Abstract
Purpose
Combined acetaminophen and ibuprofen may be more effective than either constituent alone for pain in adults. The combination was compared with the individual constituents for analgesia following tonsillectomy in children.
Methods
One hundred and fifty-two children (6-14 yr) undergoing tonsillectomy were randomized to receive either combination acetaminophen (48 mg·kg−1·day−1) and ibuprofen (24 mg·kg−1·day−1) or the same doses of acetaminophen alone or ibuprofen alone, every six hours for 48 hr. The primary outcome measure was a time-corrected area under the curve (AUCt) calculated from assessments on a 100-mm visual analogue scale (with Wong Baker FACES® as anchors). At each assessment the children rated pain while at rest and on swallowing at multiple time points over the study duration. Secondary outcome measures were a global pain rating, requirement for rescue analgesia, sleep disturbance, and frequency of adverse events.
Results
The mean [standard error of the mean (SEM)] AUCt values at rest were; combination 29.6 (1.9), acetaminophen 30.4 (2.0), ibuprofen 34 (1.9). The mean (SEM) AUCt values on swallowing were; combination 39.1 (2.0), acetaminophen 39.9 (2.0), ibuprofen 43.7 (1.9). The mean (95% confidence interval) differences in AUCt values between groups on swallowing were: combination vs acetaminophen −0.9 (−6.2 to 4.5); combination vs ibuprofen −4.6 (−9.9 to 0.67) and at rest were: combination vs acetaminophen −0.81 (−6.11 to 4.48); combination vs ibuprofen −4.37 (−9.62 to 0.88). Differences between groups were not clinically important for the pain scores, similarly for the secondary outcomes.
Conclusion
The combination of ibuprofen and acetaminophen was not superior to its individual components in the regimen studied in this pediatric population undergoing tonsillectomy. The study was registered with the Australia New Zealand Clinical Trial Registry (ACTRN12607000005459) on January 4, 2007.
Résumé
Objectif
L’association de l’acétaminophène et de l’ibuprofène peut-être plus efficace que chaque molécule seule contre la douleur chez l’adulte. L’association a été comparée aux molécules prises individuellement pour l’analgésie après amygdalectomie chez des enfants.
Méthodes
Cent cinquante deux enfants (âgés de 6 à 14 ans) subissant une amygdalectomie ont été randomisés pour recevoir une association d’acétaminophène (48 mg·kg−1·jour−1) et d’ibuprofène (24 mg·kg−1·jour−1) ou les mêmes doses d’acétaminophène seul ou d’ibuprofène seul, toutes les six heures pendant 48 h. Le critère d’évaluation principal était une surface sous la courbe corrigée pour le temps (ASCt) calculée à partir des évaluations sur une échelle visuelle analogique de 100 mm (l’échelle Wong Baker FACES® servant de référence). À chaque évaluation, les enfants ont coté la douleur au repos et à la déglutition, à de multiples occasions pendant la durée de l’étude. Les critères d’évaluation secondaires étaient une cotation globale de la douleur, la nécessité d’avoir une analgésie complémentaire, les troubles du sommeil et la fréquence des effets indésirables.
Résultats
Les valeurs moyennes (écart-type de la moyenne [ET]) de l’ASCt au repos ont été: association 29,6 (1,9), acétaminophène 30,4 (2,0), ibuprofène 34 (1,9). Les valeurs moyennes (ET) de l’ASCt à la déglutition ont été: association 39,1 (2,0), acétaminophène 39,9 (2,0), ibuprofène 43,7 (1,9). Les différences moyennes (intervalle de confiance à 95 %) entre les valeurs d’ASCt des différents groupes à la déglutition ont été: association contre acétaminophène −0,9 (−6,2 à 4,5); association contre ibuprofène −4,6 (−9,9 à 0,67); au repos, les différences ont été: association contre acétaminophène −0,81 (−6,11 à 4,48); association contre ibuprofène −4,37 (−9,62 à 0,88). Les différences entre les groupes n’étaient pas cliniquement importantes ni pour les scores de douleurs, ni pour les critères d’évaluation secondaires.
Conclusion
L’association d’ibuprofène et d’acétaminophène ne s’est pas montrée supérieure à ses composants individuels pour le protocole étudié chez cette population pédiatrique subissant une amygdalectomie. L’étude a été inscrite au registre des essais cliniques d’Australie-Nouvelle Zélande le 4 janvier 2007 sous le numéro ACTRN12607000005459.
Similar content being viewed by others
Multimodal analgesia has the potential to obtain greater analgesic effect with fewer adverse effects.1 Ibuprofen and acetaminophen have different mechanisms of analgesia and are therefore good candidates for combination therapy. Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that inhibits cyclooxygenase enzymes, predominantly in peripheral tissues.2 The mode of action of acetaminophen is not completely understood, but it is thought to involve a central nervous system effect, possibly mediated through N-methyl-d-aspartate, substance P, cannabinoid, and nitric oxide synthase and serotonergic pathways.3-6
Tonsillectomy is a common surgical procedure in children often performed as day-stay surgery. Postoperative pain following tonsillectomy can be severe and last up to seven days with substantial associated distress for children and parents.7 Acetaminophen and NSAIDs are commonly co-prescribed for postoperative analgesia, and combination therapy would simplify this regime. The results of a recent qualitative systematic review of the evidence for combining acetaminophen and an NSAID for postoperative pain in adults showed that the combination provided superior analgesia to either drug alone.8 Nevertheless, there is insufficient evidence to recommend this combination in children where the risk-benefit ratio may be different. The aim of this study was to determine the efficacy of a novel fixed-dose combination elixir of ibuprofen and acetaminophen in children following tonsillectomy. We examined the primary hypothesis that the combination of ibuprofen and acetaminophen provides better analgesia than either acetaminophen alone or ibuprofen alone.
Trial design and subject selection
This multicentre prospective randomized double-blinded multi-arm parallel active-controlled trial was undertaken from October 2008 to June 2010 following relevant ethics committee approval (Northern X Regional Ethics Committee, New Zealand (NZ) and CLINICOM- Committee for Evaluation of Protocols for Clinical Research, India).
Children were recruited across two study centres in Auckland, NZ and two centres in Ahmedabad, India. Study sites were private hospitals providing day-stay surgery to pediatric and adult surgical patients and a public day-stay surgical unit associated with a secondary pediatric teaching hospital in Auckland.
Eligibility criteria included children aged 6-14 yr presenting to the study centres for routine tonsillectomy (with or without adenoidectomy) under the care of a participating surgeon. Exclusion criteria are presented in Table 1. Research staff identified potentially eligible children at New Zealand sites from pre-screening study site operating lists. The recruitment of children was undertaken primarily by a study nurse with the support of the investigators. At Indian sites, potentially eligible children were identified from pre-screening during routine preoperative outpatient clinics, and the recruitment of children was conducted by participating surgeons.
Written informed consent was provided by a parent or legal guardian, and where appropriate, children provided written assent themselves. No subjects were recruited unless both the participant and his or her parent or legal guardian were willing to provide consent.
Intervention
Children underwent tonsillectomy under general anesthesia. Surgical and anesthetic techniques were at the discretion of the treating clinician. Duration of inpatient stay was determined by clinical status but generally conformed to local standard practice (discharge was on the day of surgery for New Zealand sites and 48 hr following surgery for Indian sites).
Three drug formulations were compared: acetaminophen 120 mg + ibuprofen 60 mg per 5 mL suspension; acetaminophen 120 mg per 5 mL suspension; and ibuprofen 60 mg per 5 mL suspension. The weight-based doses used (0.5 mL·kg−1 per dose) were based on an acetaminophen dose of 48 mg·kg·day−1 in four divided doses and an ibuprofen dose of 24 mg·kg−1·day−1 in four divided doses. The maximum daily dose was 2.4 g acetaminophen and 1.2 g ibuprofen, based on a weight of 50 kg. These doses are consistent with doses used in NZ and the United Kingdom.9,10 The first dose of study drug was administered prior to the induction of anesthesia, then every six hours (or as close as was practical) with food for 48 hr following surgery. To facilitate standardization of the regimen and increase compliance, it was suggested that doses should be given before main meals and before bedtime.
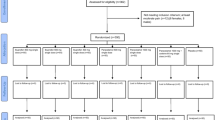
Rescue analgesia was provided if children required additional analgesia due to insufficiently controlled pain (score ≥ 60 mm on study 100-mm visual analogue scale [VAS]). Prior to discharge from the recovery room a rescue dose of intravenous morphine was administered (intravenous fentanyl where contraindications to morphine were present). Following discharge from the recovery room (during “ward stay” and “at home” phases, Fig. 1) patients with inadequately controlled pain were transferred to the combination suspension, ensuring that they were receiving both acetaminophen and ibuprofen.
Frequency of study drug dosing and collection of efficacy and safety data. Children at the Indian sites remained in hospital for 48 hr following surgery (“recovery room” and “ward stay” phases). Children at New Zealand sites were discharged home from the recovery room where they completed study assessments independently for 48 hr (“at home phase”). *Where contraindications to morphine were present, fentanyl was used as rescue analgesia
The study period was 48 hr following surgery. All children were transferred to the combined ibuprofen and acetaminophen suspension for up to ten days following this period.
Study personnel at the Auckland site maintained phone contact with patients on postoperative days 1, 10, and 28 to facilitate completion and return of the study diary and to monitor for adverse events. Study diaries and remaining study drug were returned by prepaid courier. Patients’ primary care providers were contacted to identify any medical treatment sought for adverse effects. Patients at the Indian sites completed their study diaries as inpatients, and these were collected prior to discharge. Patients returned to the study hospital for postoperative review on days 10 and 28, and adverse event data were collected during these visits. Patients were excluded following randomization if they failed to return the study diary or missed more than one dose of the study drug.
Randomization and masking
Children were allocated to treatment groups in a 1:1:1 ratio according to a randomization schedule (computer-generated random numbers) provided by an independent statistician (C.F.). Each participant was assigned a unique randomization number. Investigators and children were blinded to the allocation, and the randomization code was not broken until study data were checked and locked.
The study sponsor provided the study drugs in suspensions identical in appearance (white colour with strawberry flavour, sugar free, and alcohol free) and in identical packaging (100-mL amber bottles with study medicine labelling). All study drugs were manufactured in the Republic of Ireland by Pinewood Laboratories Ltd, a Good Manufacturing Practice (GMP) approved facility. On discharge, children were provided with pre-packaged bottles of the study drug that corresponded to their randomization number. They were also given the combined ibuprofen and acetaminophen suspension for use after the 48-hr study period.
Primary outcome measures
A modified version of a 100-mm horizontal VAS with anchors from the Wong-Baker FACES® Pain Rating and accompanying appropriate text was used to assess pain (Appendix). At each assessment, the children rated pain at rest and on swallowing. Assessments were made at baseline (prior to the initial dose of study drug), immediately postoperatively (once the participant was alert enough to comply), at hourly intervals for the duration of recovery room stay, following discharge from the recovery room, and 30-60 min after each dose of study medication for 48 hr. The area under the curve (AUC) was calculated for each of the two pain scores (“at rest” and “on swallowing”). The AUC was divided by the duration of pain assessment (48 hr) to obtain a measure of the average pain intensity, i.e., time-adjusted AUC (AUCt). The two time-adjusted AUCs were considered co-primary outcomes.
Secondary outcome measures
Requirements for rescue analgesia were assessed in the recovery room and for 48 hr following discharge from the recovery room (during “ward stay” and “at home” periods, Fig. 1). A global pain rating, rated by participants as nil (1), mild (2), moderate (3), or severe (4), was collected on the first postoperative day. Sleep disturbance attributable to pain was rated on a 100-mm VAS (0 = no disturbance; 100 = very disturbed) for the first and second postoperative nights (assisted by the parent or caregiver as required).
The authors reviewed and collated all adverse events identified from parental responses in the patient diaries, from follow-up telephone or clinic contact, and from contact with primary care providers. The only pre-defined category of adverse event was postoperative bleeding requiring intervention. The severity of each event was assessed as either mild (discomfort noticed but no disruption of normal activities), moderate (discomfort sufficient to reduce or affect daily activities), or severe (inability to perform daily activities). Possible relationship to the study drug was also assessed on the basis of the temporal association of the onset of the adverse event relative to drug administration and whether another cause could explain the event.
Sample size estimation
We assumed an overall within-group standard deviation of 14 mm for the AUCt on the basis of data collected in a recent evaluation of combination acetaminophen and ibuprofen for dental pain in adults.11 We employed a Bonferroni correction to allow for the independent assessment of the two pain measures. Forty-eight children per group would give 80% power to show a difference of 9 mm in the AUCt with a comparison-wise type 1 error rate of 0.025 (one-sided) and an overall rate of 0.05. This number was rounded to 50 children per group. We made no adjustment for the two between-drug comparisons. Acceptance of the primary hypothesis required both comparisons (combination vs acetaminophen and combination vs ibuprofen) to reach significance at this level. This situation differs from one where a hypothesis would be accepted if either test were significant. In the latter, the chance of a type I error is increased, and it is normal to adjust the significance level to allow for this. Requiring both between-drug comparisons to be significant did increase the overall chance of a type 2 error (i.e., it reduced the power of the study).12
Statistical analyses
The data were analysed using SPSS® version 15.0 (SPSS Inc., Chicago, IL, USA). The calculation of efficacy endpoints was based on allocation to group by randomization. Safety endpoints were analysed according to the actual treatment taken.
For the primary endpoint, a general linear model (GLM) was used to compare groups. Each model included treatment group, study centre, and a treatment-by-centre interaction term. The interaction term was included to confirm the consistency of any treatment effect.
Sleep disturbance due to pain was compared between groups using the same GLM used for the primary endpoints. The requirement for rescue analgesia, global pain rating scales, and the incidence of adverse events were compared using Chi square or Fisher’s exact tests when expected frequencies were < 5. There was no correction for multiple comparisons for the analyses of the secondary endpoints.
The type I error rate for each of the between-group comparisons was pre-specified at 0.05. For the study hypothesis to be accepted, the AUCt of the combination treatment, either at rest or on activity, was required to be superior to that of the individual ibuprofen and acetaminophen groups.
Results
Patient flow
There were 152 children randomized following initial screening and exclusion of those deemed ineligible. At the Indian sites, 32 patients with health insurance were excluded during the pre-screening process. This was not a pre-defined exclusion criterion and represented a protocol violation. Neither the principal investigator nor the study sponsor received notice of this violation which became evident only during data analysis. Both the Indian and NZ ethics committees were then notified of the protocol violation.
Two children (1%) failed to return patient diaries and were excluded from the primary endpoint analysis (but were included in the safety analysis). Nine children did not complete the global pain rating at the end of treatment, and ten children did not complete the evaluation of sleep disturbance.
Flow of children through the study is presented in Fig. 2. Only three children were recruited at the second New Zealand site, so both New Zealand sites were grouped for the purpose of analysis. Demographics and clinical characteristics were reasonably well balanced between groups at baseline (Table 2).
Compliance
One participant missed one dose of study drug (this participant refused to swallow because of postoperative pain). The parents of one participant administered two additional doses of the study medication during the first 24 hr after surgery. Three children received miscalculated larger doses of the study medications, but none of these exceeded 115% of the scheduled dose.
Analgesic effectiveness outcome analysis
The statistical criterion for superiority of the combination therapy was not met. Time-adjusted AUC scores were not significantly different between the treatment groups at rest. On swallowing, the comparison between the combination treatment and ibuprofen alone for AUCt reached significance. The resulting differences were very small and of no clinical relevance (Table 3).
There was no difference between centres regarding their treatment effects; both centre* treatment interactions were not significant (AUC at rest P = 0.092; AUC on swallowing P = 0.079).
Secondary outcome analysis
There was no clinically important or statistically significant difference between groups in sleep disturbance or in the use of rescue analgesia in the recovery room, but after discharge from the recovery room, fewer patients required rescue analgesia in the combination group than in the other two groups (Table 4). The statistical criterion for superiority of the combination therapy was not met for the global pain ratings, and the difference between the combined group and the acetaminophen group was not clinically compelling (Table 5).
Adverse effects
All randomized participants (n = 152) received at least one dose of the study drug (the preoperative dose administered by study staff) and were therefore included in the adverse effects evaluation. Thirty-three adverse events were reported by 27 participants (18%) and are presented in Table 6. One participant experienced mild postoperative bleeding that was attributed to surgical causes and resolved without admission to hospital. On review by the authors, the majority of adverse events were evaluated as “mild” (80%) and considered to be unrelated to the study drug (64%).
Discussion
The results of the primary outcome analysis showed that the combination of ibuprofen and acetaminophen was not significantly superior to the same daily dose of the component drugs administered individually for alleviating post-tonsillectomy pain in children. Furthermore, the differences in pain scores between groups were not clinically important. As a result, the primary study hypothesis was rejected. Rates of adverse events were consistent with those previously reported for the individual component drugs, but the low expected frequency of adverse events (both drugs have established safety profiles)13 means that this study was insufficiently powered to form definitive conclusions regarding the safety of the combination.
Previous studies comparing the combination of ibuprofen and acetaminophen with individual components for postoperative pain relate predominantly to adult patients.8 Data pertaining to children are limited to three studies using a variety of pain assessment techniques and outcome measures in tonsillectomy and dental pain models.14-16 All of these studies assessed the combination of acetaminophen and ibuprofen using a single-dose design, and one used a rectal route of administration.14 Results of all three studies showed the combination treatment to be superior to acetaminophen alone, although studies comparing the combination treatment with ibuprofen alone showed conflicting results.14,16 These conclusions are inconsistent with our data showing no difference between the three treatments with regard to the primary outcome measure. Our secondary findings are more aligned with this previous work.
Limitations
Our results relate to pediatric patients undergoing tonsillectomy and may not necessarily be generalizable to the adult population or pain following other surgical procedures. The results of this study are strengthened by the administration of the study drug and assessment of postoperative pain over a 48-hr period (as opposed to a single preoperative dose). A recent simulation study suggested a prolonged analgesic effect for the combination of acetaminophen and ibuprofen compared with either drug alone.17 Those authors emphasized the importance of scheduling follow-up evaluations for combination therapy that extend beyond the immediate postoperative period. This may explain the finding of Viitanen et al. that superiority of the combination was evident only following discharge from hospital14 as well as our own result that a requirement for post-discharge rescue medication was eliminated for children receiving the combination.
The same simulation study suggests that improvements in analgesia using the combination may be more apparent when lower doses are investigated (i.e., < 5 mg·kg−1 acetaminophen or 2 mg·kg−1 ibuprofen).17 Larger doses (as used in this study) result in concentrations that correspond to the upper portion of the response curve, meaning that the maximal analgesic effect is approached for both drugs, and the difference between the single and combined therapies becomes less evident. This may explain the negative result in our comparison. As the adverse effects of ibuprofen are dose-dependent,18 the potential to deliver equivalent analgesic efficacy with lower doses of component drugs may therefore make a combination agent more tolerable than traditional doses of ibuprofen.
Quantifying pain in children is notoriously problematic with no clear “gold standard” measurement instrument available.19 A modified version of a horizontal VAS assessment with smiling and crying faces as anchors was used in this study. Visual analogue scales are thought to be less reliable in children aged 12 yr and under, particularly in children younger than eight years.19,20 As our protocol included children aged six years and above, this may have affected the reliability of our measurements in younger children who are more likely to select the extremes on VAS rating scales.19 In addition, where the “crying face” pain anchor is used, children have been shown to underreport pain systematically.19 These factors may collectively explain the low average VAS scores seen in this study. Low overall levels of pain can compound difficulties in assessment of analgesic efficacy. Nevertheless, it is the view of our research group that alleviating pain is a fundamental human right21 and that there are serious ethical concerns about allowing pain to develop in order to show analgesic effect.11,22,23 For this reason, we adopted a preemptive dosing strategy (in contrast to treating established pain) and did not include a placebo comparison.
Simple verbal scores have been shown to be more reliable than VAS ratings for self-assessment of pain in children.24 The global categorical pain rating used as a secondary outcome measure may therefore have been a more appropriate tool than VAS ratings for our participant population, and issues relating to the measurement instruments could explain the conflicting conclusions drawn from these assessments. There were differences between sites regarding the ethnicity of the participants and the clinical practices; however, there was no significant difference between centres in terms of their treatment effects.
In conclusion, the combination of ibuprofen and acetaminophen was not superior to its individual components in the regimen studied in this pediatric population undergoing tonsillectomy.
References
Altman RD. A rationale for combining acetaminophen and NSAIDs for mild-to-moderate pain. Clin Exp Rheumatol 2004; 22: 110-7.
Vane JR, Botting RM. Mechanism of action of anti-inflammatory drugs. Scand J Rheumatol Suppl 1996; 102: 9-21.
Toussaint K, Yang XC, Zielinski MA, et al. What do we (not) know about how paracetamol (acetaminophen) works? J Clin Pharm Ther 2010; 35: 617-38.
Graham GG, Scott KF. Mechanism of action of paracetamol. Am J Ther 2005; 12: 46-55.
Smith HS. Potential analgesic mechanisms of acetaminophen. Pain Physician 2009; 12: 269-80.
Anderson BJ. Paracetamol (acetaminophen): mechanisms of action. Paediatr Anaesth 2008; 18: 915-21.
Warnock FF, Lander J. Pain progression, intensity and outcomes following tonsillectomy. Pain 1998; 75: 37-45.
Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg 2010; 110: 1170-9.
Paediatric Formulary Committee. BNF for Children 2011-2012: the Essential Resource for Clinical Use of Medicine in Children. London: BMJ Group; 2012 .
MIMS New Zealand. MIMS online. Available from URL: http://www.mims.co.nz/About.aspx (accessed September 2013).
Merry AF, Gibbs RD, Edwards J, et al. Combined acetaminophen and ibuprofen for pain relief after oral surgery in adults: a randomized controlled trial. Br J Anaesth 2010; 104: 80-8.
Brasher PM, Brant RF. Problems of multiplicity. Can J Anesth 2008; 55: 259-64.
Pierce CA, Voss B. Efficacy and safety of ibuprofen and acetaminophen in children and adults: a meta-analysis and qualitative review. Ann Pharmacother 2010; 44: 489-506.
Viitanen H, Tuominen N, Vaaraniemi H, Nikanne E, Annila P. Analgesic efficacy of rectal acetaminophen and ibuprofen alone or in combination for paediatric day-case adenoidectomy. Br J Anaesth 2003; 91: 363-7.
Gazal G, Mackie IC. A comparison of paracetamol, ibuprofen or their combination for pain relief following extractions in children under general anaesthesia: a randomized controlled trial. Int J Paediatr Dent 2007; 17: 169-77.
Pickering AE, Bridge HS, Nolan J, Stoddart PA. Double-blind, placebo-controlled analgesic study of ibuprofen or rofecoxib in combination with paracetamol for tonsillectomy in children. Br J Anaesth 2002; 88: 72-7.
Hannam J, Anderson BJ. Explaining the acetaminophen-ibuprofen analgesic interaction using a response surface model. Paediatr Anaesth 2011; 21: 1234-40.
Verburg KM, Maziasz TJ, Weiner E, Loose L, Geis GS, Isakson PC. Cox-2-specific inhibitors: definition of a new therapeutic concept. Am J Ther 2001; 8: 49-64.
Stinson JN, Kavanagh T, Yamada J, Gill N, Stevens B. Systematic review of the psychometric properties, interpretability and feasibility of self-report pain intensity measures for use in clinical trials in children and adolescents. Pain 2006; 125: 143-57.
Shields BJ, Palermo TM, Powers JD, Grewe SD, Smith GA. Predictors of a child’s ability to use a visual analogue scale. Child Care Health Dev 2003; 29: 281-90.
Brennan F, Carr DB, Cousins M. Pain management: a fundamental human right. Anesth Analg 2007; 105: 205-21.
Anderson BJ, Woollard GA, Holford NH. Acetaminophen analgesia in children: placebo effect and pain resolution after tonsillectomy. Eur J Clin Pharmacol 2001; 57: 559-69.
Anderson B, Cranswick N. The placebo (I shall please)—is it so pleasing in children? Paediatr Anaesth 2005; 15: 809-13.
Berntson L, Svensson E. Pain assessment in children with juvenile chronic arthritis: a matter of scaling and rater. Acta Paediatr 2001; 90: 1131-6.
Acknowledgements
We are grateful to the following individuals for their support: Drs. Shilpa Patel and Ajay Shah for administering the study protocol and data collection at the Indian sites and Ms. Elaine Davies and Ms. Jacqueline Hannam for administering the study protocol and data collection at the Auckland sites; Ms. Jacqueline Hannam also assisted with proofreading and editing the manuscript; A/Prof Brian Anderson for his contribution to the study design and for editing the manuscript; Professor Randall Morton, Dr. Niall Wilton, and Dr. Andrew Gunn for their contribution to patient recruitment and oversight of study processes; Dr. Hartley Atkinson, Dr. Amanda Potts, and Ms. Jennifer Zhang for managing the study database, providing support for the study sites, and reviewing and commenting on the manuscript. We are also grateful to the anesthetists and surgeons who provided clinical care for the children and especially to the children and their families for their participation.
Funding
The study was sponsored by AFT Pharmaceuticals Ltd. Dr. Edwards was supported by funding from the Green Lane Research and Educational Fund and the Performance-Based Research Fund (PBRF), School of Medicine, University of Auckland.
Declaration of interests
The University of Auckland, Shravan ENT Hospital, and Niyati ENT Hospital received payment from the study sponsor to undertake this research. The sponsor contributed to protocol design, provided monitoring during the study, and maintained the trial database. The authors had complete access to all data. An independent statistician (C.F.) performed the analysis, which was cross-checked by the sponsors and the authors (A.F.M., K.E.). The sponsor reviewed the final draft of the manuscript and was allowed to make suggestions. The composition and content of the manuscript were determined entirely by the academic authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Alan F. Merry oversaw the study design and provided supervision of data collection at the Auckland sites. He inspected case report forms from all three sites, contributed to preparation of the final study report, and revised the manuscript. He also contributed to the response to reviewers. Alan F. Merry and Kylie-Ellen Edwards contributed to the analysis and interpretation of the data. Kylie-Ellen Edwards prepared the first draft of the manuscript and the first draft of the response to reviewers. Zahoor Ahmad, Colin Barber, and Murali Mahadevan contributed to patient recruitment, oversaw data collection, and provided clinical care of patients during their involvement in the study Chris Frampton provided input into the design of the study and undertook all statistical analyses. He assisted with the interpretation of the data and the statistical aspects of the final study report and was involved in drafting and editing the manuscript. Alan F. Merry, Kylie-Ellen Edwards, Zahoor Ahmad, Colin Barber, Murali Mahadevan, and Chris Frampton contributed to the final version of the manuscript.
Appendix
Appendix
100-mm horizontal visual analogue scale with modified Wong-Baker FACES as anchors

Rights and permissions
About this article
Cite this article
Merry, A.F., Edwards, KE., Ahmad, Z. et al. Randomized comparison between the combination of acetaminophen and ibuprofen and each constituent alone for analgesia following tonsillectomy in children. Can J Anesth/J Can Anesth 60, 1180–1189 (2013). https://doi.org/10.1007/s12630-013-0043-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-013-0043-3