Abstract
Background and objectives
Lumbar plexus (LP) block is a common and useful regional anesthesia technique. Surface landmarks used to identify the LP in patients with healthy spines have been previously described, with the distance from the spinous process (SP) to the skin overlying the LP being approximately two-thirds the distance from the SP to the posterior superior iliac spine (PSIS) (SP-LP:SP-PSIS ratio). In scoliotic patients, rotation of the central neuraxis may make these surface landmarks unreliable, possibly leading to an increased block failure rate and an increased incidence of complications. The objective of the present study was to describe these surface landmarks of the LP in patients with scoliosis.
Methods
We selected 47 patients with known thoracolumbar scoliotic disease from our institution’s radiology archives. We measured bony landmark geometry, Cobb angle, and the LP location and depth. Additionally, we calculated the SP-LP:SP-PSIS ratio for both the concave and convex sides.
Results
In scoliotic patients (31 females and 16 males), the median (range) Cobb angle was 23 (8-54) degrees. The LP depth was 7.5 (5.7-10.7) cm on the concave side of the scoliotic spine and 7.6 (5.4-10.8) cm on the convex side, while the distance from the SP-LP was 3.4 (1.9-4.7) cm on the concave side and 3.7 (2.4-5.1) cm on the convex side. The SP-LP:SP-PSIS ratio was 0.61 (0.20-0.97) and 0.65 (0.45-0.98) on the concave and convex sides, respectively. None of these distances were significantly different between sides.
Conclusions
In patients with scoliotic disease of the spine, there is wide variability in the bony surface landmarks. The location of the LP is generally more medial than expected when compared with both modified and traditional landmarks. A review of the imaging studies and the pre-procedural ultrasound assessment of the anatomy should be considered prior to needle puncture.
Résumé
Contexte et objectifs
Le bloc du plexus lombaire (PL) est une technique d’anesthésie régionale utile et souvent utilisée. Des repères cutanés servant à identifier le PL chez des patients ayant une colonne vertébrale normale ont été décrits antérieurement: la distance entre l’apophyse épineuse (AÉ) et la peau recouvrant le PL étant approximativement les deux tiers de la distance séparant l’AÉ de l’épine iliaque postéro-supérieure (EIPS) (rapport AÉ–PL/AÉ–ÉIPS). Chez les patients scoliotiques, la rotation du névraxe peut rendre ces repères cutanés non fiables, menant possiblement à un plus grand taux d’échec du bloc et à une plus grande fréquence des complications. L’objectif de la présente étude était de décrire ces repères cutanés du PL chez des patients atteints de scoliose.
Méthodes
Nous avons sélectionné 47 patients ayant une scoliose thoracolombaire connue dans les archives radiologiques de notre établissement. Nous avons mesuré la géométrie des repères osseux, l’angle de Cobb, l’emplacement du PL ainsi que sa profondeur. De plus, nous avons calculé le rapport AÉ–PL/AÉ–ÉIPS du côté convexe et du côté concave.
Résultats
Chez les patients scoliotiques (31 femmes et 16 hommes), l’angle de Cobb médian (extrêmes) était de 23° (8°-54°). La profondeur du PL était de 7,5 cm (5,7-10,7) du côté concave de la colonne vertébrale scoliotique et de 7,6 cm (5,4-10,8) du côté convexe, tandis que la distance ÉP–PL était de 3,4 cm (1,9-4,7) du côté concave et de 3,7 cm (2,4-5,1) du côté convexe. Les rapports AÉ–PL/AÉ–ÉIPS étaient de 0,61 (0,20-0,97) et 0,65 (0,45-0,98), respectivement, du côté concave et du côté convexe. Aucune de ces distances n’a présenté de différence significative selon le côté.
Conclusions
Il existe une grande variabilité des repères cutanés osseux chez les patients ayant une scoliose vertébrale. La localisation du PL est habituellement plus centrale qu’attendu par rapport aux repères traditionnels et aux repères modifiés. Un contrôle des études d’imagerie et de l’évaluation échographique de l’anatomie avant intervention doit être envisagé avant de piquer le patient.
Similar content being viewed by others
The lumbar plexus (LP) block, also known as the psoas compartment block, can be utilized to provide primary anesthesia as well as postoperative analgesia for a number of surgical procedures. Because of the deep location of the plexus and its potential for serious complications, the LP block is considered an “advanced technique” even when used under ideal conditions in patients with normal spinal anatomy.1 Epidural spread, high neuraxial anesthesia, hypotension, local anesthetic toxicity, iliopsoas hematoma, and renal hematoma are the most common complications reported in the literature.1
Several approaches based on surface anatomy have been used to place an LP block. The modified traditional approach relies on a needle entry point that is 4 cm lateral to the spinous process (SP) at the level of the L4 vertebral body.1 In contrast, with the approach described by Capdevila et al., the needle entry point is located two-thirds the distance between the SP and the posterior superior iliac spine (PSIS) along the intercristal line, based on data from computerized tomography (CT).2 Because patients with scoliosis have rotation of their central neuraxis, surface landmarks may be altered, resulting in an incorrect needle entry site. This has the potential to lead to an increased block failure rate and an increased incidence of complications, including local anesthetic toxicity as well as needle entry into the kidney or the epidural space.3 - 5 The present study was designed to describe the surface landmarks used in the performance of the LP block in patients with spinal scoliosis. Additionally, we aimed to examine the correlation between the Cobb angle, an indicator of the severity of scoliosis, and the surface landmarks of the LP.
Methods
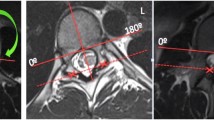
Following Institutional Review Board approval (July 2006), the abdominal CT scans from a convenience sample of 47 patients with known thoracolumbar scoliotic disease of the spine were selected from Mayo Clinic radiology archives. There was no preselected indication for the CT scan, and therefore, any reason for a CT was included in our dataset. All CT scans were performed at the Mayo Clinic, Florida. The CT scan archives were searched using the key word “scoliosis”, and there were no exclusion criteria other than a Cobb angle < 10° and known hardware of the lumbar spine. A senior radiology resident, under the supervision of a consultant radiologist, read the CT films using a MagicView 300 imaging system (Siemens AG; Munich, Germany) and recorded the relevant geometry. The CT scan resolution was 5 mm per slice. Computerized tomography scout films of the lumbar spine or thoracolumbar spine were used to determine the Cobb angle (Fig. 1). Next, transverse (i.e., axial) CT sections of the lumbar region were examined, centring on the level of the intercristal line (Fig. 1). The researchers then selected the films for measurement that best illustrated LP anatomy. The “best” film was defined as the slice in which the LP appeared to be centred. This was generally within ± 1 cm (two CT scan slices) of the intercristal line.
We measured the bony landmarks for the LP block using both the modified traditional technique and the technique described by Capdevila et al., including the location of the PSIS relative to the SP, the location of the LP in the transverse plane, the location of transverse processes, the skin depth to the LP, and the Cobb angle. In addition, we measured the location of the transverse process relative to the SP at the level of the intercristal line. The direction of scoliotic curvature was noted. Measurements were made bilaterally on both sides of the SP and recorded to the nearest millimeter. Figure 2 shows a transverse view of a CT scan illustrating relevant anatomy measurements. We used DicomWorks 1.3.5 imaging software (Puech et al., 2007) to project the path of a 10-cm Tuohy needle inserted using the traditional landmark of 4 cm lateral to the SP and manipulated in the likely direction that an anesthesiologist would use when performing a block. We projected the direction perpendicular in all planes, as well as possible “searching” directions of approximately 10°. Researchers noted structures other than the LP plexus that may be potentially breached by the needle.
Transverse CT showing study measurements relative to the spinous process (SP); D 1 = distance from skin to LP on convex side of curvature; D 2 = distance from skin to LP on concave side of curvature; T 1 = distance from SP to midpoint of transverse process on convex side of curvature; T 2 = distance from SP to midpoint of transverse process on concave side of curvature; L 1 = distance from SP to point on skin overlying LP on convex side of curvature; L 2 = distance from SP to point on skin overlying LP on concave side of curvature; P 1 = distance from spinous process to PSIS on convex side of curvature; P 2 = distance from spinous process to PSIS on concave side of curvature. CT = computed tomography; LP = lumbar plexus; PSIS = posterior superior iliac spine
Statistical analysis was performed using SAS® version 9.3 (SAS Institute Inc., Cary, NC, USA). Sample median, minimum, and maximum were used to summarize continuous data. The Wilcoxon signed-rank test was used to explore paired comparisons in the landmarks between the convex and concave sides of the spine. Comparisons between males and females were performed utilizing the Wilcoxon rank-sum test. Spearman’s rank correlation test was used to evaluate the correlation between the Cobb angle and the landmarks to the LP. All recorded P values are two sided.
Results
In our study, patients had a median (range) age of 80 (69-90) years; 31 (66%) of 47 patients were female, and the median (range) Cobb angle was 23 (8-54) degrees. The Table summarizes the overall study results according to sex. The median (range) skin depth to the LP was 7.5 (5.7-10.7) cm on the concave side and 7.6 (5.4-10.8) cm on the convex side. The median (range) distance from the SP to the midpoint of the transverse process at the level of the intercristal line was 4.5 (2.7-5.4) cm on the concave side of curvature and 4.3 (2.8-5.5) cm on the convex side of curvature. The median (range) distance from the SP to the PSIS on the concave side of scoliotic disease was 5.5 (3.5-9.6) cm and 5.7 (3.2-7.7) cm on the convex side of curvature.
The median (range) distance from the SP to the point on the skin overlying the LP was 3.4 (1.9-4.7) cm on the concave side of curvature and 3.7 (2.4-5.1) cm on the convex side of curvature. The LP was a median (range) of 0.6 (−0.7-2.1) cm medial to the modified traditional landmark on the concave side and 0.3 cm (−1.1-1.6) cm medial to the modified traditional landmark on the convex side.
The SP-LP:SP-PSIS ratio landmark (described by Capdevila et al.; referred to as the “Ratio” in the Table) had a median (range) value of 0.61 (0.20-0.97) on the concave side and 0.65 (0.45-0.98) on the convex side. The median (range) difference between the ratio proposed by Capdevila et al. (0.67) and the ratio observed in our study was 0.06 (−0.30-0.47) on the concave side and 0.02 (−0.31-0.21) on the convex side.
The paired comparisons between the concave and convex sides of the spine did not show a consistent relationship for the skin depth to the LP (P = 0.37), the distance from the SP to the mid-point of the transverse process (P = 0.22), the distance from the SP to the PSIS (P = 0.76), the distance from the SP to the point on the skin overlying the LP (P = 0.16), or the ratio (P = 0.36).
On the convex side of the curvature, the distance from the SP to the point on the skin overlying the LP had a slightly better correlation with the Cobb angle (Spearman’s r = 0.23; P = 0.12), but this was not statistically significant. On the concave side of the curvature, the distance from the SP to the midpoint of the transverse process had the strongest correlation with the Cobb angle (Spearman’s r = 0.17; P = 0.24) but was again not statistically significant. None of the other landmarks to the LP were significantly correlated with the Cobb angle on either the concave side (all Spearman’s |r| ≤ 0.08; all P ≥ 0.61) or the convex side (all Spearman’s |r| ≤ 0.16; all P ≥ 0.30).
Figures 3 and 4 show the projected needle paths of an attempted LP block in a representative patient with scoliosis, including searching directions following failed plexus localization on first needle pass. As can be seen in the Figs., it is possible to encounter structures other than the LP, including the kidney and centroneuraxis structures.
Transverse CT of a patient with severe scoliosis, Cobb angle 35°. Renal, epidural, or dural puncture is possible when performing an LP block on a scoliotic patient, as shown by the projection of the 10-cm needle with searching directions 10° in the transverse plane. CT = computed tomography; LP = lumbar plexus
Transverse CT of a patient with moderate scoliosis, Cobb angle 22°. Renal, epidural, or dural puncture is possible when performing an LP block on a scoliotic patient as shown by the projection of the 10-cm needle with searching directions 10° in the transverse plane. CT = computed tomography; LP = lumbar plexus
Discussion
Based on our data, it appears that the location of the LP is highly variable in adults with scoliotic changes of the spine. Generally speaking, the LP is located more medially than would be expected compared with either the modified traditional landmarks or the landmarks described by Capdevila et al., regardless of the side of curvature.
The prevalence of scoliosis of the lumbar spine in adults has been estimated to range from 1.4-20% in the general population and up to 68% in patients > 60 yr of age.6 , 7 A Cobb angle > 10° in the coronal plane is typically required to make the diagnosis of scoliosis, though no clear diagnostic criteria exist.8 , 9 Scoliosis in adults can be either progressive from childhood or de novo. De novo adult scoliosis is most commonly due to asymmetric disc degeneration and facet joint degeneration.10 The latter forms a vicious cycle: the progression of lumbar curvature results in increasing joint stress, and increasing joint stress results in more curvature, thus furthering scoliotic disease. The most common site of the apex of curvature is the L2/3 and L3/4 joint, but most adults will have additional thoracolumbar curvature in addition to lumbar curvature.9 Schwab et al. studied spinal deformity in 75 healthy volunteers aged 60-90 yr and found a mean Cobb angle of 17°. The majority (44%) of patients had a Cobb angle of 10-20°, and 24% of patients had a Cobb angle > 20°. The pattern of curvature distribution was 63% lumbar, 27% thoracic and lumbar, and 10% thoracolumbar.7 While the Cobb angle pertains to left or right spine curvature in scoliosis and alters superficial bony landmarks, the secondary left or right rotation of the vertebral bodies (due to scoliotic spine curvature) also contributes to changes in the superficial bony landmarks.
It is not known whether bony landmark abnormalities from curvature or rotational changes in the spine are more important for affecting the needle insertion site. It is likely that both are important. Although the relationship is not perfectly linear, there is evidence in the literature that the Cobb angle and vertebral rotation correlate.11
In adults with non-scoliotic disease, the landmarks for the LP block are well identified. Posterior approaches, aided by nerve stimulation, are more popular, while the anterior (“3-in-1”) approach is considered to produce more variable success.12 In 1974, Winnie described the first successful posterior technique, i.e., inserting the block needle at the intersection of the intercristal line and running a line parallel to the SP through the PSIS.13 Further modifications by Chayen, Hannah, and Parkinson have been published.1 Hadzic et al. described an updated or “modified traditional” approach, i.e., measuring 4 cm lateral to the SP at the intercristal line.1 In this approach, a nerve stimulator (1.5 mA, 2 Hz, 100 µsec) is attached to a 10-cm short-bevel stimulating needle inserted perpendicular to all planes and advanced until a twitch response of the quadriceps muscle is obtained at a current of 0.5-1.0 mA. Typically, 30 mL of local anesthetic is injected with frequent aspiration.
In 2002, Capdevila et al. published an alternative technique for locating the LP relative to the PSIS.2 He studied axial CT cross sections of patients, described the location of the plexus, and found that the needle entry point should be 0.67 or 0.68 (i.e., approximately 2/3) times the distance from the SP to the PSIS in female and male patients, respectively, based on the consistency of this measurement in their sample (range, 0.60-0.80). In our sample of patients with scoliotic disease, the landmark described by Capdevila et al. was highly variable, with values ranging from 0.20-0.97 on the concave side and 0.45-0.98 on the convex side. Ilfield et al. have subsequently shown that the landmarks used in Capdevila’s study were approximately 0.75 cm too lateral in 50% of patients.14 Because of the large variability we found, using the insertion point determined from our study could potentially have implications on needle trajectory. Depending on which side of the curvature the LP block is planned, the insertion site determined by our study may correct an otherwise too lateral needle trajectory (convex) or may worsen an otherwise too medial needle trajectory (concave).14
The use of real-time ultrasound guidance for the performance of LP block has been described in the literature by several authors and may obviate the need of certain surface landmark approaches in the future as image quality continues to improve.15 , 16 Whether this would reduce complications associated with inadvertent needle placement is not known, but that potential is likely, assuming good image quality. Indeed, one case report describing pre-procedural ultrasound scanning in a patient with known scoliosis allowed successful LP block with a notable difference in needle insertion site compared with “traditional” surface landmarks.17 Nevertheless, given current technology, recent studies have failed to support the widespread use of real-time ultrasound-guided techniques for LP blockade.18 The use of ultrasound to identify the ideal needle insertion site may provide useful information, as there are likely many patients with subclinical or simply undiagnosed scoliotic spine changes whose surface landmarks are altered. The identification of bony structures (transverse process) may help in guiding needle placement in these types of patients. There is a lack of guidance in the literature for performing LP blockade in adults with scoliosis. Given its high prevalence, the anesthesiologist performing an LP block will frequently encounter patients with scoliotic disease. Our study describes landmarks to the LP in this population and questions the reliability of both the modified traditional landmark and the Capdevila landmark in patients with scoliosis.
An anatomical explanation of our findings is confirmed by the observation that the LP is embedded within the psoas major muscle.19 The psoas major muscle originates on the transverse processes, intervertebral discs, and bodies of the T12-L5 vertebrae and connects onto the lesser trochanter of the femur.20 Lateral displacement to the spine will result in a component of rotation of the psoas group, since the psoas muscle is anchored to the femur. The transverse processes will be rotated inward toward midline in the transverse plane. The psoas will be stretched further on the convex side in the coronal plane due to anchoring on the relatively fixed trochanter and ilium. This combination would seemingly result in the LP being displaced medially on both the concave and convex sides of the curvature, with a more superficial LP position on the concave side and a deeper position on the convex side. One would expect that, as the Cobb angle increases, medial displacement of the LP would also increase. Furthermore, one would expect that, as the Cobb angle increases, the LP would move increasingly superficial on the concave side and increasingly deep on the convex side. While our data do seem to indicate that, regardless of the side of curvature, the LP is generally located more medially than described by Capdevila et al., there is not a linear correlation with the Cobb angle. It appears that, as the Cobb angle increases, rotational changes of the spine do not change in a linear fashion. The apparent large variability of LP location in patients with scoliosis is probably more important. This suggests that a more rigorous assessment of anatomy should be undertaken through a review of imaging studies and that pre-procedural ultrasound imaging should be considered prior to needle puncture.
Complications of the LP block include epidural spread, intrathecal spread, psoas hematoma, and renal hematoma. Additionally, complications with any regional technique may include infection, local anesthetic toxicity and nerve injury.21 In scoliotic patients, modified traditional landmarks and the landmarks described by Capdevila et al. may result in a needle trajectory which results in possible intrusion into structures such as the epidural space or the kidney. Figures 3, 4, and 5 illustrate this point. We speculate that complication rates may be increased in the scoliotic patient population receiving an LP block using landmark-based techniques that identify and are based on the SP. In these patients, ultrasound guidance may be particularly advantageous. Identification of important structures that lie within the needle trajectory may decrease complications.
Our study has several limitations. Firstly, our study is retrospective, observational, and limited when compared with a prospective analysis that may provide direct success and complication rates in scoliotic patients undergoing LP block. Secondly, CT imaging may not be an ideal imaging modality, as magnetic resonance imaging may more clearly identify nerve anatomy. Thirdly, we did not collect body mass index (BMI) data in our patient population; however, bony landmarks should be independent of BMI, and therefore, we would not expect a higher BMI to affect the data per se. That being said, there is evidence that a higher BMI is associated with an increased Cobb angle in adolescents.22 Not measuring the effect of BMI on LP depth may have contributed partially to the lack of significant findings in terms of differences in depth between the concave and the convex side and differences between men and women. Another possible limitation is that all CT scans were obtained with the patient in the supine position. This is quite different from the lateral decubitus position that is generally used to perform the LP block. We are unable to quantify how these differences in position (i.e., used to collect data vs used to perform the real block) affect the data. We consider our methods reasonable because supine positioning is the standard for CT scan acquisition. Another possible limitation is the possibility of human error in terms of determining where to take a given measurement on the CT films (i.e., midpoint of the transverse process). While we acknowledge this as a possibility, we are unable to resolve this issue through study design. Finally, while 47 patients seems to be a reasonable number of individuals to power this study based on other work in the area, it is possible that a larger study population may have found additional significant correlations between degree of scoliosis and LP location.
The results of our study indicate that patients with a history of scoliosis who present for LP block require a more critical assessment of anatomy prior to needle puncture. A full review of any available CT/magnetic resonance imaging and possible bedside ultrasound assessment of lumbar anatomy should be the minimum requirement before proceeding with block placement. In summary, the location of the LP is highly variable in the adult with scoliotic changes of the spine. Furthermore, the LP is located more medially than would be expected compared with either the modified traditional landmarks or the landmarks described by Capdevila et al., regardless of the side of curvature. Ultrasound guidance may be advantageous in patients with scoliosis of the lumbar spine, though further study is needed.
References
Robards C, Hadzic A. Lumbar plexus block. In: Hadzic A (Ed.). The New York School of Regional Anesthesia Textbook of Regional Anesthesia and Acute Pain Management, 1st ed. New York: Mc Graw Hill Medical; 2007: 481-8.
Capdevila X, Macaire P, Dadure C, et al. Continuous psoas compartment block for postoperative analgesia after total hip arthroplasty: new landmarks, technical guidelines, and clinical evaluation. Anesth Analg 2002; 94: 1606-13.
Aida S, Takahashi H, Shimoji K. Renal subcapsular hematoma after lumbar plexus block. Anesthesiology 1996; 84: 452-5.
Vadi MG, Patel N, Stiegler MP. Local anesthetic systemic toxicity after combined psoas compartment-sciatic nerve block: analysis of decision factors and diagnostic delay. Anesthesiology 2014; 120: 987-96.
Auroy Y, Benhamou D, Bargues L, et al. Major complications of regional anesthesia in France: The SOS Regional Anesthesia Hotline Service. Anesthesiology 2002; 97: 1274-80.
Schwab F, Dubey A, Pagala M, Gamez L, Farcy JP. Adult scoliosis: a health assessment analysis by SF-36. Spine 2003; 28: 602-6.
Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005; 30: 1082-5.
Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine 2002; 27: 387-92.
Aebi M. The adult scoliosis. Eur Spine J 2005; 14: 925-48.
Marty-Poumarat C, Scattin L, Marpeau M, Garreau de Loubresse C, Aegerter P. Natural history of progressive adult scoliosis. Spine (Phila Pa 1976) 2007; 32: 1227-34; discussion 1235.
Easwar TR, Hong JY, Yang JH, Suh SW, Modi HN. Does lateral vertebral translation correspond to Cobb angle and relate in the same way to axial vertebral rotation and rib hump index? A radiographic analysis on idiopathic scoliosis. Eur Spine J 2011; 20: 1095-105.
Awad IT, Duggan EM. Posterior lumbar plexus block: anatomy, approaches, and techniques. Reg Anesth Pain Med 2005; 30: 143-9.
Winnie AP, Ramamurthy S, Durrani Z, Radonjic R. Plexus blocks for lower extremity surgery. Anesthesiol Rev 1974; 1: 11-6.
Ilfeld BM, Loland VJ, Mariano ER. Prepuncture ultrasound imaging to predict transverse process and lumbar plexus depth for psoas compartment block and perineural catheter insertion: a prospective, observational study. Anesth Analg 2010; 110: 1725-8.
Kirchmair L, Entner T, Kapral S, Mitterschiffthaler G. Ultrasound guidance for the psoas compartment block: an imaging study. Anesth Analg 2002; 94: 706-10.
Karmakar MK, Ho AM, Li X, Kwok WH, Tsang K, Ngan Kee WD. Ultrasound-guided lumbar plexus block through the acoustic window of the lumbar ultrasound trident. Br J Anaesth 2008; 100: 533-7.
Factor D, Perlas A. Ultrasound-assisted lumbar plexus block in a patient with scoliosis. Reg Anesth Pain Med 2010; 35: 568-9.
Chin KJ, Perlas A. Ultrasonography of the lumbar spine for neuraxial and lumbar plexus blocks. Curr Opin Anaesthesiol 2011; 24: 567-72.
Di Benedetto P, Pinto G, Arcioni R, et al. Anatomy and imaging of lumbar plexus. Minerva Anestesiol 2005; 71: 549-54.
Chung KW. Gross Anatomy. 4th ed. Philadelphia: Lippincott Williams & Willkins; 2000 .
Greengrass RA. Posterior lumbar plexus block. Tech Reg Anesth Pain Manag 2003; 7: 3-7.
Matusik E, Durmala J, Matusik P, Wadolowski K. Severity of spine deformity in children and adolescents with idiopathic scoliosis is associated with nutritional status and body composition. Bone Abstracts 2013; DOI: 10.1530/boneabs.2.P151.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Christopher B. Robards, Kevin Riutort, Colleen S. Thomas, and Brandon R. Runyan helped analyze the data. Christopher B. Robards, Kevin Riutort, Colleen S. Thomas, Steven B. Porter, R. Doris Wang, Steven R. Clendenen, and Roy A. Greengrass assisted with writing the manuscript. Kevin Riutort and Roy A. Greengrass helped design the study. Kevin Riutort, R. Doris Wang, Steven R. Clendenen, and Brandon R. Runyan helped conduct the study. Kevin Riutort has seen the original study data and is the author responsible for archiving the study files. Colleen S. Thomas conducted the final analysis of the data. Kevin Riutort, Brandon R. Runyan, and Roy A. Greengrass reviewed the analysis of the data.
Rights and permissions
About this article
Cite this article
Robards, C.B., Riutort, K., Thomas, C.S. et al. Lumbar plexus block surface landmarks as assessed by computed axial tomography in adult patients with scoliosis: a case series. Can J Anesth/J Can Anesth 62, 385–391 (2015). https://doi.org/10.1007/s12630-014-0303-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0303-x