Abstract
Purpose
In order to establish guidelines for the preparation of the Dräger Fabius GS™ premium anesthetic workstation for malignant hyperthermia-susceptible patients, the authors evaluated the effect of the workstation’s exchangeable and autoclavable components on the washout of isoflurane.
Methods
A Dräger Fabius GS™ workstation was primed with 1.5% isoflurane, and exchangeable components were replaced as follows: Group 1: no replacement (control); Group 2: autoclaved ventilator diaphragm and ventilator hose; Group 3: flushed ventilator diaphragm and ventilator hose; Group 4: autoclaved compact breathing system. The fresh gas flow (FGF) was set at 10 L · min−1, and the concentration of isoflurane in the inspiratory limb of the circle breathing circuit was recorded every minute until an endpoint of 5.0 parts per million (ppm) was achieved, at which time the FGF was reduced to 3 L · min−1. Six experiments were conducted in each of the four groups.
Results
The time to achieve an isoflurane concentration of 5.0 ppm decreased in the following order: Group 1 (151 ± 17 min) > Group 3 (137 ± 7 min) > Group 4 (122 ± 11 min) > Group 2 (42 ± 6 min) (P < 0.01 vs control). Isoflurane concentration increased approximately fivefold when the FGF was reduced to 3 L · min−1.
Conclusion
Anesthetic washout from the Dräger Fabius GS™ is relatively slow. Although washout was accelerated when the Dräger Fabius GS™ was equipped with autoclaved components, the reduction in washout time may be less than that required for this technique to be accepted into clinical practice. A dedicated vapor-free workstation may be preferable for rapid turnover between cases.
Résumé
Objectif
Les auteurs ont évalué l’effet des composants échangeables et autoclavables du poste de travail anesthésique Dräger Fabius GS™ premium sur l’élimination d’isoflurane afin d’élaborer des lignes directrices pour la préparation du poste lors de la prise en charge de patients susceptibles de souffrir d’hyperthermie maligne.
Méthode
Un poste de travail Dräger Fabius GS™ a été préparé avec de l’isoflurane 1,5 %, et les composants échangeables ont été remplacés comme suit : Groupe 1 : aucun remplacement (témoin) ; Groupe 2 : autoclavage du diaphragme et du tuyau du ventilateur ; Groupe 3 : vidange du diaphragme et du tuyau du ventilateur ; Groupe 4 : autoclavage du système de ventilation compact. Le débit de gaz frais (DGF) a été établi à 10 L·min−1, et la concentration d’isoflurane dans la partie inspiratoire du circuit anesthésique a été enregistrée chaque minute jusqu’à l’obtention d’un seuil de 5,0 parties par million (ppm), moment auquel le DGF a été réduit à 3 L·min−1. Six expériences ont été réalisées dans chacun des quatre groupes.
Résultats
Le temps nécessaire à l’obtention d’une concentration d’isoflurane de 5,0 ppm a diminué dans l’ordre suivant : Groupe 1 (151 ± 17 min) > Groupe 3 (137 ± 7 min) > Groupe 4 (122 ± 11 min) > Groupe 2 (42 ± 6 min) (P < 0,01 vs témoin). La concentration d’isoflurane a approximativement quintuplé lorsque le DGF était réduit à 3 L·min−1.
Conclusion
L’élimination de l’anesthésique du poste de travail Dräger Fabius GS™ est relativement lent. Bien que l’élimination ait été accélérée lorsque le Dräger Fabius GS™ était équipé de composants autoclavables, la réduction du temps d’élimination pourrait néanmoins être moindre que ce qui est requis pour que cette technique soit acceptée dans la pratique clinique. Un poste de travail spécifique sans vapeur pourrait constituer une solution préférable pour un changement rapide entre les cas.
Similar content being viewed by others
Malignant hyperthermia (MH), a potentially fatal disorder of skeletal muscle metabolism, can be triggered in susceptible patients by exposure to volatile anesthetics. Guidelines for the preparation of anesthesia delivery systems for MH-susceptible patients include flushing the delivery system with vapor-free fresh gas in order to avoid exposing the patient to even trace concentrations of anesthetic vapor. Whereas older style anesthesia delivery systems could be effectively flushed in 10 min at high fresh gas flow (FGF), the current generation of anesthetic workstations can require considerably more time, perhaps owing in part to the complexity and composition of their internal breathing circuitry.1–3 For example, the time needed to effectively flush the Dräger Primus™ anesthetic workstation (Dräger, Lübeck, Germany) exceeded 1 h,3 which could result in considerable delays to the surgical schedule. These studies also showed that certain internal rubber or plastic components can act as reservoirs for volatile anesthetics, and that autoclaving these components greatly speeds anesthetic washout.3 Accordingly, when providing anesthetic care for the MH-susceptible patient, the workstation equipped with autoclaved components can be a cost-effective alternative to a dedicated vapor-free delivery system.3
The Dräger Fabius GS™ premium anesthetic workstation (Dräger, Lübeck, Germany) is currently marketed worldwide. Guidelines for the preparation of this workstation for MH-susceptible patients are lacking. While the Dräger Fabius GS™ and the Dräger Primus™ share certain characteristics, their internal breathing circuitries are not identical, consequently, their washout profiles may differ. We sought to evaluate the effect of the workstation’s exchangeable and autoclavable components (ventilator diaphragm, ventilator hose, and compact breathing system) on the washout of isoflurane.
Methods
The Dräger Fabius GS™ workstation was equipped with a 1.8-m long disposable circle breathing circuit (BOMImed, Winnipeg, MB, Canada) and a model lung. To simulate clinically relevant volatile anesthetic exposure, the workstation and circle breathing circuit were primed for 2 h with 1.5% isoflurane in air using a FGF of 3 L · min−1. During priming, the model lung was ventilated with a tidal volume of 500 mL and a rate of 15 breaths per min. At completion of priming, the workstation was set at the “stand-by” mode and the FGF was discontinued. After that, the vaporizer was removed; the carbon dioxide absorber canister, circle breathing circuit, model lung, and reservoir bag were replaced with components that had never been exposed to volatile anesthetics; and fresh Amsorb® (Armstrong Medical, Coleraine, Northern Ireland) was placed in the carbon dioxide absorber canister.
To determine the effect of the workstation’s exchangeable components (the ventilator diaphragm, ventilator hose, and the compact breathing system) on the washout of isoflurane, six experiments were conducted in each of the following groups:
-
Group 1: None of the workstation’s exchangeable components was replaced (control group).
-
Group 2: The ventilator diaphragm and ventilator hose were removed and were replaced with components that had been autoclaved at 132°C for 10 min.
-
Group 3: As an additional control for Group 2, the ventilator diaphragm and ventilator hose were removed, were air-blown thoroughly with a forced-air gun, and were reattached without being autoclaved.
-
Group 4: The compact breathing system was removed and was replaced with one that had been autoclaved at 132°C for 10 min.
Immediately afterward, the FGF was set at 10 L · min−1 and ventilation was restarted using the same tidal volume and respiratory rate as for the priming phase. A calibrated Miran SapphIRe 205B Series Portable Ambient Air Analyzer™ (Thermo Fisher Scientific Inc., Waltham, MA, USA) was used to measure the concentration of isoflurane in the inspiratory limb of the circle breathing circuit every minute until an endpoint of 5.0 parts per million (ppm) was achieved. This device has an accuracy of ±5% and a sensitivity of 0.1 ppm. Before each experiment, a zero calibration was performed in an environment free of volatile agent. The washout time for isoflurane was defined as the time from initiating a FGF of 10 L · min−1 until a concentration of 5.0 ppm was achieved in the inspiratory limb of the circle breathing circuit (early washout phase). When the isoflurane concentration reached 5.0 ppm, the FGF was reduced to 3 L · min−1, and the recording continued for one hour or until the isoflurane concentration again reached 5.0 ppm, whichever came first (late washout phase). All experiments were conducted on a single workstation that had never been in clinical use.
Statistical analysis
Data are expressed as mean ± SD. One-way ANOVA and Dunnett’s post hoc test were used to compare washout times for isoflurane. P < 0.05 was considered statistically significant.
Results
Early washout phase
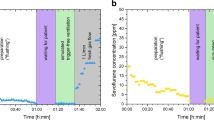
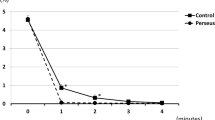
Isoflurane concentration in the inspiratory limb of the circle breathing circuit decreased exponentially during the early washout phase in all groups (Fig. 1). Washout times are summarized in the Table 1. In Group 1 (control), isoflurane concentration decreased to 5.0 ppm after 151 ± 17 min of washout. In Group 2, replacing the ventilator diaphragm and ventilator hose with autoclaved components accelerated the washout of isoflurane approximately fourfold. The time to achieve an isoflurane concentration of 5.0 ppm was significantly shorter in Group 2 (42 ± 6 min) compared with the control group (P < 0.01). In Group 3, flushing the ventilator diaphragm and ventilator hose with forced air did not achieve as rapid a washout compared with using autoclaved components. The washout time in Group 3 (137 ± 7 min) did not differ significantly compared with control. Similarly, using an autoclaved compact breathing system in Group 4 only moderately accelerated the early washout phase (122 ± 11 min) compared with control (P < 0.01).
Late washout phase
A rebound increase in isoflurane concentration was observed when the FGF was reduced to 3 L · min−1 (late washout phase) in all groups (Table 1, Fig. 2). Group 2 showed the largest rebound, reaching 46 ± 6 ppm (P < 0.01 compared with control). During the late washout phase, the isoflurane concentration did not return to 5.0 ppm or less in any group.
Late washout profiles for isoflurane in the Dräger Fabius GS™ anesthetic workstation. When the FGF was reduced from 10–3 L · min−1 (late washout phase), a four- to tenfold increase in the concentration of isoflurane in the inspiratory limb of the breathing circuit was observed. Data are mean ± SD, ppm parts per million
Discussion
The results show that the washout of isoflurane from the Dräger Fabius GS™ premium is relatively slow when compared with other current-generation anesthesia workstations.1–3 The washout time needed to achieve an isoflurane concentration of 5.0 ppm in the breathing circuit of the Dräger Fabius GS™ is more than double that reported for the Dräger Primus™ workstation.3 The use of autoclaved ventilator components accelerated the washout of isoflurane fourfold but did not achieve as rapid a washout as that observed in the Dräger Primus™ workstation.3
A factor influencing washout time is the absorption and subsequent release of volatile anesthetics from rubber and plastic components that comprise the workstation’s internal circuitry.4 Factors affecting the rate of absorption include the solubility of the anesthetic, its concentration, and the duration of exposure,5–7 all of which were standardized in this study. Anesthetic solubility in rubber, including silicone, exceeds that in most plastics.8–10 The breathing system circuitry internal to the Dräger Fabius GS™ workstation comprises silicone and is probably a site of considerable anesthetic absorption. Whereas flushing is effective in removing volatile anesthetics from latex and polysulfone tubing, only autoclaving has been found to be effective in removing volatile anesthetics from silicone.8 This is consistent with our observation that autoclaving, but not forced air flushing, accelerated the washout of isoflurane. Slow washout, despite the use of an autoclaved ventilator diaphragm and ventilator hose, may be attributed in part to anesthetic absorption by non-exchangeable components.
Another factor influencing washout may be fresh gas decoupling,11 a mechanism that is utilized in the Dräger Fabius GS™ to prevent the dependency of tidal volume on FGF. During the inspiratory phase of positive pressure ventilation, the ventilator and the inspiratory part of the internal circuitry are decoupled from the fresh gas, which passes to the reservoir bag via the carbon dioxide absorber and is subsequently fed in expiration, together with the stored volume, directly into the breathing system via a non-return valve (fresh gas decoupling valve). Accordingly, the inspiratory limb of the internal breathing system circuitry is flushed only intermittently during the respiratory cycle, suggesting that it might act as a reservoir for volatile anesthetics.
Replacing the compact breathing system of the Dräger Fabius GS™ had little effect on the washout of isoflurane. Replacing the compact breathing system is cumbersome and time consuming and involves removing and reattaching the fresh gas tubing, ventilator hose, waste gas outlet port, flexible arm and re-breathing bag, pressure sensor, pressure gauge, oxygen sensor, flow sensor, adjustable pressure limiting bypass valve, and positive end-expiratory pressure hoses. Even with practice, this procedure took more than 10 min to complete.
In previous studies, the endpoint for anesthetic washout has been variable, ranging from 1 to 10 ppm.1,12,13 These results reflect the fact that the minimum concentration of volatile anesthetic needed to trigger an MH reaction in humans is unknown. We chose an end-point concentration of 5.0 ppm because evidence suggests that MH-susceptible swine do not develop MH when exposed to an anesthetic concentration of 5.0 ppm (Denise Wedel MD, Mayo Clinic, Rochester, Minnesota, October 2, 2006, personal communication).
To simulate the clinical situation, we reduced the FGF to 3 L · min−1 after the early washout phase. The resulting rebound increase in isoflurane concentration was greatest when the ventilator diaphragm and ventilator hose were replaced with autoclaved components. This may be attributed in part to the shorter time required to flush the workstation in these studies, allowing non-exchangeable internal components that had become saturated with anesthetic vapor during priming to subsequently release a greater amount of isoflurane into the circuitry when the FGF was reduced. This supports the notion that volatile anesthetics are absorbed by various workstation components and subsequently released into the breathing circuitry. To avoid unintentional exposure of the MH-susceptible patient to anesthetic concentrations greater than 5.0 ppm, we recommend maintaining the FGF at the level used to flush the workstation for the duration of anesthesia.
Isoflurane washout time took as long as 50 min, even with the use of an autoclaved ventilator diaphragm and ventilator hose. A washout period of this duration may not be acceptable for most clinical situations, particularly when rapid turnover between cases is required. Using a dedicated vapor-free anesthetic workstation may be indicated in such situations, although replacing the workstation during the surgical schedule is itself time consuming. When time permits, the ventilator diaphragm and ventilator tubing can be replaced with autoclaved components, and the workstation can be flushed using a FGF of 10 L · min−1 for 50 min. These components can be stocked specifically for use with MH-susceptible patients and autoclaved after each use. It is often difficult to justify the cost of a vapor-free workstation given the infrequency of their use. At our institution, it is estimated that a dedicated vapor-free workstation requires 50 h of labor per year for regular maintenance and annual servicing. Given their relative costs, using autoclaved components is an economical alternative to a dedicated MH anesthetic workstation.
A limitation of the study is that only one volatile anesthetic was analyzed. The washout of sevoflurane was nearly identical to that of isoflurane in the Dräger Primus™ workstation,2 although it cannot be assumed that the same findings apply to the Dräger Fabius™ workstation.
A clear understanding of the washout characteristics of the anesthesia workstation is required to avoid unintentional exposure of the MH-susceptible patient to volatile anesthetics. This study highlights that the washout of volatile anesthetic agent varies depending on the anesthesia delivery system. Guidelines for the preparation of current-generation anesthetic workstations for the MH-susceptible patients must be specific for the workstation. It is incumbent on manufacturers to consider factors influencing volatile anesthetic washout in the design and manufacture of anesthetic workstations.
References
Petroz GC, Lerman J. Preparation of the Siemens KION anesthetic machine for patients susceptible to malignant hyperthermia. Anesthesiology 2002; 96: 941–6.
Prinzhausen H, Crawford MW, O’Rourke J, Petroz GC. Preparation of the Drager Primus anesthetic machine for malignant hyperthermia-susceptible patients. Can J Anesth 2006; 53: 885–90.
Crawford MW, Prinzhausen H, Petroz GC. Accelerating the washout of inhalational anesthetics from the Drager Primus anesthetic workstation: effect of exchangeable internal components. Anesthesiology 2007; 106: 289–94.
Eger EI II, Larson CP Jr, Severinghaus JW. The solubility of halothane in rubber, soda lime and various plastics. Anesthesiology 1962; 23: 356–9.
Folkman J, Long DM Jr, Rosenbaum R. Silicone rubber: a new diffusion property useful for general anesthesia. Science 1966; 154: 148–9.
Lowe HJ, Titel JH, Hagler KJ. Absorption of anesthetics by conductive rubber in breathing circuits. Anesthesiology 1971; 34: 283–92.
Lockwood GG, Chakrabarti MK, Whitwam JG. An evaluation of anaesthetic loss from a closed breathing system. Anaesthesia 1993; 48: 564–7.
Gilly H, Weindlmayr-Goettel M, Koberl G, Steinbereithner K. Anaesthetic uptake and washout characteristics of patient circuit tubing with special regard to current decontamination techniques. Acta Anaesthesiol Scand 1992; 36: 621–7.
Marx T, Froba G, Bader S, Villwock J, Georfieff M. Diffusion of anaesthetic gases through different polymers. Acta Anaesthesiol Scand 1996; 40: 275–81.
Smith C, Flynn C, Wardall G, Broome IJ. Leakage and absorption of isoflurane by different types of anaesthetic circuit and monitoring tubing. Anaesthesia 2002; 57: 686–9.
Primus Anesthetic Workstation Technical Documentation, Revision 3.0. Lübeck, Germany: Dräger Medical; 2003. p. 68–70.
Beebe JJ, Sessler DI. Preparation of anesthesia machines for patients susceptible to malignant hyperthermia. Anesthesiology 1988; 69: 395–400.
Schonell LH, Sims C, Bulsara M. Preparing a new generation anaesthetic machine for patients susceptible to malignant hyperthermia. Anaesth Intensive Care 2003; 31: 58–62.
Acknowledgements
The authors thank the Occupational Health and Safety Services, The Hospital for Sick Children, Toronto, ON, Canada for their generous loan of the Miran SapphIRe 205B Series Portable Ambient Air Analyzer™ (Thermo Fisher Scientific Inc., Waltham, MA, USA). We gratefully acknowledge the technical assistance of Mr. Keith Mathews RTT, Department of Anesthesia, The Hospital for Sick Children, Toronto, Ontario, Canada and Mr. Rocky Yang BASc, Department of Medical Engineering, The Hospital for Sick Children, Toronto, ON, Canada.
Potential competing interests
Funded in part by a grant from Dräger, Lübeck, Germany to Dr. Crawford. No author has competing interests related to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Whitty, R.J., Wong, G.K., Petroz, G.C. et al. Preparation of the Dräger Fabius GS™ workstation for malignant hyperthermia-susceptible patients. Can J Anesth/J Can Anesth 56, 497–501 (2009). https://doi.org/10.1007/s12630-009-9097-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-009-9097-7