Abstract
Purpose
Elevated glycosylated hemoglobin (HbA1c) is often found in surgical patients with no history of diabetes. The purpose of this prospective observational study was to determine if elevated preoperative HbA1c is associated with postoperative hyperglycemia in non-diabetic surgical patients and to identify predictors of elevated HbA1c.
Methods
This study included 257 non-diabetic adults scheduled for inpatient surgery. Preoperatively, capillary blood glucose (CBG) and HbA1c were measured and patients completed the Canadian Diabetes Risk Questionnaire (CANRISK). Capillary blood glucose was measured for two days or until hospital discharge at the following time points: postoperatively, before all meals, and at 22:00 hr. The mean CBG and incidence of hyperglycemia were compared between HbA1c levels: Group I < 6.0%, Group II 6.0-6.4%, and Group III ≥ 6.5%.
Results
The mean postoperative glucose levels at all time points were significantly higher in Group III compared with Groups I and II (P < 0.01). At least one episode of hyperglycemia (CBG ≥ 10.0 mMol·L−1) occurred in 61% (11/18) of patients in Group III vs 11% (23/209) of patients in Group I (relative risk, 5.55; 95% confidence interval [CI], 3.26 to 9.47; P < 0.001). Elevated glycosylated hemoglobin ≥ 6.0% was found in 31% (33/107) of those with a high CANRISK score. The best predictors of postoperative hyperglycemia were preoperative CBG > 6.9 mMol·L−1 [diagnostic odds ratio (OR) (reference < 6.0 mMol·L−1), 4.16; 95% CI, 1.57 to 10.98; P = 0.004], HbA1c ≥ 6.0% [OR (reference < 6.0%), 3.00; 95% CI, 1.39 to 6.49; P = 0.005], and HbA1c ≥ 6.5% [OR (reference < 6.5%), 13.45; 95% CI, 4.78 to 37.84; P <0.001].
Conclusions
Elevated HbA1c is associated with higher mean postoperative glucose levels in patients with no diabetic history. The CANRISK score is a strong predictor of elevated HbA1c, while CBG and HbA1c are both predictors of postoperative hyperglycemia.
Résumé
Objectif
Une hémoglobine glycosylée (HbA1c) élevée est souvent observée chez des patients chirurgicaux sans antécédents de diabète. L’objectif de cette étude observationnelle prospective était de déterminer si une HbA1c préopératoire élevée est associée à une hyperglycémie post opératoire chez des patients chirurgicaux non diabétiques et d’identifier les facteurs prédictifs d’une HbA1c élevée.
Méthodes
Cette étude a inclus 257 adultes non diabétiques devant être hospitalisés pour chirurgie. La glycémie capillaire (CBG) et l’HbA1c ont été mesurées en préopératoire et les patients ont rempli le questionnaire canadien sur le risque de diabète (CANRISK). La glycémie capillaire a été mesurée pendant deux jours ou jusqu’au congé de l’hôpital aux moments suivants : en post opératoire, avant chaque repas et à 22 h. La CBG moyenne et l’incidence des hyperglycémies ont été comparées en fonction des taux d’HbA1c : Groupe I < 6,0 %, Groupe II 6,0 % à 6,4 % et Groupe III ≥ 6,5 %.
Résultats
Les taux moyens de glucose postopératoires ont été significativement plus élevés à toutes les échéances dans le Groupe III comparativement aux Groupes I et II (P < 0,01). Au moins un épisode d’hyperglycémie (CBG ≥ 10,0 mmol· L−1) est survenu chez 61 % (11/18) des patients du Groupe III contre 11 % (23/209) des patients du Groupe I (risque relatif, 5,55; intervalle de confiance à 95 % [IC] : 3,26 à 9,47; P = 0,001). Une hémoglobine glycosylée élevée ≥ 6,0 % a été retrouvée chez 31 % (33/107) des patients ayant un score CANRISK élevé. Les éléments prédictifs d’une hyperglycémie post opératoire étaient : CBG préopératoire > 6,9 mmol· L−1 [rapport de cotes du diagnostic (OR) (référence < 6,0 mmol· L−1), 4,16; IC à 95 %, 1,57 à 10,98; P = 0,004], HbA1c préopératoire ≥ 6,0 % [OR (référence < 6,0 %), 3,00; IC à 95 %, 1,39 à 6,49; P = 0,005], et HbA1c préopératoire ≥ 6,5 % [OR (référence < 6,5 %), 13,45; IC à 95 %, 4,78 à 37,84; P <0,001].
Conclusions
Une HbA1c élevée est associée à des taux moyens de glucose postopératoire plus élevés chez les patients sans antécédents diabétiques. Le score CANRISK est un puissant élément prédictif d’HbA1c élevée, tandis que la CBG et l’HbA1c préopératoires sont toutes deux des éléments prédictifs d’hyperglycémie postopératoire.
Similar content being viewed by others
Diabetes is currently reaching near epidemic levels, with approximately 2 million Canadians living with the disease at an annual cost of 9 billion dollars.1 Due to the lack of symptoms, particularly in its early stages, type 2 diabetes may go undiagnosed, with up to one-third of those unaware they have the disease.1 Surgical patients with diabetes require greater use of healthcare resources and are at an increased risk of morbidity and mortality in the postoperative period.2-7 This may be due to associated comorbidities, such as cardiovascular disease, but may also be more directly due to the presence of elevated blood glucose levels.8
Studies have shown that hyperglycemia is common in both medical and surgical hospital inpatients.6,9,10 Postoperative hyperglycemia increases the risk of surgical site infections (SSI) as a result of inflammation and decreased immune function.11-14 Furthermore, in non-cardiac surgery settings, an increased need for re-operation, longer hospital length of stay, and mortality have all been associated with postoperative hyperglycemia.3,8,15 Although anesthesiologists assess patients preoperatively for underlying medical conditions, such as hypertension and obstructive sleep apnea,16 screening for diabetes is not routinely conducted in the perioperative setting. Interestingly, screening in primary care is commonplace and recommended using either fasting blood glucose (FBG) or glycosylated hemoglobin (HbA1c) testing for individuals ≥ 40 yr of age or deemed to be high risk based on their score on a validated screening tool such as the Canadian Diabetes Risk Questionnaire (CANRISK).17
Prediabetes corresponds with a FBG of 6.1-6.9 mMol·L−1 and/or HbA1c levels of 6.0-6.4%, with diabetes corresponding with a FBG > 6.9 mMol·L−1 and/or a HbA1c ≥ 6.5%. Nevertheless, FBG requires an eight-hour fast and is not easily tested during the preoperative clinic visit or on the morning of surgery where patients are now encouraged to drink clear carbohydrate-containing fluids up to two hours before surgery.18 Glycosylated hemoglobin testing is easily performed yet still not commonly ordered preoperatively for patients with no history of diabetes. It has been shown, however, that > 20% of surgical patients with no diabetic history are at high risk for developing diabetes, while 4% would have a provisional diagnosis of diabetes based on their HbA1c test results.19
While elevated HbA1c is common among hospitalized patients, it has not been clearly established that this is predictive of postoperative hyperglycemia in patients undergoing non-cardiac surgery.19,20 Recent studies of abdominal surgery suggest that elevated HbA1c is associated with major cardiac complications, while hyperglycemia is more likely to be associated with SSI, emphasizing the importance of identifying both of these risk factors.2,14 If this were indeed the case, widespread HbA1c screening and postoperative glucose testing would each identify different types of high-risk patients to target for intervention strategies. Nevertheless, more studies are needed to determine which patients should be screened and if the correlations between HbA1c and hyperglycemia are seen in diverse surgical populations.
Accordingly, we hypothesized that elevated preoperative HbA1c is associated with higher mean postoperative glucose levels among non-diabetic patients having a variety of elective surgical procedures and that there is a higher incidence of clinically significant postoperative hyperglycemia in patients with elevated vs normal preoperative HbA1c levels. Our additional objectives were to explore other factors that may predict elevated HbA1c or postoperative hyperglycemia.
Methods
This prospective cohort study was approved for ethical compliance by the Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (ANAE-253-14) in May 2014. Adults presenting for elective surgery at Kingston General Hospital and Hotel Dieu Hospital (Queen’s University, Kingston, ON, Canada) from June 5 to August 2, 2014 were approached to participate in this prospective observational study. Informed consent was obtained in the Same Day Admission Centre immediately preoperatively. The study dates were chosen to allow full-time recruitment by study staff. Patients ≥ 18 yr of age with no history of diabetes and scheduled for elective surgery requiring postoperative hospital admission were eligible to participate. Exclusion criteria included planned admission to a high dependency unit, cardiac surgery, and the use of oral hypoglycemic agents or insulin.
In the Same Day Admission Centre, baseline demographic and clinical data were collected on consenting patients who then completed the self-administered CANRISK (Appendix 1) prior to having their glucose levels tested. The Public Health Agency of Canada developed the CANRISK in consultation with Canadian and international experts to identify adults with prediabetes and undiagnosed type 2 diabetes.21 The 12-item questionnaire was validated for assessing diabetes risk on a national scale for Canada’s multi-ethnic population in 2011.22 It is available in paper and electronic form and can be easily self-administered in just a few minutes.
On the day of surgery, blood was obtained for HbA1c testing (VARIANT™ II HBA2/HbA1c Dual Program; Bio-Rad Laboratories, Montreal, QC, Canada). Caregivers were blinded to the HbA1c findings, and test results were mailed directly to study staff one week following the procedure. Capillary blood glucose (CBG) was measured (StatStrip; Nova Biomedical, Waltham, MA, USA) preoperatively. Since patients are now encouraged to drink clear carbohydrate-containing fluids up to two hours before surgery,18 this measurement was called “preoperative CBG” rather than fasting blood glucose. Postoperatively, nursing staff were requested to measure CBG upon the patients’ arrival to the postanesthesia care unit (PACU), before each meal time, and at 22:00 hr for two days or until discharge. The StatStrip measures CBG as a plasma glucose corrected for hematocrit. Intraoperative data collection included the use of intravenous steroids and procedure duration. The anesthetic, analgesic, and surgical management was at the discretion of the attending physicians. All patients received either an oral diet or intravenous fluids containing carbohydrates postoperatively as determined by the surgical service. All data were collected by study staff who were blinded to the HbA1c results.
Abnormal results protocol
The surgical service was notified if the CBG was >10.0 mMol·L−1 on two or more occasions postoperatively. An information sheet with general recommendations for management of hyperglycemia was provided to the surgical service and management was at their discretion (Appendix 2). For HbA1c ≥ 6.0%, the results were faxed to the primary care physician’s office along with suggestions for further investigations and management.
Variables
The primary outcome was mean CBG (mMol·L−1) before breakfast on postoperative day 1 (POD1). This variable was chosen as it was most likely to have been captured for all patients, and it would reflect the effects of the surgical stress response. The secondary outcome was the incidence of postoperative hyperglycemia, which we defined as at least one occurrence of CBG ≥10.0 mMol·L−1. We chose this a priori based on the current definitions of postoperative hyperglycemia which range from 7.8-11.1 mMol·L−1.3,5,6,8-10,12,14,15,20,23-25 As we could not guarantee that the CBG measurements were always pre-meal, our definition of hyperglycemia also took into account clinical practice guidelines that recommend a pre-meal glucose target < 7.8 mMol·L−1 and random blood glucose < 10.0 mMol·L−1 for patients with non-critical illness.10
The primary exposure variable of interest was HbA1c level, defined as normal < 6.0% (Group I), very high risk for diabetes (i.e., prediabetes) 6.0-6.4% (Group II), and diagnostic for diabetes ≥ 6.5% (Group III).23 Patients were also stratified into diabetic risk categories using the CANRISK, which provides a ten-year risk of developing type 2 diabetes. Low risk is defined as a score of < 21, moderate risk is 21-32, and high risk is a score of ≥ 33 (Appendix 1).18 Additional covariates included POD0 morning glucose, age, sex, race (self-reported), smoking status, body mass index (using height and weight measured in the preoperative clinic), physical activity level, family history of diabetes, American Society of Anesthesiologists classification, surgical procedures, duration of surgery, medications (chart review), and comorbidities (determined by the attending anesthesiologist).
Sample size and statistical analysis
Sample size was calculated to assess for a statistically significant difference in mean CBG before breakfast on POD1. At least 105 patients were required to detect differences in mean CBG between the three groups [Group I = 6.0 mMol·L−1; Group II = 6.5 mMol·L−1; Group III = 7.5 mMol·L−1; common standard deviation (SD) = 2.0] using an alpha = 0.05 and power = 0.8. The statistical analyses were conducted using SPSS® version 21 (IBM Corp., Armonk, NY, USA). Frequencies and percentages were calculated for categorical data. Surgical duration was found to be skewed based on a visual inspection of the distribution of continuous data, and therefore, median and interquartile range [IQR] were calculated. All other continuous data were normally distributed and means and standard deviations (SD) were calculated.
Statistically significant differences in mean blood glucose levels across HbA1c levels were assessed at each time point using one-way analysis of variance (ANOVA). Repeated measures ANOVA could not be conducted due to the high frequency of missing CBG results. Therefore, to account for multiple testing when examining the difference in mean values between the three groups over the 12 data collection time points, statistical significance was set at P < 0.001 (i.e., 0.05/36). The incidence (defined as the first time a patient had a CBG ≥ 10.0 mMol·L−1) and prevalence (defined as each time a patient had a CBG ≥10.0 mMol·L−1) of CBG at each time point were calculated. Due to the high rate of missing CBG results postoperatively, exploratory analysis was conducted using the incidence of postoperative hyperglycemia (at least one postoperative occurrence of CBG ≥ 10.0 mMol·L−1) as the dependent variable for the inferential analysis. The Chi square test, Student’s t test, or Mann-Whitney U test was used to assess for statistically significant differences in postoperative hyperglycemia (CBG ≥ 10 mMol·L−1), stratified by HbA1c category, CANRISK, and demographic and clinical covariates. In order to examine potential predictors of elevated HbA1c, a similar analysis was conducted with HbA1c ≥ 6.0% as the dependent variable, with groups collapsed into two categories, normal HbA1c (< 6.0%) vs abnormal HbA1c (≥ 6.0%). Subgroup analysis was conducted on Group I (HbA1c < 6.0%) to assess for potential risk factors for postoperative hyperglycemia in this low risk for diabetes group. Relative risk (RR) and 95% confidence intervals (CI) were used to measure the strength and precision of the potential risk factors. Sensitivity, specificity, predictive values, likelihood ratios, and diagnostic odds ratios were calculated for potential predictors of postoperative hyperglycemia and elevated HbA1c (≥ 6.0%). Potential predictors were identified as those with a P < 0.10 (two-sided) in the bivariable analyses. The diagnostic odds ratio is the most useful measure to compare the validity of the predictor variables as it combines specificity and sensitivity and it is not affected by prevalence. The diagnostic odds ratio (OR) is the ratio of having a positive screen if the condition is truly present relative to the odds of having a positive screen if the condition is not present.
Results
Details regarding patient recruitment are presented in Fig. 1. In total, 275 patients were followed postoperatively. Nevertheless, 18 patients who agreed to participate in the study were excluded from the analysis for the following reasons: two due to a clotted sample, eight due to early discharge, and eight due to no postoperative CBG measures. Of the remaining 257 patients, there were 209/257 (81.3%) patients in Group I (HbA1c < 6.0%), 30/257 (11.7%) patients in Group II (HbA1c = 6.0-6.4%), and 18/257 (7.0%) patients in Group III (HbA1c ≥ 6.5%). Nineteen percent (48/257) of patients had elevated HbA1c, and 7.0% (18/257) had HbA1c levels consistent with a provisional diagnosis of diabetes. Forty-two percent (107/257) had CANRISK scores suggesting a high risk for diabetes. There were no significant differences between mean (SD) HbA1c levels in patients with early discharge, the 18 patients excluded from further analysis, and those who remained in the analysis [5.7 (0.6)%, 5.7 (0.4)%, 5.6 (0.6)%, respectively; F = 0.09; P = 0.92].
Potential predictors of elevated HbA1c
Glycosylated hemoglobin was collapsed into two categories, normal HbA1c (< 6.0%) vs abnormal HbA1c (≥ 6.0%). Those in the high HbA1c group had significantly higher CANRISK scores and preoperative CBGs (Table 1). The patients with a high CANRISK score had a greater risk of having elevated HbA1c than patients with a low CANRISK score (RR, 14.80; 95% CI, 2.1 to 105.1). The relative risk (RR) of elevated HbA1c was 8.97 (95% CI, 5.3 to15.3) in patients with preoperative CBG > 6.9 mMol·L−1 compared with those with preoperative CBG < 6.1 mMol·L−1. Other significant predictors (bivariable analysis) of HbA1c ≥ 6.0% were age, body mass index, and family history of diabetes.
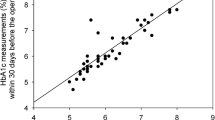
Glycosylated hemoglobin and prediction of postoperative glucose level
The mean (SD) CBG before breakfast on POD1 was 6.0 (1.1) mMol·L−1 for Group I, 6.7 (1.2) for Group II, and 9.2 (2.0) for Group III (P < 0.001). Fig. 2 displays mean blood glucose levels preoperatively and at each time point stratified by HbA1c Group and shows the prevalence and incidence of hyperglycemia (CBG ≥10.0 mMol·L−1) at each time point. The majority of new cases (i.e., incidence) of hyperglycemia occurred on POD0, with a small number of new cases occurring on POD1. No new cases of hyperglycemia occurred after dinner on POD1. The frequency of missing data and the number of patients discharged are presented by group for each time point in Table 2. By POD2 dinner, 53% (137/257) of patients had been discharged. The frequency of missing postoperative CBG measures for patients remaining in h ospital ranged from 3.1% (8/257) postoperatively in the PACU to 28.0% (52/186) before POD2 breakfast. There were overall significant differences in mean CBG across HbA1c categories at each time point (P < 0.001), except POD0 22:00 hr (P = 0.011). Post hoc comparisons revealed no significant differences between Group I and Group II; however, there were significantly higher CBG levels across all time points for Group III vs Group I (P < 0.001). Six patients had two or more measures of CBG ≥ 10.0 mMol·L−1. Only one study patient received insulin, which was given after POD2 dinner. This resulted in only one CBG measurement (POD2 22:00 hr) taken after insulin therapy during the entire study. None of the patients received insulin or dextrose-containing intravenous fluids intraoperatively.
Mean blood glucose levels (mMol·L−1) stratified by preoperative HbA1c level and prevalence and incidence of hyperglycemia (CBG ≥ 10.0 mmol·L−1) preoperatively, postanesthetic care unit (PACU), before meals, and 22:00 hr. CBG = capillary blood glucose; POD = postoperative day; SDAC = Same Day Admission Centre
There was a significant difference in the incidence of postoperative hyperglycemia across HbA1c categories [Group III 61.1% vs Group 1 11.0%; RR, 5.6; 95% CI, 3.3 to 9.5 (Group 1 reference); Chi square, 37.7; P = 0.001]. Patients with HbA1c ≥ 6.5% had an increased risk of having postoperative hyperglycemia compared with those with normal HbA1c (RR, < 5.6; 95% CI, 3.3 to 9.5) (Table 3). Patients with a high preoperative CBG (> 6.9 mMol·L−1) were also significantly more likely to have postoperative hyperglycemia compared with those with preoperative CBG < 6.1 mMol·L−1 (RR, 3.2; 95% CI, 1.5 to 6.5). Family history of diabetes was also a significant predictor of postoperative hyperglycemia.
Postoperative hyperglycemia occurred in 11.0% (23/209) of patients with normal HbA1c (Table 4). Compared with the low CANRISK groups (4/47 = 8.5%), there was no difference in the risk of postoperative hyperglycemia for the moderate (8/66 = 12.1%) (RR, 1.16; 95% CI, 0.75 to 1.79) or high (10/74 = 13.5%) (RR, 1.59; 95% CI, 0.53 to 4.8) CANRISK groups. There was, however, a greater risk of postoperative hyperglycemia with preoperative CBG > 6.9 mMol·L−1 compared with preoperative CBG < 6.1 mMol·L−1 (RR, 3.9; 95% CI, 1.12 to13.3).
Validity of potential predictors of postoperative hyperglycemia and elevated HbA1c
Based on the diagnostic OR, the best predictors of postoperative hyperglycemia were preoperative CBG > 6.9 mMol·L−1 [OR (reference < 6.0 mMol·L−1), 4.16; 95% CI, 1.57 to -11.0; P = 0.004], HbA1c ≥ 6.0% [OR (reference < 6.0%), 3.0; 95% CI, 1.39 to -6.5; P = 0.005], and HbA1c ≥ 6.5% [OR (reference < 6.5%), 13.5; 95% CI, 4.8 to -37.8; P < 0.001] (Table 5). The best predictors of elevated HbA1c ≥ 6.0% were moderate to high CANRISK scores [OR for CANRISK scores ≥ 21 (reference < 21), 14.8; 95% CI, 1.98 to110.2 and OR for CANRISK scores ≥ 33 (reference < 33), 4.2; 95% CI, 2.0 to 8.7] and preoperative CBG [OR for > 6.9 mMol·L−1 (reference < 6.1 mMol·L−1), 4.2; 95%, CI 1.6 to 11.0] (Table 5).
Discussion
Our findings suggest that as many as one in five non-diabetic surgical patients could indeed have abnormal glucose control. The interaction between and predictors of elevated HbA1c, CANRISK scores, and postoperative hyperglycemia are complex. Nineteen percent (48/257) of patients scheduled for surgery with an overnight admission to a ward bed had HbA1c above normal (≥ 6.0%), with 7% (18/257) of patients meeting diagnostic criteria for diabetes, confirming that undiagnosed dysglycemia is common among non-cardiac surgical patients. Mean CBG levels were significantly higher in patients with HbA1c ≥ 6.5% at all time points in the 48 hr postoperatively compared with patients with normal HbA1c values. Furthermore, 61% (11/18) of patients with HbA1c ≥ 6.5% had at least one episode of clinically significant hyperglycemia (CBG ≥10.0 mMol·L−1) compared with 7% (2/30) of those with HbA1c values of 6.0-6.4% and 11% (23/209) of those with normal HbA1c. Despite higher average blood glucose values, patients with prediabetic HbA1c levels (6.0-6.4%) did not experience significantly more episodes of clinically significant hyperglycemia than patients with normal HbA1c levels.
The finding of a high prevalence of postoperative hyperglycemia has clinical implications beyond that of controlling glucose levels. In a cohort study of over 40,000 patients, Kotagal et al. showed that the risk of adverse events was linked to hyperglycemia in patients with no prior history of diabetes but not to the condition in known diabetic patients.26 The reasons for this difference in adverse events between these two groups are not well understood but likely due to undertreatment with insulin in patients with no prior diagnosis of diabetes or possibly an increase in surgical stress leading to hyperglycemia. Kwon et al. studied over 11,000 patients and showed that perioperative hyperglycemia was associated with an increased risk of infection, re-operation, and death in general surgery patients with and without a previous diagnosis of diabetes.3 Nevertheless, the risk of adverse events in patients with hyperglycemia who were treated with insulin was similar to that in patients with normal blood glucose. These studies suggest that identifying and treating elevated blood glucose levels might prevent adverse outcomes. Patients with no known history of diabetes do not routinely have blood glucose testing ordered postoperatively and may develop hyperglycemia that is not identified and therefore not treated.
Until very recently, it was not known whether the adverse outcomes in surgical patients with dysglycemia were due to hyperglycemia in the postoperative period or poor glucose control in the months prior to surgery. In October 2015, Goodenough et al. published a prospective study of 438 patients having abdominal surgery to determine the optimal HbA1c level associated with the least surgical risk.2 Almost half the patients with HbA1c ≥ 6.5% had not previously been diagnosed with diabetes. They found that both HbA1c ≥ 6.5% and perioperative hyperglycemia (defined as peak glucose ≥ 8.9 mMol·L−1) were independently associated with an increased rate of major complications after abdominal surgery, although HbA1c ≥ 6.5% was a stronger predictor. The authors suggest that short-term glycemic control may correlate better with SSI, whereas long-term control measured by HbA1c may more likely be associated with other adverse events such as cardiovascular complications. They recommend broader HbA1c testing preoperatively due to the high rate of undiagnosed diabetes and the strong association between HbA1c and major complications. Nevertheless, caution is required as it is not clear which patients should undergo HbA1c screening. In the current study, 64% (23/36) of patients with postoperative hyperglycemia had normal HbA1c levels.
The CANRISK is an inexpensive evidence-based tool that effectively and efficiently identifies people at high risk for diabetes and allows for targeted laboratory testing. Ninety percent of study patients completed the questionnaire, which proved to be the strongest predictor of elevated HbA1c, with 31% of patients with a high score having HbA1c ≥ 6.0%. Among patients with a low CANRISK score, none had HbA1c ≥ 6.5%. The CANRISK could easily be incorporated into the preoperative assessment for most elective surgical patients and allow for targeted HbA1c testing.
There is increasing evidence in the literature that elevated preoperative HbA1c is related to adverse outcomes following a variety of surgical procedures. Preoperative identification of poorly controlled or newly diagnosed diabetes can allow for early intervention. Recent studies have shown that treating diabetic patients with HbA1c > 8.0% before surgery resulted in better blood glucose the day of surgery, reduced length of hospital stay, and lower complication rates in the first year after surgery.27,28 Nevertheless, the current evidence is insufficient to recommend an upper limit of HbA1c prior to elective surgery, and the risks associated with poor glycemic control should be balanced against the necessity for surgery.
The conclusions from Goodenough et al.2 show the importance of identifying both elevated HbA1c as well as postoperative hyperglycemia. Although there is a correlation between the two, the types of complications may differ. Hyperglycemia impairs the immune response leading to an increase in SSI.14 It is likely that this risk would occur even in hyperglycemic patients with normal HbA1c levels. Our study showed that patients with preoperative CBG > 6.9 mMol·L−1 were significantly more likely to experience postoperative hyperglycemia compared with those with preoperative CBG < 6.1 mMol·L−1. This use of preoperative CBG screening (even when drinking clear fluids) may help establish which patients to follow closely with postoperative CBG testing. Further study is needed to determine the appropriate preoperative CBG levels that should trigger more testing.
There are several limitations to this study. While we were able to confirm that the CANRISK score can reliably identify patients without an elevated HbA1c preoperatively, the study was not designed to conduct multivariable analyses to identify the best set of risk factors to predict who might have an elevated HbA1c preoperatively. Nevertheless, these results provide a relatively easy and inexpensive means of identifying a high-risk cohort who would benefit from HbA1c testing preoperatively. The findings can also be used to develop future studies to identify the best combination of risk factors to identify a high-risk group of individuals who should be considered for HbA1c testing preoperatively. Another limitation of this study is missing CBG and CANRISK data. As outlined in the results, the majority of the missing data is due to early discharge (therefore not truly missing) or missed blood testing. Missing data appear to have affected all HbA1c groups, and the effect on the results is difficult to predict. An additional limitation is the fact that we could not verify the pre-meal status of the CBG measures; therefore, hyperglycemia was defined as CBG ≥ 10.0 mMol·L−1. If many patients were fasting before the measures were drawn, then the results of this study are conservative and the true prevalence of postoperative hyperglycemia may be even higher. Although we did document postoperative complications, due to the small number of patients in the study and the diverse surgical procedures and patient factors, we were not able to make valid comparisons between groups regarding complication rates. Lastly, there are uncommon conditions where HbA1c may not accurately reflect glycemic status. Such conditions include diseases with altered hemoglobin structure or where the rate of red blood cell turnover is significantly shortened or prolonged (e.g., hemoglobinopathies, chronic liver disease, etc.).17
In this study, elevated HbA1c was relatively common among elective surgical patients with no history of diabetes and was associated with higher mean CBG levels postoperatively. Both elevated HbA1c and preoperative CBG were predictors of clinically significant postoperative hyperglycemia, but more research is required to determine the most reliable means to identify which patients would benefit from postoperative CBG monitoring and treatment to reduce the risk of SSI. A high CANRISK score was a strong predictor for elevated HbA1c, and HbA1c has been associated with major cardiovascular complications after surgery. Several recent studies have shown that treatment of elevated HbA1c preoperatively and hyperglycemia postoperatively can reduce the risk of adverse outcomes.27,28 Therefore, it is important to identify patients at risk of these complications by more widespread HbA1c and CBG testing. Nevertheless, the findings of this study must be viewed with caution due to the small sample size and heterogeneous nature of the surgical procedures included. Future studies are needed to evaluate the role of CANRISK screening to identify surgical patients who may benefit from further testing.
References
Government of Canada. Diseases and Conditions: Type 2 diabetes. Available from URL: http://healthycanadians.gc.ca/diseases-conditions-maladies-affections/disease-maladie/diabete-eng.php (accessed June 2016).
Goodenough CJ, Liang MK, Nguyen MT, et al. Preoperative glycosylated hemoglobin and postoperative glucose together predict major complications after abdominal surgery. J Am Coll Surg 2015; 221(854-61): e1.
Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg 2013; 257: 8-14.
Marchant MH Jr, Viens NA, Cook C, Vail TP, Bolognesi MP. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am 2009; 91: 1621-9.
Moghissi ES, Korytkowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care 2009; 32: 1119-31.
Noordzij PG, Boersma E, Screiner F, et al. Increased preoperative glucose levels are associated with perioperative mortality in patients undergoing noncardiac, nonvascular surgery. Eur J Endocrinol 2007; 156: 137-42.
Sampson MJ, Dozio N, Ferguson B, Dhatariya K. Total and excess bed occupancy by age, specialty and insulin use for nearly one million diabetes patients discharged from all English Acute Hospitals. Diabetes Res Clin Pract 2007; 77: 92-8.
Frisch A, Chandra P, Smiley D, et al. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care 2010; 33: 1783-8.
Jamsen E, Nevalainen PI, Eskelinen A, Kalliovalkama J, Moilanen T. Risk factors for perioperative hyperglycemia in primary hip and knee replacements. A prospective observational study of 191 patients with osteoarthritis. Acta Orthop 2015; 86: 175-82.
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler M, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 2002; 87: 978-82.
Aldam P, Levy N, Hall GM. Perioperative management of diabetic patients: new controversies. Br J Anaesth 2014; 113: 906-9.
Gottschalk A, Rink B, Smektala R, Piontek A, Ellger B, Gottschalk A. Spinal anesthesia protects against perioperative hyperglycemia in patients undergoing hip arthroplasty. J Clin Anesth 2014; 26: 455-60.
Tennyson C, Lee R, Attia R. Is there a role for HbA1c in predicting mortality and morbidity outcomes after coronary artery bypass graft surgery? Interact Cardiovasc Thorac Surg 2013; 17: 1000-8.
Gustafsson UO, Thorell A, Soop M, Ljungqvist O, Nygren J. Haemoglobin A1c as a predictor of postoperative hyperglycaemia and complications after major colorectal surgery. Br J Surg 2009; 96: 1358-64.
Ito N, Iwaya T, Ikeda K, et al. Hyperglycemia 3 days after esophageal cancer surgery is associated with an increased risk of postoperative infection. J Gastrointest Surg 2014; 18: 1547-56.
Choi PT, Griesdale DE. Finding the sweet spot in preoperative assessment. Can J Anesth 2014; 61: 393-7.
Committee Canadian Diabetes Association Clinical Practice Guidelines Expert. Cheng AY. Canadian Diabetes Association 2013 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes 2013; 37(Suppl 1): S1-3.
Merchant R, Chartrand D, Dain S, et al. Guidelines to the practice of anesthesia – revised edition 2016. Can J Anesth 2016; 63: 86-112.
Koumpan Y, VanDenKerkhof E, van Vlymen J. An observational cohort study to assess glycosylated hemoglobin screening for elective surgical patients. Can J Anesth 2014; 61: 407-16.
Faritous Z, Ardeshiri M, Yazdanian F, Jalali A, Totonchi Z, Azarfarin R. Hyperglycemia or high hemoglobin A1C: which one is more associated with morbidity and mortality after coronary artery bypass graft surgery? Ann Thorac Cardiovasc Surg 2014; 20: 223-8.
Kaczorowski J, Robinson C, Nerenberg K. Development of the CANRISK questionnaire to screen for prediabetes and undiagnosed type 2 diabetes. Can J Diabetes 2009; 33: 381-5.
Robinson CA, Agarwal G, Nerenberg K. Validating the CANRISK prognostic model for assessing diabetes risk in Canada’s multi-ethnic population. Chronic Dis Inj Can 2011; 32: 19-31.
Engoren M, Schwann TA, Habib RH. Hyperglycemia, hypoglycemia, and glycemic complexity are associated with worse outcomes after surgery. J Crit Care 2014; 29: 611-7.
Agos F, Shoda C, Bransford D. Part II: Managing perioperative hyperglycemia in total hip and knee replacement surgeries. Nurs Clin North Am 2014; 49: 299-308.
Malcolm JC, Kocourek J, Keely E, et al. Implementation of a screening program to detect previously undiagnosed dysglycemia in hospitalized patients. Can J Diabetes 2014; 38: 79-84.
Kotagal M, Symons RG, Hirsch IB, et al. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg 2015; 261: 97-103.
Kallio PJ, Nolan J, Olsen AC, Breakwell S, Topp R, Pagel PS. Anesthesia preoperative clinic referral for elevated Hba1c reduces complication rate in diabetic patients undergoing total joint arthroplasty. Anesth Pain Med 2015; 5: e24376.
Underwood P, Seiden J, Carbone K, et al. Early identification of individuals with poorly controlled diabetes undergoing elective surgery: improving A1C testing in the preoperative period. Endocr Pract 2015; 21: 231-6.
Acknowledgements
We gratefully acknowledge Dr. Robyn Houlden for her expertise and assistance with the study design and for recommendations regarding the management of hyperglycemia. Thanks to Aditi Kane for her assistance in data collection. In addition, we sincerely thank the nurses in the Same Day Admission Centre, Postanesthesia Care Unit, and surgical wards for their assistance in capillary blood glucose measurements.
Funding
This study was funded using departmental research support through the Alison B. Froese Research Fund in Anesthesiology and Perioperative Medicine and the Queen’s University Thomas M. and Louise A. Brown Research Studentship Award.
Conflicts of interest
None declared.
Author contributions
Michael Yang, Melanie Jaeger, Elizabeth VanDenKerkhof, and Janet van Vlymen participated in the design of the study. Michael Yang and Michael Baxter collected the data. Elizabeth VanDenKerkhof analyzed the data. Michael Yang, Michael Baxter, Melanie Jaeger, Elizabeth VanDenKerkhof, and Janet van Vlymen participated in the interpretation of the data and wrote and critically revised the manuscript.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is accompanied by an editorial. Please see Can J Anesth 2016; 63: this issue.
Appendices
Appendix 1

Canadian Diabetes Risk Questionnaire
Appendix 2

General recommendations for the management of hyperglycemia
Rights and permissions
About this article
Cite this article
Yang, M.H., Jaeger, M., Baxter, M. et al. Postoperative dysglycemia in elective non-diabetic surgical patients: a prospective observational study. Can J Anesth/J Can Anesth 63, 1319–1334 (2016). https://doi.org/10.1007/s12630-016-0742-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-016-0742-7