Abstract
Pharmacological and device-induced reperfusion therapies have demonstrated increasingly positive outcomes regarding both reperfusion efficacy and 90-day functional outcomes after acute ischemic stroke. However, presently, only a minority of patients are eligible for these treatments. Less than 10 % of all ischemic stroke patients receive intravenous thrombolysis in most centers and it has been projected that only approximately 7–15 % of ischemic stroke patients are eligible for acute endovascular intervention. Making these effective therapies safely available to a much larger number of patients is critical for expanding the benefits of acute ischemic stroke treatment. In this article, we summarize the key results from the clinical trials, challenges, and exciting novel opportunities to increase patient eligibility for these therapies as well as for better outcomes for stroke patients.
Similar content being viewed by others
Overcoming the Challenges of Translating Preclinical Drug Development to the Clinical Setting
The cellular consequences of reduced or absent blood flow to the brain are manifold and referred to as the ischemic cascade [1]. Therapies directed at impeding components of the ischemic cascade in an attempt to prevent ischemic tissue from progressing to irreversible infarction form the basis of the neuroprotective strategy of acute ischemic stroke treatment. A large number of approaches to acute ischemic neuroprotection were shown to be beneficial in animal stroke models, performed primarily in rodents [2]. Many purported neuroprotective drugs were then studied in clinical trials, but unfortunately none of the neuroprotective drugs were found to be effective in phase III trials in which they were compared to placebo [3]. Many reasons were identified for the failure of translation of monotherapy neuroprotection from successful animal models in clinical trials [4]. Fault can be found in how the preclinical modeling was conducted as well as how the clinical assessment programs were performed (Table 1). The failures of translation led to a number of suggestions as to how make the preclinical evaluation of potential neuroprotective drugs more rigorous and to improve clinical trial design and performance. The Stroke Therapy Academic Industry Roundtable (STAIR) has published a series of papers focused on these issues and the preclinical STAIR recommendations have been widely adopted as means to improve the quality of animal studies evaluating neuroprotective drugs [5–8]. Other groups have proposed complimentary recommendations to improve preclinical neuroprotective drug evaluation [9]. One important concern is the relatively small number of laboratories that evaluated purported neuroprotective drugs in a limited number of models. To ameliorate this concern, a consortium of stroke animal modeling sites was organized to large-scale testing of promising neuroprotective drugs in multiple animal stroke models across multiple sites with rigorous performance of the necessary experiments [10]. Whether this approach to enhancing the quality of how neuroprotective drugs are evaluated in the preclinical setting increases the likelihood of successful clinical trials remains to be determined.
Advances in Acute Arterial Recanalization Strategies
In contradistinction to the disappointing clinical trial results observed with neuroprotective drugs in acute ischemic stroke, pharmacological and device-induced reperfusion therapies have demonstrated increasingly positive outcomes regarding both reperfusion efficacy and 90-day functional outcomes. The initial trials of intravenous (i.v.) recombinant tissue-type plasminogen activator (rtPA) demonstrated clear efficacy in the 3-h time window from stroke onset and reduced but still statistically significant benefit in the 3–4.5-h time window [11, 12]. A recent patient level meta-analysis of multiple i.v. rtPA trials demonstrated that when it is given in the 3-h time window, the number of patients needed to treat for one improvement in outcome is 11 and in the 3–4.5-h time period, it is 20 [13]. The reperfusion efficacy of i.v. rtPA is modest, with a greater than 50 % reperfusion efficacy as determined by the thrombolysis in cerebral infarction (TICI) perfusion scale seen in 30–40 % of treated patients in the i.v. rtPA control arms of the recently reported endovascular trials [14]. Another i.v. thrombolytic drug, tenecteplase, appears to have better reperfusion efficacy than seen with rtPA and a suggestion of better clinical outcomes in small clinical trials [15]. A head to head comparison of i.v. tenecteplase versus i.v. rtPA in acute ischemic stroke patients enrolled up to 4.5 h from stroke onset is underway. A very exciting advance in the acute stroke therapy field occurred recently with the publication of five endovascular trials within 4 months that showed a substantial improvement in 90-day functional outcome with a stent retriever deployed into a proximal vessel occlusion when compared to i.v. rtPA in most patients in the control group [16–20]. The absolute difference in 90-day modified Rankin Scale score 0–2 in the endovascular group compared to i.v. rtPA or best medical therapy in these trials ranged from 14 to 31 % and was highly statistically significant (Table 2). Similarly, the reperfusion efficacy of the stent retrievers when assessed in these trials was remarkable with up to 80–90 % of treated patients demonstrating a TICI score of 2b-3 indicating 50–100 % reperfusion of previously occluded proximal vessels. These advances in i.v. and intra-arterial therapy for acute ischemic stroke will have a profound effect on how neuroprotection should be considered and evaluated in the future. Neuroprotection should now be viewed as an adjunctive therapy to be employed before or after i.v. thrombolysis and/or endovascular stroke therapy (EST). The era of trying to develop neuroprotection as a standalone treatment for acute ischemic stroke has passed because the convincing efficacy of reperfusion therapy with i.v. rtPA and EST would make it unethical to withhold these proven therapies. Therefore, it would not be possible to evaluate a neuroprotective drug alone as compared to placebo in a time window when the neuroprotective drug might have a chance to demonstrate efficacy. Several scenarios for employing neuroprotection in conjunction with reperfusion can be envisioned and these novel approaches for testing neuroprotection will hopefully prove beneficial.
The Ischemic Penumbra as the Target of Acute Stroke Therapy
After the onset of focal brain ischemia, the brain region with impaired cerebral blood flow contains subregions that progress to irreversible injury, i.e., infarction at differing amounts of time depending primarily upon the severity of the initial CBF decline, but metabolic factors and temperature can affect the rapidity of infarct development [22]. The ischemic region that is already infarcted at any given time point after the onset of ischemic stroke is the ischemic core, while the ischemic region at risk for becoming infarcted over time is known as the ischemic penumbra. The ischemic penumbra is the tissue target of acute stroke therapies, mediated either by reperfusion or neuroprotection because of a therapeutic intervention can salvage ischemic destined to become infarcted its functional capacity should be preserved, leading to a better clinical outcome [23]. The initial i.v. clinical trials of rtPA employed very basic imaging with computed tomography (CT) scanning to exclude a hemorrhage but did not evaluate the extent of the ischemic core or penumbra. The early initiation of treatment, especially in the National Institutes for Neurological Disorders and Stroke (NINDS) rtPA trials, precluded the necessity for advanced imaging because at very early time points, the ischemic core should be small and the ischemic large in patients with large artery occlusions. The benefits of i.v. rtPA were much less robust in the 3–4.5-h time window European Cooperative Acute Stroke Study (ECASS) III trial which also employed basic CT imaging, reinforcing the concept that “time is brain,” meaning that there was apparently less potentially salvageable ischemic tissue to respond to i.v. rtPA in this time window as compared to the 0–3-h time window required in the NINDS trials [12, 24]. The much larger but less rigorous Third International Stroke trial (IST-3) of i.v. rtPA also demonstrated substantial benefit for patients treated in the 0–3-h time window, but no benefit on the primary outcome measure used in the trial for patients treated between 3 and 4.5 h [25]. The initial endovascular trials that employed the first generation of devices to remove intracranial blood clots did not show benefit for many reasons [21, 26]. Patients in these trials were treated at later time points than in the i.v. rtPA trials and problems included the long time from stroke onset to vessel opening, the relatively low percentage of patients achieving substantial reperfusion and the lack of requiring that a target vessel occlusion be present prior to randomization. None of these trials utilized advanced imaging to identify the extent of ischemic core and penumbra, as an enrollment criteria.
The ischemic core and penumbra can be approximated by obtaining either brain magnetic resonance imaging (MRI) or head CT imaging. On MRI, the lesion volume determined by diffusion-weighted imaging (DWI) prior to treatment is a reasonable estimate of the ischemic core, although small part of the DWI lesion is potentially reversible with early treatment [27]. Perfusion-weighted MRI (PWI) provides a measure of ischemic tissue at risk of becoming infarcted when the threshold of T max greater than 6 s is used to identify the region of hypoperfusion [28]. The ischemic penumbra is then derived by subtracting the DWI lesion volume from the PWI lesion volume, and this region of normal DWI and abnormal PWI is known as the diffusion/perfusion mismatch. A recent analysis of the Diffusion-Weighted Imaging Evaluation for Understanding Stroke Evolution Study-2 (DEFUSE-2) data suggested that EST was clinically beneficial in patients treated either before or after 6 h from onset who had a favorable mismatch pattern with a greater than 80 % mismatch [29]. A large, prospective new clinical trial will test this hypothesis that late time window EST with a stent retriever is beneficial in patients with a favorable mismatch pattern on MRI or CT perfusion (CTP). CTP is the other imaging modality that appears to be capable of providing a reasonable estimate of the ischemic core and penumbra. The initial studies of CTP that used cerebral blood volume measures to identify the ischemic core and CBF maps to identify the hypoperfused brain tissue raised concerns about accuracy [30]. Newer CTP studies taking a different approach to ischemic core and penumbra identification appear to be reasonably accurate, utilizing a CBF value of <30 % of the contralateral side to identify the ischemic core and the threshold of T max greater than 6 s to identify the region of hypoperfusion [31]. A more simplistic approach to identifying the ischemic core was used in some of the endovascular trials, the Alberta Stroke Program Early CT score (ASPECTS). The ASPECTS is determined by inspecting 10 prespecified brain regions on 2 slices on a noncontrast head CT. The maximum score is 10 and 1 point is taken off for each of these 10 regions that appear to be hypointense [32]. A score of 8–10 suggests a minimal or absent ischemic core, a score of 6–7 a modest sized ischemic core and a score of 0–5 a large to very large ischemic core. ASPECTS scores were obtained in 4/5 of the recently reported endovascular trials with a median value of 9 in these trials, supporting the notion that patients in these trials with a large vessel proximal occlusion had substantial amounts of ischemic penumbra prior to randomization [16–20]. The apparently small ischemic cores in patients randomized in these endovascular trials who had a documented proximal, large artery occlusion, along with the highly effective reperfusion efficacy of the stent retriever used in the trials and the rapidity of vessel opening were all important factors contributing to the success of these trials. A possible role for neuroprotection can be envisioned as adjunctive treatment with EST. Animal stroke modeling studies have demonstrated that neuroprotection given early after stroke onset can impede the enlargement of the DWI determined lesion volume, preserving a large DWI/PWI mismatch [33]. High-flow oxygen therapy functioning as a neuroprotective gas treatment was able to extend the therapeutic time window for i.v. rtPA to reduce postmortem infarct volume in a rat embolic stroke model [34]. These observations raise the intriguing hypothesis of testing neuroprotective drugs and gasses as a way to keep the ischemic core from expanding and the ischemic penumbra from shrinking prior to i.v. thrombolysis and/or EST as patients are being transported to primary or tertiary stroke centers for treatment.
Increasing the Number of Patient Eligible for Acute Stroke Therapy
The primary goal of any acute ischemic stroke therapy is aimed at improving patients’ functional status. In this respect, the results from the recent positive endovascular trials provide a long-awaited breakthrough for the treatment of large arterial strokes, demonstrating significantly improved functional outcomes at 90 days after stroke, resulting in an absolute risk benefit of 13–31 % in the proportion of patients achieving functional independence at 90 days [16–20, 35]. However, presently, only a minority of patients are eligible for acute EST. Large artery strokes are estimated to constitute approximately one quarter of all ischemic strokes (approximately 200,000 patients annually in the USA) and represent the most devastating stroke subtype. Yet, it has been projected that only approximately 7–15 % of patients are eligible for acute intervention [36–38]. Likewise, less than 10 % of all ischemic stroke patients receive i.v. rtPA in most centers [39–41]. Thus, making these effective therapies safely available to a much larger number of acute stroke patients is critical for expanding the benefits of acute ischemic stroke treatment.
One of the key challenges in acute stroke therapy relates to the concept that cerebral ischemia is a dynamic process that strongly depends on both the severity and duration of hypoperfusion. This concept has been aptly synthesized in the term “time is brain.” As outlined above, this general concept has been proven valuable in the clinical setting. However, while adhering to time-based treatment exclusion criteria that are reasonable from a population-based standpoint, it is clear that an individual brain’s “intrinsic survival time” can vary substantially between subjects. This concept is reflected in current treatment recommendations for i.v. thrombolysis where the presence of extensive (accelerated) ischemic brain injury is an accepted exclusion criterion for therapy even if patients are otherwise eligible and present within the therapeutic window. Similarly, formal ASPECTS scoring as an indicator for the extent of brain injury and thus futile if not harmful intervention was used by several of the recent EST trials to screen patients for study inclusion. Recent developments in neuroimaging technology now allow for defining tissue signatures that identify those patients that can be included in the extended time window.
In addition, there exists now an exciting opportunity to reassess the potential beneficial effect of brain-protective strategies to complement acute strategies for cerebrovascular recanalization. Despite extensive research, to date, no preclinically effective candidate neuroprotectant demonstrated efficacy in clinical trials [42]. As discussed, the putative reasons for this are manifold, including not only suboptimal clinical trial design but also inappropriate preclinical stroke modeling, which resulted in the call for more rigorous design of animal stroke studies with higher quality standard levels to avoid bias such as outlined by STAIR committee [5, 7, 43]. While the STAIR recommendations have not (yet) resulted in therapeutic success, the proposed criteria are intuitive and consistent with best scientific practice [5, 7]. Furthermore, no candidate compound has met all STAIR criteria prior to its use in the clinical setting [44, 45], for which reason the lack of neuroprotectant efficacy in prior studies should not be construed to indicate that neuroprotective strategies cannot be translated into beneficial outcomes in the clinical setting.
In this respect, EST provides a unique opportunity for acute ischemic stroke therapy. In contrast to the situation in many patients treated with i.v. rtPA, patients considered for EST have a similar pathophysiological constellation to that of preclinically studied scenarios: EST patients have a large arterial occlusion that is associated with an ischemic core that is surrounded by hypoperfused, yet salvageable brain tissue [46–48]. Second, EST allows for superselective targeted drug delivery, which may allow for local synergistic effects while reducing systemic drug-related adverse effects [49]. Third, much higher recanalization rates are achieved with EST than with i.v. thrombolysis [19]. This is important as it has been repeatedly shown in preclinical studies that most putative neuroprotective agents are much less efficacious in the absence of timely recanalization and nutritious reperfusion [34, 50, 51]. In addition, recanalization not only facilitates drug delivery to the brain but also represents a therapeutic target as recanalization can be associated with deleterious reperfusion-associated injury [7, 52, 53].
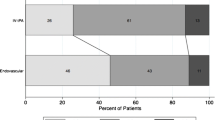
Several key strategies can, therefore, be envisioned to improve patient eligibility for acute recanalization therapies as well as to increase treatment efficacy and safety (Fig. 1). First, a major goal is to facilitate early therapy and prevent the progression of ischemic brain tissue towards infarction. Several preclinical studies have provided proof-of-principle data that it is possible to slow down or even completely arrest the progression of infarct growth for several hours through pharmacological and non-pharmacological interventions (penumbral “freezing”) [33, 34, 50, 54–56]. One exciting possibility is to treat patients “in the field,” thereby increasing the number of patients presenting with a favorable imaging profile for subsequent i.v. thrombolysis and EST. Importantly, the feasibility of rapid prehospital delivery of putative cerebroprotective agents has already been shown in the Field Administration of Stroke Therapy-Magnesium (FAST-MAG) trial [57]. While the trial was negative for its primary endpoint, it reported an impressive median interval time of <1 h from symptom onset to drug administration, with 73 % of subjects receiving the study drug within 1 h of symptom onset [57]. Hence, it is now possible to implement prehospital therapy to increase the number of EST candidate patients that otherwise would not reach a dedicated tertiary stroke center in time. In addition, implementation of mobile CT scan units in conjunction with telemedicine consultation will allow for defining stroke subtype and to determine the presence of large artery occlusion already en route to the hospital and thus optimize patient triage and ultra-early treatment decisions such as to give rtPA in the ambulance [58, 59].
General concepts to increase the number of patient eligible for acute stroke therapy and improve post-stroke outcome. a Early post-NINDS rtPA era: Stroke patients received systemic thrombolysis after exclusion of contraindications. b Present: Endovascular stroke therapy increases the proportion of patients with favorable outcome after large arterial occlusion. Telestroke evaluation aids in the early assessment of patients at spoke hospitals (asterisk) to render decisions for patient transfer to dedicated stroke centers resulting in greater numbers of treated patients. Advanced neuroimaging is used to select patients most likely to benefit from aggressive intervention. c Future: Telestroke and neuroimaging are done prehospital (1) and supplemented by neuroprotection strategies to increase the number of patient eligible for recanalization therapy and treatment within the “golden hour.” Intra-hospital (2) standard therapy is supplemented by novel neuroprotection therapies to improve treatment efficacy and safety. Green patients with good outcome, red patients with poor outcome. Vertical dashed line indicates the pre- vs. intra-hospital care
A second major strategy will include treatments that capitalize on superselective endovascular application or that can be applied in conjunction with EST. For example, to avoid liver first-pass, shear activated nano-particles conjugated to rtPA have been infused locally to break up into individual nanoscale components that then adhere to the clot surface for concentrated rtPA delivery and augmented clot dissolution and minimize device-induced endothelial injury [49, 60]. Several prospective observational studies indicated that increased body temperature is associated with a poor outcome; in animal stroke models, hypothermia achieved remarkable reductions in infarct size, and cooling has demonstrated improved outcomes after cardiac arrest in randomized clinical trials. Therefore, hypothermia is being explored as a promising adjunct therapy for the management of acute stroke patients that could be initiated during or shortly after EST [61–64]. Another non-pharmacological recanalization strategy includes sonothrombolysis, which may enhance clot dissolution via endovascular or transcranial ultrasound [65, 66]. Many of the previously evaluated neuroprotective drugs with favorable preclinical studies when combined with reperfusion could be considered as a combination with reperfusion therapy [67]. Granulocyte colony-stimulating factor (G-CSF) is one such drug that was demonstrated to extend the therapeutic time window in animal studies and reduce rtPA-induced hemorrhagic transformation [56, 68].
Arterial recanalization is not without risk and tissue injury following reperfusion has been well described in experimental ischemic stroke [53]. This so-called reperfusion injury is thought to be initiated by an overproduction of reactive oxygen species in mitochondria resulting in oxidative stress [53]. Reperfusion injury is associated with inflammatory processes, microvascular occlusion, and cell death as well as cell-matrix degeneration that can result in the disruption of the blood-brain barrier with resultant development of deleterious vasogenic edema and hemorrhagic transformation [69, 70]. While in the recent EST trials, the overall risk for symptomatic intracranial hemorrhage was not significantly different from patients treated with standard medical care [35], the overall incidence of hemorrhagic transformation after EST has been reported for as many as one in five patients (one in six patients had asymptomatic hemorrhagic transformation) [20]. This is an important issue as the outcomes of reperfusion-associated injury in the clinical setting are still poorly understood [71, 72]. In particular, a possible role of asymptomatic hemorrhagic transformation in worsening post-stroke outcome remains to be clarified. While data from the ECASS II cohort was reassuring in this respect [73], a trend towards worse outcomes was noted in subjects included in the NINDS and Alteplase Thrombolysis for Acute Noninterventional Therapy in Ischemic Stroke (ATLANTIS) studies [74]. More concerning, several cohort studies suggested that even patients with asymptomatic hemorrhagic transformation have a higher risk for a poor 90-day and 1-year outcome [75–77]. Thus, further research is required to determine the contribution of blood-brain barrier disruption (with or without hemorrhagic transformation) to patient outcome. Given the contribution of inflammatory processes to reperfusion-associated injury, an exciting possibility is the use of immunomodulatory therapies to attenuate reperfusion-related sequelae [69]. Indeed, a recent pilot study provided proof-of-concept for this approach by showing that combination of rtPA with fingolimod, a sphingosine-1-phosphate receptor modulator that has been approved as disease-modifying therapy for the relapsing-remitting form of multiple sclerosis, was associated with less ischemic lesion growth, smaller infarct volumes, less hemorrhagic transformation, as well as overall improved functional status by day 90 [78]. While these data have to be interpreted with great caution given the small sample size, they nevertheless show the feasibility of this promising approach.
Considerations for Future Neuroprotection Trials
Future neuroprotection trials will focus on using neuroprotective agents as adjunctive therapies to i.v. rtPA and endovascular therapies. Two main approaches should be considered; the first to give the neuroprotective agent either in ambulance or at the initial hospital where the acute ischemic stroke patient is evaluated. As briefly mentioned, the recently published FAST-MAG trial of i.v. magnesium sulfate although not demonstrating efficacy with this drug was a very important trial because it showed how a large phase III acute stroke therapy trial could be done with randomization, obtaining informed consent and initiation of study drug in the ambulance [57]. The median time from stroke onset to initiation of study drug was truly remarkable in the trial, 45 and 46 min in the two study arms. Only 3.9 % of the patients included in the trial were determined to have a condition mimicking ischemic stroke and 22.8 % were determined to have an intracranial hemorrhage. A clinical trial can be envisioned in which a neuroprotective drug or gas is initiated in the ambulance using the FAST-MAG approach to study design and implementation. The predefined target population of the study would be patients with a proximal, large vessel occlusion that is identified with CT angiography (CTA) or magnetic resonance angiography (MRA) upon arrival in hospital. The primary goal of the trial would be to preserve the ischemic penumbra and to impede enlargement of the ischemic core during transport of the patient to a tertiary center capable of doing endovascular therapy. Therefore, the primary outcome measure in the predefined target population would be an imaging one, the volume of the ischemic core and ischemic penumbra determined by CTP or DWI/PWI MRI upon arrival at the tertiary center and before the endovascular procedure is performed. The patients included in the trial could potentially be enriched by utilizing telemedicine in the ambulance and performing an National Institutes of Health Stroke Scale (NIHSS) score using this technology to only include a score of 10 or more which is likely to identify patients with a large vessel occlusion and to use the exam by the telemedicine consultant to exclude patients with a posterior circulation occlusion where imaging assessment of the ischemic core and penumbra is more tenuous [79]. Of course, long-term clinical outcome and safety information will be collected and included among the secondary outcome measures of the trial. A more targeted variant of such a prehospital clinical trial would be to focus on patients who are initially assessed at an outlying hospital who are then referred and transported to a large center performing EST. In such a trial, the initial imaging, presumably a head CT, CTA, and CTP would be performed at the outlying hospital and only patients meeting accepted criteria for EST would be randomized to active neuroprotective treatment or placebo. After the initial randomization and transport of the patient to the tertiary center, the patient would be clinically evaluated and imaged again to determine if the volume of the ischemic core and penumbra have changed since the initial scans were obtained and these measurements would form the basis of the primary outcome measure of the trial. Appropriate patients would then undergo the endovascular procedure and long-term clinical outcome and safety information obtained. The goals of the two types of trials outlined would be to determine if neuroprotective therapy initiated early after ischemic stroke onset can slow down the expansion of the ischemic core and shrinkage of the ischemic penumbra so that patients being transported long distances or in whom there are delays in beginning endovascular therapy with a stent retriever might still benefit from this robustly effective treatment can be used in as many patients as possible.
The second potential approach that should explore the use of neuroprotection as adjunctive therapy with successful endovascular therapy would be to target reperfusion injury. Until recently, reperfusion injury was of theoretical concern but now that the stent retrievers have demonstrated such a high percentage of reperfusion, its relevance to the ultimate outcome of ischemic stroke patients may assume increasing importance [71]. As discussed, there are many potential contributing mechanisms to reperfusion injury and therefore a number of potential therapeutic targets. After extensive animal modeling experiments have identified the most promising therapeutic targets, clinical trials will need to be carefully designed and implemented. Only patients with documented reperfusion exceeding 50 % of baseline hypoperfused, ischemic tissue and/or blood vessels should be enrolled in such trials. Patients with large ischemic cores after successful reperfusion will likely be excluded, as will patients with substantial hemorrhagic conversion in the ischemic region. All of these inclusion/exclusion criteria will require a repeat head CT, CTA, and CTP after completion of the endovascular procedure. The high rate of good to excellent functional outcome observed in the prior endovascular trials will make it difficult to detect any additional benefit that might occur with a treatment targeting reperfusion injury even in carefully selected patients. The control arm of such a trial will have had successful reperfusion by a stent retriever and the recent endovascular trials suggest that 50–70 % of these controls will have a favorable 90-day outcome on the modified Rankin Scale (mRS), so to increase that number by 10–15 % will require a large sample size to be appropriately powered.
References
Puyal J, Ginet V, Clarke PG. Multiple interacting cell death mechanisms in the mediation of excitotoxicity and ischemic brain damage: a challenge for neuroprotection. Prog Neurobiol. 2013;105:24–48. doi:10.1016/j.pneurobio.2013.03.002.
Schabitz WR, Fisher M. Perspectives on neuroprotective stroke therapy. Biochem Soc Trans. 2006;34:1271–6. doi:10.1042/BST0341271.
Henninger N, Kumar R, Fisher M. Acute ischemic stroke therapy. Expert Rev Cardiovasc Ther. 2010;8:1389–98. doi:10.1586/erc.10.128.
Savitz SI, Fisher M. Future of neuroprotection for acute stroke: in the aftermath of the SAINT trials. Ann Neurol. 2007;61:396–402. doi:10.1002/ana.21127.
Stroke therapy academic industry roundtable (STAIR). Recommendations for standards regarding preclinical neuroprotective and restorative drug development. Stroke. 1999;30(12):2752–8.
Stroke therapy academic industry roundtable II (STAIR-II). Recommendations for clinical trial evaluation of acute stroke therapies. Stroke. 2001;32(7):1598–606.
Fisher M, Feuerstein G, Howells DW, Hurn PD, Kent TA, Savitz SI, et al. Update of the stroke therapy academic industry roundtable preclinical recommendations. Stroke. 2009;40:2244–50. doi:10.1161/STROKEAHA.108.541128.
Saver JL, Jovin TG, Smith WS, Albers GW, Baron JC, Boltze J, et al. Stroke treatment academic industry roundtable: research priorities in the assessment of neurothrombectomy devices. Stroke. 2013;44:3596–601. doi:10.1161/STROKEAHA.113.002769.
Sena E, van der Worp HB, Howells D, Macleod M. How can we improve the pre-clinical development of drugs for stroke? Trends Neurosci. 2007;30:433–9. doi:10.1016/j.tins.2007.06.009.
Llovera G, Hofmann K, Roth S, Salas-Perdomo A, Ferrer-Ferrer M, Perego C, et al. Results of a preclinical randomized controlled multicenter trial (pRCT): anti-CD49d treatment for acute brain ischemia. Sci Transl Med. 2015;7:299ra121. doi:10.1126/scitranslmed.aaa9853.
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–7.
Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–29. doi:10.1056/NEJMoa0804656.
Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384:1929–35. doi:10.1016/S0140-6736(14)60584-5.
Albers GW, Goyal M, Jahan R, Bonafe A, Diener HC, Levy EI, et al. Relationships between imaging assessments and outcomes in Solitaire with the intention for thrombectomy as primary endovascular treatment for acute ischemic stroke. Stroke. 2015;46:2786–94. doi:10.1161/STROKEAHA.115.010710.
Parsons M, Spratt N, Bivard A, Campbell B, Chung K, Miteff F, et al. A randomized trial of tenecteplase versus alteplase for acute ischemic stroke. N Engl J Med. 2012;366:1099–107. doi:10.1056/NEJMoa1109842.
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20. doi:10.1056/NEJMoa1411587.
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30. doi:10.1056/NEJMoa1414905.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015. doi:10.1056/NEJMoa1415061.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–18. doi:10.1056/NEJMoa1414792.
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–306. doi:10.1056/NEJMoa1503780.
Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368:893–903. doi:10.1056/NEJMoa1214300.
Shen Q, Ren H, Cheng H, Fisher M, Duong TQ. Functional, perfusion and diffusion MRI of acute focal ischemic brain injury. J Cereb Blood Flow Metab. 2005;25:1265–79. doi:10.1038/sj.jcbfm.9600132.
Fisher M. The ischemic penumbra: a new opportunity for neuroprotection. Cerebrovasc Dis. 2006;21 Suppl 2:64–70. doi:10.1159/000091705.
Saver JL. Time is brain--quantified. Stroke. 2006;37:263–6. doi:10.1161/01.STR.0000196957.55928.ab.
Sandercock P, Wardlaw JM, Lindley RI, Dennis M, Cohen G, Murray G, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet. 2012;379:2352–63. doi:10.1016/S0140-6736(12)60768-5.
Kidwell CS, Jahan R, Gornbein J, Alger JR, Nenov V, Ajani Z, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368:914–23. doi:10.1056/NEJMoa1212793.
Nagakane Y, Christensen S, Brekenfeld C, Ma H, Churilov L, Parsons MW, et al. EPITHET: positive result after reanalysis using baseline diffusion-weighted imaging/perfusion-weighted imaging co-registration. Stroke. 2011;42:59–64. doi:10.1161/STROKEAHA.110.580464.
Wheeler HM, Mlynash M, Inoue M, Tipirneni A, Liggins J, Zaharchuk G, et al. Early diffusion-weighted imaging and perfusion-weighted imaging lesion volumes forecast final infarct size in DEFUSE 2. Stroke. 2013;44:681–5. doi:10.1161/STROKEAHA.111.000135.
Lansberg MG, Cereda CW, Mlynash M, Mishra NK, Inoue M, Kemp S, et al. Response to endovascular reperfusion is not time-dependent in patients with salvageable tissue. Neurology. 2015;85:708–14. doi:10.1212/WNL.0000000000001853.
Wintermark M, Flanders AE, Velthuis B, Meuli R, van Leeuwen M, Goldsher D, et al. Perfusion-CT assessment of infarct core and penumbra: receiver operating characteristic curve analysis in 130 patients suspected of acute hemispheric stroke. Stroke. 2006;37:979–85. doi:10.1161/01.STR.0000209238.61459.39.
Lin L, Bivard A, Levi CR, Parsons MW. Comparison of computed tomographic and magnetic resonance perfusion measurements in acute ischemic stroke: back-to-back quantitative analysis. Stroke. 2014;45:1727–32. doi:10.1161/STROKEAHA.114.005419.
Liebeskind DS, Jahan R, Nogueira RG, Jovin TG, Lutsep HL, Saver JL. Serial Alberta Stroke Program early CT score from baseline to 24 hours in Solitaire Flow Restoration with the Intention for Thrombectomy study: a novel surrogate end point for revascularization in acute stroke. Stroke. 2014;45:723–7. doi:10.1161/STROKEAHA.113.003914.
Bratane BT, Cui H, Cook DJ, Bouley J, Tymianski M, Fisher M. Neuroprotection by freezing ischemic penumbra evolution without cerebral blood flow augmentation with a postsynaptic density-95 protein inhibitor. Stroke. 2011;42:3265–70. doi:10.1161/STROKEAHA.111.618801.
Henninger N, Bratane BT, Bastan B, Bouley J, Fisher M. Normobaric hyperoxia and delayed tPA treatment in a rat embolic stroke model. J Cereb Blood Flow Metab. 2009;29:119–29. doi:10.1038/jcbfm.2008.104.
Badhiwala JH, Nassiri F, Alhazzani W, Selim MH, Farrokhyar F, Spears J, et al. Endovascular thrombectomy for acute ischemic stroke: a meta-analysis. JAMA. 2015;314:1832–43. doi:10.1001/jama.2015.13767.
Meyers PM, Schumacher HC, Connolly Jr ES, Heyer EJ, Gray WA, Higashida RT. Current status of endovascular stroke treatment. Circulation. 2011;123:2591–601. doi:10.1161/CIRCULATIONAHA.110.971564.
Cloft HJ, Rabinstein A, Lanzino G, Kallmes DF. Intra-arterial stroke therapy: an assessment of demand and available work force. AJNR Am J Neuroradiol. 2009;30:453–8. doi:10.3174/ajnr.A1462.
Wardlaw JM, Dennis MS. Thrombectomy for acute ischemic stroke. JAMA. 2015;314:1803–5. doi:10.1001/jama.2015.14674.
Kleindorfer D, Lindsell CJ, Brass L, Koroshetz W, Broderick JP. National US estimates of recombinant tissue plasminogen activator use: ICD-9 codes substantially underestimate. Stroke. 2008;39:924–8. doi:10.1161/STROKEAHA.107.490375.
Asplund K, Glader EL, Norrving B, Eriksson M. Effects of extending the time window of thrombolysis to 4.5 hours: observations in the Swedish stroke register (riks-stroke). Stroke. 2011;42:2492–7. doi:10.1161/STROKEAHA.111.618587.
Adeoye O, Hornung R, Khatri P, Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States: a doubling of treatment rates over the course of 5 years. Stroke. 2011;42:1952–5. doi:10.1161/STROKEAHA.110.612358.
O’Collins VE, Macleod MR, Donnan GA, Horky LL, van der Worp BH, Howells DW. 1,026 experimental treatments in acute stroke. Ann Neurol. 2006;59:467–77. doi:10.1002/ana.20741.
Minnerup J, Sutherland BA, Buchan AM, Kleinschnitz C. Neuroprotection for stroke: current status and future perspectives. Int J Mol Sci. 2012;13:11753–72. doi:10.3390/ijms130911753.
Philip M, Benatar M, Fisher M, Savitz SI. Methodological quality of animal studies of neuroprotective agents currently in phase II/III acute ischemic stroke trials. Stroke. 2009;40:577–81. doi:10.1161/STROKEAHA.108.524330.
Tymianski M. Can molecular and cellular neuroprotection be translated into therapies for patients?: yes, but not the way we tried it before. Stroke. 2010;41:S87–90. doi:10.1161/STROKEAHA.110.595496.
Mehra M, Henninger N, Hirsch JA, Chueh J, Wakhloo AK, Gounis MJ. Preclinical acute ischemic stroke modeling. J Neurointerv Surg. 2012;4:307–13. doi:10.1136/neurintsurg-2011-010101.
Henninger N, Sicard KM, Schmidt KF, Bardutzky J, Fisher M. Comparison of ischemic lesion evolution in embolic versus mechanical middle cerebral artery occlusion in Sprague Dawley rats using diffusion and perfusion imaging. Stroke. 2006;37:1283–7. doi:10.1161/01.STR.0000217223.72193.98.
Manning NW, Campbell BC, Oxley TJ, Chapot R. Acute ischemic stroke: time, penumbra, and reperfusion. Stroke. 2014;45:640–4. doi:10.1161/STROKEAHA.113.003798.
Marosfoi MG, Korin N, Gounis MJ, Uzun O, Vedantham S, Langan ET, et al. Shear-activated nanoparticle aggregates combined with temporary endovascular bypass to treat large vessel occlusion. Stroke. 2015. doi:10.1161/STROKEAHA.115.011063.
Henninger N, Bouley J, Nelligan JM, Sicard KM, Fisher M. Normobaric hyperoxia delays perfusion/diffusion mismatch evolution, reduces infarct volume, and differentially affects neuronal cell death pathways after suture middle cerebral artery occlusion in rats. J Cereb Blood Flow Metab. 2007;27:1632–42. doi:10.1038/sj.jcbfm.9600463.
Kim HY, Singhal AB, Lo EH. Normobaric hyperoxia extends the reperfusion window in focal cerebral ischemia. Ann Neurol. 2005;57:571–5. doi:10.1002/ana.20430.
Ip HL, Liebeskind DS. The future of ischemic stroke: flow from prehospital neuroprotection to definitive reperfusion. Interv Neurol. 2014;2:105–17. doi:10.1159/000357164.
Jung JE, Kim GS, Chen H, Maier CM, Narasimhan P, Song YS, et al. Reperfusion and neurovascular dysfunction in stroke: from basic mechanisms to potential strategies for neuroprotection. Mol Neurobiol. 2010;41:172–9. doi:10.1007/s12035-010-8102-z.
Bardutzky J, Meng X, Bouley J, Duong TQ, Ratan R, Fisher M. Effects of intravenous dimethyl sulfoxide on ischemia evolution in a rat permanent occlusion model. J Cereb Blood Flow Metab. 2005;25:968–77. doi:10.1038/sj.jcbfm.9600095.
Henninger N, Fisher M. Stimulating circle of Willis nerve fibers preserves the diffusion-perfusion mismatch in experimental stroke. Stroke. 2007;38:2779–86. doi:10.1161/STROKEAHA.107.485581.
Bratane BT, Bouley J, Schneider A, Bastan B, Henninger N, Fisher M. Granulocyte-colony stimulating factor delays PWI/DWI mismatch evolution and reduces final infarct volume in permanent-suture and embolic focal cerebral ischemia models in the rat. Stroke. 2009;40:3102–6. doi:10.1161/STROKEAHA.109.553958.
Saver JL, Starkman S, Eckstein M, Stratton SJ, Pratt FD, Hamilton S, et al. Prehospital use of magnesium sulfate as neuroprotection in acute stroke. N Engl J Med. 2015;372:528–36. doi:10.1056/NEJMoa1408827.
Ebinger M, Winter B, Wendt M, Weber JE, Waldschmidt C, Rozanski M, et al. Effect of the use of ambulance-based thrombolysis on time to thrombolysis in acute ischemic stroke: a randomized clinical trial. JAMA. 2014;311:1622–31. doi:10.1001/jama.2014.2850.
Audebert HJ, Saver JL, Starkman S, Lees KR, Endres M. Prehospital stroke care: new prospects for treatment and clinical research. Neurology. 2013;81:501–8. doi:10.1212/WNL.0b013e31829e0fdd.
Korin N, Kanapathipillai M, Matthews BD, Crescente M, Brill A, Mammoto T, et al. Shear-activated nanotherapeutics for drug targeting to obstructed blood vessels. Science. 2012;337:738–42. doi:10.1126/science.1217815.
van der Worp HB, Macleod MR, Bath PM, Demotes J, Durand-Zaleski I, Gebhardt B, et al. EuroHYP-1: European multicenter, randomized, phase III clinical trial of therapeutic hypothermia plus best medical treatment vs. best medical treatment alone for acute ischemic stroke. Int J Stroke. 2014;9:642–5. doi:10.1111/ijs.12294.
Horn CM, Sun CH, Nogueira RG, Patel VN, Krishnan A, Glenn BA, et al. Endovascular Reperfusion and Cooling in Cerebral Acute Ischemia (ReCCLAIM I). J Neurointerv Surg. 2014;6:91–5. doi:10.1136/neurintsurg-2013-010656.
van der Worp HB, Sena ES, Donnan GA, Howells DW, Macleod MR. Hypothermia in animal models of acute ischaemic stroke: a systematic review and meta-analysis. Brain. 2007;130:3063–74. doi:10.1093/brain/awm083.
Donnino MW, Andersen LW, Berg KM, Reynolds JC, Nolan JP, Morley PT, et al. Temperature management after cardiac arrest: an advisory statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care. Perioper Resuscitation Circ. 2015. doi:10.1161/CIR.0000000000000313.
Kuliha M, Roubec M, Jonszta T, Krajca J, Czerny D, Krajina A, et al. Safety and efficacy of endovascular sonolysis using the EkoSonic endovascular system in patients with acute stroke. AJNR Am J Neuroradiol. 2013;34:1401–6. doi:10.3174/ajnr.A3416.
Schellinger PD, Alexandrov AV, Barreto AD, Demchuk AM, Tsivgoulis G, Kohrmann M, et al. Combined lysis of thrombus with ultrasound and systemic tissue plasminogen activator for emergent revascularization in acute ischemic stroke (CLOTBUST-ER): design and methodology of a multinational phase 3 trial. Int J Stroke. 2015;10:1141–8. doi:10.1111/ijs.12536.
Fisher M, Saver JL. Future directions of acute ischaemic stroke therapy. Lancet Neurol. 2015;14:758–67. doi:10.1016/S1474-4422(15)00054-X.
dela Pena IC, Yoo A, Tajiri N, Acosta SA, Ji X, Kaneko Y, et al. Granulocyte colony-stimulating factor attenuates delayed tPA-induced hemorrhagic transformation in ischemic stroke rats by enhancing angiogenesis and vasculogenesis. J Cereb Blood Flow Metab. 2015;35:338–46. doi:10.1038/jcbfm.2014.208.
Iadecola C, Anrather J. The immunology of stroke: from mechanisms to translation. Nat Med. 2011;17:796–808. doi:10.1038/nm.2399.
Sanderson TH, Reynolds CA, Kumar R, Przyklenk K, Huttemann M. Molecular mechanisms of ischemia-reperfusion injury in brain: pivotal role of the mitochondrial membrane potential in reactive oxygen species generation. Mol Neurobiol. 2013;47:9–23. doi:10.1007/s12035-012-8344-z.
Warach S, Latour LL. Evidence of reperfusion injury, exacerbated by thrombolytic therapy, in human focal brain ischemia using a novel imaging marker of early blood-brain barrier disruption. Stroke. 2004;35:2659–61. doi:10.1161/01.STR.0000144051.32131.09.
Leigh R, Jen SS, Hillis AE, Krakauer JW, Barker PB. Pretreatment blood-brain barrier damage and post-treatment intracranial hemorrhage in patients receiving intravenous tissue-type plasminogen activator. Stroke. 2014;45:2030–5. doi:10.1161/STROKEAHA.114.005249.
Berger C, Fiorelli M, Steiner T, Schabitz WR, Bozzao L, Bluhmki E, et al. Hemorrhagic transformation of ischemic brain tissue: asymptomatic or symptomatic? Stroke. 2001;32:1330–5.
Kent DM, Hinchey J, Price LL, Levine SR, Selker HP. In acute ischemic stroke, are asymptomatic intracranial hemorrhages clinically innocuous? Stroke. 2004;35:1141–6. doi:10.1161/01.STR.0000125712.02090.6e.
Lei C, Wu B, Liu M, Chen Y. Asymptomatic hemorrhagic transformation after acute ischemic stroke: is it clinically innocuous? J Stroke Cerebrovasc Dis. 2014;23:2767–72. doi:10.1016/j.jstrokecerebrovasdis.2014.06.024.
Park JH, Ko Y, Kim WJ, Jang MS, Yang MH, Han MK, et al. Is asymptomatic hemorrhagic transformation really innocuous? Neurology. 2012;78:421–6. doi:10.1212/WNL.0b013e318245d22c.
Dzialowski I, Pexman JH, Barber PA, Demchuk AM, Buchan AM, Hill MD. Asymptomatic hemorrhage after thrombolysis may not be benign: prognosis by hemorrhage type in the Canadian Alteplase for Stroke Effectiveness Study registry. Stroke. 2007;38:75–9. doi:10.1161/01.STR.0000251644.76546.62.
Zhu Z, Fu Y, Tian D, Sun N, Han W, Chang G, et al. Combination of the immune modulator fingolimod with alteplase in acute ischemic stroke: a pilot trial. Circulation. 2015;132:1104–12. doi:10.1161/CIRCULATIONAHA.115.016371.
Schwamm LH, Holloway RG, Amarenco P, Audebert HJ, Bakas T, Chumbler NR, et al. A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2009;40:2616–34. doi:10.1161/STROKEAHA.109.192360.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by institutional grants.
Conflict of Interest
The authors declare that they have no competing interests.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Disclosures and Study Funding
None
Rights and permissions
About this article
Cite this article
Henninger, N., Fisher, M. Extending the Time Window for Endovascular and Pharmacological Reperfusion. Transl. Stroke Res. 7, 284–293 (2016). https://doi.org/10.1007/s12975-015-0444-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-015-0444-4