Abstract
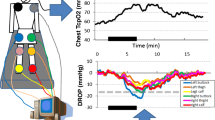
Previous studies reported that invasive physiological assessment for significance of the lesions in the patients with claudication under the condition of pharmacological hyperemia was important to identify the patients who will benefit from revascularization. However, the maximal hyperemic response in lower limb and the method to induce maximum dilatation of vascular bed in lower limb were not well established. The aim of this study was to investigate the range of maximal hyperemic response in lower limb of the normal subjects and to identify the ideal lower limb vasodilatory stimulation. Twelve limbs without stenotic lesions from 12 subjects (average age: 72 ± 6 years) were analyzed. Thermodilution-derived mean transit time (Tmn) was obtained at baseline and during pharmacological hyperemia with incremental dose of intra-arterial papaverine (10, 20, 30, and 40 mg) using a 0.014-inch pressure/temperature sensor-tipped wire in the superficial femoral artery (SFA). Percent increase in blood flow (%IBF) of lower limb was defined as the ratio between baseline Tmn and hyperemic Tmn. Mean ankle brachial index score of the subjects was 1.14 ± 0.09. The %IBF values were enhanced by papaverine in a dose-dependent manner. A dose of 30 mg of intra-arterial papaverine was sufficient to achieve maximum hyperemia (%IBF: range 219–769 %). In conclusion, the increase in blood flow of lower limb during maximal hyperemia varied between individuals and maximal hyperemia can be achieved with 30 mg of papaverine for the SFA lesion.





Similar content being viewed by others
References
Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Haris KA, Fowkes FG, TASC II Working Group. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007;43:S1–67.
Schillinger M, Sabeti S, Loewe C, Dick P, Amighi J, Mlekusch W, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006;354:1879–88.
Suzuki K, Iida O, Soga Y, Hirano K, Inoue N, Uematsu M, et al. Long-term results of the S.M.A.R.T. Control (TM) stent for superficial femoral artery lesions, J-SMART registry. Circ J. 2011;75:939–44.
Pijls NH, van Schaardenburgh P, Manoharan G, Boersma E, Bech JW, van’t Veer M, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER study. J Am Coll Cardiol 2007;49:2105–11.
Gould KL, Lipscomb K, Hamilton GW. Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am J Cardiol. 1974;33:87–94.
Brenner BJ, Raines JK, Darling RC, Austen WG. Measurement of systolic femoral arterial pressure during reactive hyperemia: an estimate of aortoiliac disease. Circulation. 1974;49–50:259–67.
Rådegran G, Calbet JA. Role of adenosine in exercise-induced human skeletal muscle vasodilatation. Acta Physiol Scand. 2001;171:177–85.
Kaufman SL, Fara JW, Udoff EJ, Harrington DP, White RI. Hemodynamic effects of vasodilators across iliac stenosis in dogs. Invest Radiol. 1979;14:471–5.
Pijls NH, De Bruyne B, Smith L, Aarnoudse W, Barbato E, Bartunek J, et al. Coronary thermodilution to assess flow reserve. Validation in humans. Circulation. 2002;105:2482–6.
Cruden NL, Lang NN, MacGillivray TJ, Uren NG, Fox KA, Newby DE. Vasomotor and fibrinolytic responses to kinin receptor agonists in the atherosclerotic human lower limb. Heart Vessels. 2012;27:179–85.
Subramanian R, White CJ, Rosenfield K, Bashir R, Almagor Y, Meerkin D, et al. Renal fractional flow reserve: a hemodynamic evaluation of moderate renal artery stenoses. Catheter Cardiovasc Interv. 2005;64:480–6.
Banerjee S, Badhey N, Lichtenwalter C, Varghese C, Brilakis ES. Relationship of walking impairment and ankle-brachial index assessments with peripheral arterial translesional pressure gradients. J Invasive Cardiol. 2011;23:352–6.
Van der Voort PH, van Hagen E, Hendrix G, van Gelder B, Bech JW, Pijls NH. Comparison of intravenous adenosine to intracoronary papaverine for calculation of pressure-derived fractional flow reserve. Cathet Cardiovasc Diagn. 1996;39:120–5.
Casella G, Leibig M, Schiele TM, Schrepf R, Seelig V, Stempfle HU, et al. Are high doses of intracoronary adenosine an alternative to standard intravenous adenosine for the assessment of fractional flow reserve? Am Heart J. 2004;148:590–5.
Vrolix M, Piessens J, De Geest H. Torsades de pointes after intracoronary papaverine. Eur Heart J. 1991;12:273–6.
McGeoch RJ, Oldroyd KG. Pharmacological options for inducing maximal hyperaemia during studies of coronary physiology. Catheter Cardiovasc Interv. 2008;71:198–204.
Kapoor N, Fahsah I, Karim R, Jevans AJ, Leesar MA. Physiological assessment of renal artery stenosis: comparisons of resting with hyperemic renal pressure measurements. Catheter Cardiovasc Interv. 2010;76:726–32.
Kroese AJ. The effect of inactivity on reactive hyperemia in the human calf: a study with strain gauge plethysmography. Scand J Clin Lab Invest. 1977;37:53–8.
Kroese AJ. The influence of age on reactive hyperemia in the human calf: a study with strain gauge plethysmography. Scand J Clin Lab Invest. 1977;37:105–9.
Râdegran G, Blomstrand E, Saltin B. Peak muscle perfusion and oxygen uptake in humans: importance of precise estimates of muscle mass. J Appl Physiol. 1999;87:2375–80.
Kroese AJ. Reactive hyperaemia in the calf of trained and untrained subjects: a study with strain gauge plethysmography. Scand J Clin Lab Invest. 1977;37:111–5.
Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease. Circulation. 2006;21:463–654.
Acknowledgments
The authors thank the staffs in the catheterization laboratory at Hyogo College of Medicine for their excellent assistance during the study.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miki, K., Fujii, K., Fukunaga, M. et al. Assessment of lower limb flow and adequate intra-arterial papaverine doses to achieve maximal hyperemia in elder subjects. Cardiovasc Interv and Ther 30, 227–233 (2015). https://doi.org/10.1007/s12928-014-0307-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-014-0307-z