Abstract
Introduction
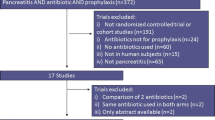
Prophylactic antibiotics are used frequently for acute pancreatitis (AP). Consensus guidelines do not recommend this currently, based on moderate quality evidence. In this study, we aimed to evaluate the antibiotic use pattern in AP in India and propose a risk-directed approach to antibiotic use in AP.
Material and Methods
This multicenter study was conducted from 1 May 2013 to 31 July 2013. Eleven participants from eight tertiary centers completed a questionnaire that captured patient demographics, etiology, admission status, presence of (peri)pancreatic necrosis, severity of pancreatitis, details of antibiotic use, and clinical outcomes (total hospital stay, persistent organ failure, need for ICU, total days in ICU, development of infections, in-hospital mortality).
Results
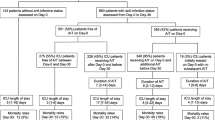
A total of 200 proformas were analyzed. Seventy-three (36.5 %) had acute necrotizing pancreatitis (ANP). Eighty-nine (44.5 %), 52 (26 %), and 55 (27.5 %) patients had mild AP (MAP), moderately severe AP (MSAP), and severe AP (SAP), respectively. Forty-five (22.5 %) patients developed infections (unifocal 29; multifocal 16). One hundred thirty-four (67 %) patients received antibiotics, of which 89 (66.4 %) received prophylactic, while 45 (33.6 %) received therapeutic antibiotics. The distribution of antibiotic use according to the severity of AP was 43 (48.3 %) in patients with MAP (prophylactic in 41; therapeutic in 2), 36 (69.2 %) in patients with MSAP (prophylactic in 29; therapeutic in 7), and 55 (100 %) in patients with SAP (prophylactic in 19; therapeutic in 36). Therapeutic antibiotics were prescribed based on culture and sensitivity in 21 (46.7 %) patients.
Conclusions
Despite nonrecommendation, prophylactic antibiotics are used frequently in AP. We emphasize on the need for multicenter randomized controlled trials on prophylactic antibiotics for AP based on a risk-directed approach, rather than a “blanket approach.”
Similar content being viewed by others
Introduction
In spite of an increasing understanding of the pathophysiology of acute pancreatitis (AP) over the past few years, there is still no specific treatment for the ailment. Fifteen percent (range 4 % to 47 %) of patients with AP develop (peri)pancreatic necrosis, of which 33 % (range 16 % to 47 %) develop infected necrosis (IN) [1]. Furthermore, it has also been reported that extra-pancreatic hospital that acquired infections in patients with AP can adversely impact morbidity and mortality [2]. Even though use of prophylactic antibiotics appears plausible based on these premises, randomized controlled trials (RCTs) on the use of prophylactic antibiotics in AP have yielded heterogeneous results, and recent double-blinded placebo-controlled trials and meta-analyses have failed to show significant preventive benefit [3–6]. One of the earlier meta-analysis did demonstrate some benefit from carbapenems in subgroup analysis [7], but it was subsequently found that studies with the highest quality had the least effect of antibiotics on pancreatic infection [8, 9]. Based on these studies (moderate quality evidence), recent consensus guidelines recommend against the use of prophylactic antibiotics and antifungals in patients with AP [10, 11]. However, in “real-life” clinical practice, use of prophylactic antibiotics in patients with AP is common both in India and abroad. This kind of practice often overlooks the known adversities of prolonged antibiotic use, such as development of bacterial resistance (which is becoming a major problem globally, including India) [12], development of fungal infections, and alteration of the gut microflora. This mandates the use of antibiotics in these patients in a rational and need-based manner.
In the current study, we aimed to evaluate the pattern of the use of antibiotics in patients with AP in India and attempted to propose a risk-directed approach to antibiotic use in these patients.
Patient and Methods
This was a multicenter study conducted from 1 May 2013 to 31 July 2013. The study was conceived at the Acute Pancreatitis module of Pancreas India in New Delhi in April 2013, with the primary objective to evaluate the antibiotic use pattern in patients with AP. Pancreas India is a yearly mentorship program that was initiated in 2012. This program is split into three modules (AP, chronic pancreatitis, and pancreatic neoplasm) across the year.
Participants of Pancreas India were invited to take part in the study, and a structured questionnaire was distributed among them. The questionnaire was supposed to be completed for consecutive patients admitted with a diagnosis of AP to the respective study centers during the study period. The parameters included in the questionnaire were the following: demographic details of the patients, etiology of AP, admission status (direct admission or transfer from another hospital), presence of (peri)pancreatic necrosis, severity of pancreatitis (mild, moderate, or severe), details of antibiotic use during previous (if data available) and current admissions, and clinical outcomes (total hospital stay, persistent organ failure (POF), need for care in the ICU, total days in the ICU, development of infections during hospitalization, in-hospital mortality). Following infections were recorded: infected pancreatic necrosis (IPN), pneumonia, ventilator-associated pneumonia (VAP), cholangitis, IV access site infections, urinary tract infection (UTI), and sepsis.
The study was coordinated and monitored from the Asian Institute of Gastroenterology. Fortnightly, communications were made with the participants, and timely updates on enrollment were obtained via e-mail. Completed questionnaires were returned by early August 2013, after which a database was generated and data analyzed. The analyzed data was presented and discussed at the Chronic Pancreatitis module of Pancreas India in Hyderabad in August 2013.
Definitions
Necrosis was defined as lack of enhancement of pancreatic parenchyma and/or presence heterogeneous and nonliquid densities of varying degrees. Severity of AP was defined as mild AP (MAP)—AP without organ failure and local complication; moderately severe AP (MSAP)—AP with organ failure (OF) that resolves within 48 h (transient OF) and/or local complications without persistent OF (POF); and severe AP (SAP)—AP with POF (OF that persists beyond 48 h). Local complications included acute peripancreatic fluid collections (APFC), pancreatic pseudocyst (PP), acute necrotic collection (ANC), and walled off necrosis (WON), as defined in the recently published Revised Atlanta Classification [13]. Organ failure was considered to be present if there was renal failure (serum creatinine level of >2 mg/dL even after adequate hydration or need for hemodialysis, circulatory failure (systolic blood pressure of less than 90 mmHg or need for pressor support), and/or respiratory failure (defined as PaO2 of <60 mmHg or support with BIPAP or ventilator) [14]. OF was defined as early if it developed within 2 weeks of onset of AP and late if it developed beyond 2 weeks.
Statistical analysis
A database was generated and descriptive statistical analysis performed in the JMP statistical software (version 9.0, SAS Institute, Cary, NC). Continuous variables were expressed as mean [95 % confidence interval (CI); range], and categorical variables were expressed as proportions (percentage).
Results
Out of the invited participants, 11 from 8 centers across India returned completed questionnaires of 208 patients. The study centers and number of patients from each center is depicted in Fig. 1. Eight questionnaires were duplicates; therefore, a total of 200 questionnaires were analyzed.
Patient characteristics and clinical outcomes
Out of 200 patients, 76 (38.4 %) were transferred from other centers and were referred by physicians, general surgeons, and general practitioners. Overall, 73 (36.5 %) patients had acute necrotizing pancreatitis (ANP). Eighty-nine (44.5 %), 52 (26 %), and 55 (27.5 %) patients had MAP, MSAP, and SAP, respectively. Data on severity of AP was not recorded for four patients. These patients were excluded from the analysis of antibiotic prescription. The mean (95 % CI; range) age in years was 38 years (36.9–41.2; 7–81), and 154 (77 %) patients were male. The most common etiology was alcohol [87 (43.5 %)] followed by gallstones [55 (27.5 %)]. An etiology could not be found in 39 (19.5 %) patients. Data on etiology was not recorded for ten (5 %) patients. A total of 45 (22.5 %) patients had infections, and 16 (8 %) died in-hospital. Six patients were referred to other hospitals (one patient to a government hospital due to financial constraints; one patient wanted to be referred to Amritha Institute as her relative was an employee there; four patients to their local hospitals due to logistical issues). Table 1 shows a detailed description of the patient characteristics and clinical outcomes.
Characteristics of infections among study patients
Forty-five (22.5 %) patients developed infections (unifocal in 29 and multifocal in 16). The distributions of infections among these patients were as follows: IPN—18; pneumonia—10; VAP—8, cholangitis—4; central line infection—1; UTI—8; and sepsis—13. Prevalence of IPN among patients with ANP was 24.7 % (18/73). Infection was diagnosed in the ward in 24 patients while in the ICU in 21 patients.
Organisms were detected in culture of samples (blood/tracheobronchial aspirate/percutaneous drain fluid/urine) from 21 patients. Culture revealed a single organism in 13 (61.9 %) patients while multiple organisms in the remaining 8 (38.1 %). The most common organism was E. coli, which was seen in nine (42.9 %) patients, followed by Klebsiella sp. in seven (33.3 %), and Acinetobacter sp. in five (23.8 %) patients each.
Table 2 shows the details of patients who had multifocal infections and polymicrobial growth in culture.
Characteristics of patients who died in-hospital
Table 3 describes the salient features of the patients who died in-hospital. A total of 16 (8 %) patients died during the study period. The mean (95 % CI; range) duration between admission and death in these patients was 14.5 days (6.9–22.01; range 1–37). Fourteen (87.5 %) of these patients had POF, 9 (56.3 %) had infections, and the cause of death was early OF in 7/16 (43.7 %) patients while sepsis with late OF in 7/16 (43.7 %) patients. The cause of death was not recorded for two patients.
Overall antibiotic use
Data on antibiotic prescription during first hospitalization was available for 55 out of the 76 transferred patients. Fifty-one (92.7 %) of these patients received prophylactic antibiotics while four (7.3 %) received therapeutic antibiotics. Prophylactic antibiotics were continued in 27 (52.9 %) of these patients during current hospitalization. Out of these 27, 5 patients had MAP, 13 had MSAP, and 9 had SAP.
During the current hospitalization, a total of 134 (67 %) patients received antibiotics, of which 89 (66.4 %) received prophylactic while 45 (33.6 %) received therapeutic antibiotics. Three of the contributing centers had an institutional therapeutic antibiotic protocol that they followed while treating their patients. The distribution of antibiotic use according to the severity of AP was as follows: 43 (48.3 %) in patients with MAP (prophylactic in 41 and therapeutic in 2), 36 (69.2 %) in patients with MSAP (prophylactic in 29 and therapeutic in 7), and 55 (100 %) in patients with SAP (prophylactic in 19 and therapeutic in 36). Mean (95 % CI; range) durations (in days) of treatment with prophylactic and therapeutic antibiotics were 6.3 (95 % CI 5.3–7.3; range 1–30) and 13 (95 % CI 8.6–18.01; range 4–60), respectively.
Prophylactic antibiotics used during current hospitalization
Table 4 shows the distribution of the classes of prophylactic antibiotics during current admission. Majority of patients with MAP [23 (56.1 %)] received a single third-generation cephalosporin while seven (17.1 %) received multiple antibiotics. Among the patients with MSAP, 11 (37.9 %) received multiple prophylactic antibiotics that included at least a third-generation cephalosporin or a beta-lactam or a carbapenem in 9 (31 %) patients. Of the patients with SAP, 11 (57.9 %) patients received multiple prophylactic antibiotics that included at least one third-generation cephalosporin or a carbapenem or a glycopeptide. Two patients with MSAP and one with SAP received prophylactic aminoglycosides antibiotics. Multiple antibiotics were prescribed either together or individually at different time points.
Therapeutic antibiotics used during current hospitalization
Therapeutic antibiotics were prescribed based on culture and sensitivity reports in 21 out of 45 (46.7 %) patients, while it was empirical in 24 (53.3 %). Table 5 shows the details of the class of empirical antibiotics that were used based on the individual sites of infections.
Discussion
In this study, we have evaluated the pattern of antibiotic use in patients with AP in India in a prospective multicenter study setting. The salient findings were as follows: (a) Overall, 134 patients received antibiotics of which 66.4 % was prophylactic; (b) 46.1 % patients with MAP received prophylactic antibiotics; and (c) patients with MSAP and SAP received multiple prophylactic antibiotics including aminoglycosides.
Prophylactic antibiotics and antifungals are not recommended in AP according to current guidelines [10, 11]. This recommendation was based on systematic reviews and meta-analyses [3–6]. However, the studies evaluated were heterogeneous in terms of methodologic quality, selection criteria, treatment duration, antibiotic selection, and outcome measures [6]. Subgroup analysis in the meta-analysis by Heinrich et al. showed a protective effect of carbapenems against infected necrosis [7]. On the other hand, Mazaki et al. and deVries et al. reported that trials with higher quality failed to show any preventive benefit [8, 9]. However, even though guidelines do not recommend prophylactic antibiotics, based on the disparate data and moderate quality evidence, role of prophylactic antibiotics cannot be conclusively ruled out at present. At the same time, a “blanket cover” of prophylactic antibiotics for most patients with AP too does not appear justified. For example, there is no rationale for the use of higher generation antibiotic prophylaxis for patients with MAP. It has been shown that nearly 5 % of patients with MAP can have extra-pancreatic infection [15]. A more rational approach to deal with these infections would be to use targeted treatment specific to the infection rather than using a blanket cover of prophylactic antibiotics. The major dilemma in the use of prophylactic antibiotics in clinical practice lays with MSAP and SAP, which are characterized by the presence of (peri)pancreatic necrosis and organ dysfunction/failure. In the current study, pancreatic necrosis was observed in 36.5 % patients, which was somewhat higher than population-based series. This could be due to a referral bias since all the study centers were tertiary care referral centers and could explain the high prevalence of the use of prophylactic antibiotics. Nevertheless, as long as consensus antibiotic guidelines based on high-quality evidence are nonexistent for these patients, a risk-directed approach could be a rational way to use prophylactic antibiotics, instead of the currently prevalent manner of using antibiotic prophylaxis for majority of such patients.
Use of a short course of prophylactic carbapenem antibiotics for patients with ANP with POF appears justified since these patients are at a higher risk of developing infected necrosis, which is associated with a high rate of delayed (after 2 weeks) mortality [6]. Other choices of antibiotics include quinolones, high-dose cephalosporins, and metronidazole, due to the good penetration of these into the pancreas and demonstration of efficacy in clinical trials [16–18]. Another potential group of patients for antibiotic prophylaxis could be those who appear septic, and a source of infection is being sought for by blood cultures and other investigations [6]. Even the recent IAP/APA guidelines suggest a potential role of prophylactic antibiotics for these patients [11]. However, prophylactic antibiotics should be started in these patients only after the investigation for identification of the source has been started. Another rational way to begin prophylactic antibiotics in patients with ANP is a biomarker-based approach. It was shown recently that any rise in blood urea nitrogen (BUN) at 24 h of admission with AP was associated with a 4.3-fold increase risk of death [19], and a rise in BUN by 5 mg/dL within 48 h of admission was associated with subsequent development of infected necrosis with an odd’s of 5.37 (95 % CI 0.71–8.47; p = 0.007) on multivariable analysis [20]. Therefore, patients with increasing BUN within 24–48 h after admission could form another potential group that might be benefitted from prophylactic antibiotics. Furthermore, procalcitonin has been evaluated in several studies as a predictor of SAP and IPN [21, 22]. In a systematic review and meta-analysis, procalcitonin emerged as a good predictor of IPN with a sensitivity and specificity of 0.8 (95 % CI 0.71–0.88) and 0.91 (95 % CI 0.87–0.94), respectively, with low heterogeneity. However, the procalcitonin cutoff and timing of highest value were variable [23]. Nevertheless, these four could be potential rational indications for the use of prophylactic antibiotics and need to be evaluated further under randomized controlled settings. It would be important to be vigilant on the duration of antibiotic prophylaxis, and care should be taken to avoid prophylaxis for a prolonged period of time.
The current study was not designed to evaluate the effect of prophylactic or therapeutic antibiotics on infections in patients with AP. This was one of the limitations of the study. Moreover, the timing of diagnosis of infections including IPN and the rate of conversion of prophylactic antibiotics to therapeutic antibiotics was not recorded. Another limitation of the study was the nonuniformity in proportion of cases from different study centers. While the highest proportion of cases (36 %) was from the coordinating center, other centers contributed 4 % to 12 % of cases. Nevertheless, this study is important since, to our knowledge, it is first from the country that has evaluated the pattern of antibiotic use in patients with AP. It was performed in multiple high-volume tertiary care academic centers across the country. Furthermore, the data on the pattern of infections associated with AP in Indian patients is another strength of this multicenter study.
In conclusion, besides prescription of prophylactic antibiotics and antifungals in patients with MSAP and SAP (possibly due to severity of the disease), a substantial proportion of patients with even MAP received antibiotic prophylaxis. We emphasize the need for high-quality multicenter RCTs on the use of prophylactic antibiotics in AP on the basis of a risk-directed approach, rather than a “blanket approach.” This could culminate in identification of rational indications of antibiotic prophylaxis in AP.
References
Banks PA, Freeman ML. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101:2379–400.
Wu BU, Johannes RS, Kurtz S, Banks PA. The impact of hospital-acquired infection on outcome in acute pancreatitis. Gastroenterology. 2008;135:816–20.
Isenmann R, Runji M, Kron M, et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gasrtoenterology. 2004;126:997–1004.
Dellinger EP, Tellado JM, Soto NE, et al. Early antibiotic treatment for severe acute necrotizing pancreatitis: a randomized double-blinded, placebo-controlled study. Ann Surg. 2007;245:674–83.
Gascia-Barrasa A, Borobia FG, Pallares R, et al. A double-blind, placebo-controlled trial of ciprofloxacin prophylaxis in patients with acute necrotizing pancreatitis. J Gastrointest Surg. 2009;13:768–74.
Talukdar R, Vege SS. Recent developments in acute pancreatitis. Clin Gastroenterol Hepatol. 2009;7:S3–9.
Heinrich S, Schafer M, Rousson V, Clavien PA. Evidence-based treatment of acute pancreatitis: a look at established paradigms. Ann Surg. 2006;243:154–8.
Mazaki T, Ishii Y, Takayama T. Meta-analysis of prophylactic antibiotic use in acute necrotizing pancreatitis. Br J Surg. 2006;93:674–84.
drVries AC, Besselink MG, Buskens E, et al. Randomized controlled trials of antibiotic prophylaxis in severe acute pancreatitis: relationship between methodology and outcome. Pancreatology. 2007;7:531–8.
Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology Guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–15.
Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13 4 Suppl 2:e1–15.
Morrissey I, Hackel M, Badal R, et al. A review of ten years of the study of monitoring antimicrobial resiatance trends (SMART) from 2002-2011. Pharmaceuticals. 2013;6:1335–46.
Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis-2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–11.
Talukdar R, Sharma M, Deka A, et al. Utility of the “Harmless Acute Pancreatitis Score” in predicting a non-severe course of acute pancreatitis: a pilot study in an Indian cohort. Indian J Gastroenterol. 2014;33:316–21.
Talukdar R, Bhattacharyya A, Rao B, et al. Validation of the revised Atlanta definitions of severity of acute pancreatitis: have all loose ends being tied? Pancreatology. 2014;14: 257–62.
Beger HG, Bittner R, Block S, et al. Bacterial contamination of pancreatic necrosis: a prospective clinical study. Gastroenterology. 1986;91:433–7.
Villatoro E, Bassi C, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev. CD002941.
Tenner S. Initial management of acute pancreatitis: critical decision making in the first 72 hours. Am J Gastroenterol. 2004;99:2489–94.
Wu BU, Johannes RS, Sun X, et al. Early changes in blood urea nitrogen predict mortality in acute pancreatitis. Gastroenterology. 2009;137:129–35.
Talukdar R, Nechutova H, Clemens M, Vege SS. Could rising BUN predict the future development of infected pancreatic necrosis? Pancreatology. 2013;13:355–9.
Quenot JP, Luyt CE, Roche N, et al. Role of biomarkers in the management of antibiotic therapy: an expert panel review II: clinical use of biomarkers for initiation or discontinuation of antibiotic therapy. Ann Intensive Care. 2013;3:21.
Talukdar R, Reddy DN. Predictors of adverse outcomes in acute pancreatitis: new horizons. Indian J Gastroenterol. 2013;32:143–51.
Mofidi R, Suttie SA, Patil PV, et al. The value of procalcitonin at predicting the severity of acute pancreatitis and development of infected pancreatic necrosis: systematic review. Surgery. 2009;146:72–81.
Conflict of interest
RT, PI, HPC, RD, SS, HJ, KRP, LM, SM, JKP, BT, AC, AK, DNR, GVR, HR, NB, PG, and RK declare that they have no conflict of interest.
Ethics statement
The study was performed in a manner to conform with the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning Human and Animal Rights, and that the authors followed the policy concerning Informed Consent as shown on springer.com.
Financial disclosure
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Talukdar, R., Ingale, P., Choudhury, H.P. et al. Antibiotic use in acute pancreatitis: An Indian multicenter observational study. Indian J Gastroenterol 33, 458–465 (2014). https://doi.org/10.1007/s12664-014-0494-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-014-0494-7