | A little bit | Somewhat | Quite a bit | Very well | |
1. I understand how external beam radiation works | 0 | 1 | 2 | 3 | 4 |
2. I understand what cancer is | 0 | 1 | 2 | 3 | 4 |
3. I understand the role of the radiation oncologist | 0 | 1 | 2 | 3 | 4 |
4. I understand the purpose of tattoos for radiation | 0 | 1 | 2 | 3 | 4 |
5. I understand the differences between external beam radiation and brachytherapy | 0 | 1 | 2 | 3 | 4 |
6. I understand how radiation is administered | 0 | 1 | 2 | 3 | 4 |
7. I understand how communicating with the doctor and radiation team helps | 0 | 1 | 2 | 3 | 4 |
8. I understand the role of nutrition during therapy | 0 | 1 | 2 | 3 | 4 |
Appendix 2
Understanding how radiation therapy works
-
1.
Which of the following best describes radiation therapy?
-
(a)
X-rays that destroy cancer cells
-
(b)
Drugs that destroy cancer cells
-
(c)
Surgery that removes a tumor
-
(a)
-
2.
When cancer is called “inoperable”, what does that mean?
-
(a)
Radiation therapy cannot be used
-
(b)
Surgery cannot be used
-
(c)
Chemotherapy cannot be used
-
(a)
-
3.
Radiation can injure both healthy and cancer cells.
-
(a)
True
-
(b)
False
-
(a)
-
4.
When cancer cells are growing, they are at their weakest.
-
(a)
True
-
(b)
False
-
(a)
-
7.
External beam radiation therapy makes people radioactive after treatment is over.
-
(a)
True
-
(b)
False
-
(a)
-
10.
Once radiation therapy is complete, there is no benefit for a patient to see their radiation oncologist.
-
(a)
True
-
(b)
False
-
(a)
-
11.
“Palliative” radiation is used to:
-
(a)
Cure cancer
-
(b)
Reduce symptoms, without trying to cure
-
(c)
Stop infection
-
(a)
-
13.
Side effects from radiation therapy can develop years after treatment is complete.
-
(a)
True
-
(b)
False
-
(a)
-
14.
Radiation can temporarily make cancers grow faster.
-
(a)
True
-
(b)
False
-
(a)
-
15.
Missing a few treatments during radiotherapy does not make a difference, as long as all treatments are completed.
-
(a)
True
-
(b)
False
-
(a)
-
16.
Radiation treatment using radioactive seeds is an option for all cancers.
-
(a)
True
-
(b)
False
-
(a)
-
18.
It is a good idea to try to lose weight during radiation therapy.
-
(a)
True
-
(b)
False
-
(a)
-
19.
Radiation works by:
-
(a)
Treating all cancers throughout the entire body
-
(b)
Selectively targeting only precise spots in the body
-
(a)
-
20.
Radiation cannot be given all at one time because it would make a patient too sick.
-
(a)
True
-
(b)
False
-
(a)
-
21.
Cancer cells can take months to die after radiation treatment is completed.
-
(a)
True
-
(b)
False
-
(a)
Appendix 3
Satisfaction with the video
-
1.
I learned things about radiation therapy that I did not know before.
-
(a)
True
-
(b)
False
-
(a)
-
2.
I found the video scary.
-
(a)
True
-
(b)
False
-
(a)
-
3.
I found the video depressing.
-
(a)
True
-
(b)
False
-
(a)
-
4.
I feel like I better understand what to expect with radiation therapy.
-
(a)
True
-
(b)
False
-
(a)
-
5.
I had more questions at the end of the video than before I watched it.
-
(a)
True
-
(b)
False
-
(a)
-
6.
I found the video boring.
-
(a)
True
-
(b)
False
-
(a)
-
7.
What were the three most important things you learned from the video
-
8.
What did you like about the video?
-
9.
What did you dislike about the video?
-
10.
Please suggest changes that would improve the video.
Rights and permissions
About this article
Cite this article
Matsuyama, R.K., Lyckholm, L.J., Molisani, A. et al. The Value of an Educational Video Before Consultation with a Radiation Oncologist. J Canc Educ 28, 306–313 (2013). https://doi.org/10.1007/s13187-013-0473-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-013-0473-1