Abstract
Objectives
to validate the MSRA questionnaire proposed as prescreening tool for sarcopenia, in a population of community-dwelling elderly subjects.
Design
observational study.
Setting
community dwelling elderly subjects.
Participants
274 community dwelling elderly subjects, 177 women and 97 men, aged 66-78 years.
Measurements
Based on EWGSOP diagnostic criteria subjects were classified as sarcopenic and nonsarcopenic. The Mini Sarcopenia Risk Assessment (MSRA) questionnaire, is composed of seven questions and investigates anamnestic and nutritional characteristics related to risk of sarcopenia onset (age, protein and dairy products consumption, number of meals per day, physical activity level, number of hospitalizations and weight loss in the last year).
Results
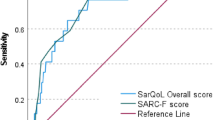
33.5% of the study population, were classified as sarcopenic. With the 7-item MSRA score, subjects with a score of 30 or less, had a 4-fold greater risk of being sarcopenic than subjects with a score higher than 30 (OR:4.20;95% CI:2.26–8.06); area under the ROC curve was 0.786 (95% CI:0.725-0.847). In a logistic regression, considering as dependent variable the probability of being sarcopenic, and as independent variables the 7 items of the questionnaire, two items (number of meals and milk and dairy products consumption) showed non-significant diagnostic power. A 5-item score was then derived and the area under the ROC curve was 0.789 (95% IC:0.728-0.851). Taking into account the cost of false positive and false negative costs and the prevalence of sarcopenia, the “optimal” threshold of the original MSRA score (based on 7 items) is 30, with a sensitivity of 0.804 and a specificity of 0.505, while the “optimal” threshold of the MSRA score based on 5 items, is 45, with a sensitivity of 0.804 and a specificity of 0.604.
Conclusion
this preliminary study shows that the MSRA questionnaire is predictive of sarcopenia and can be suggested as prescreening instrument to detect this condition. The use of a short form of the MSRA questionnaire improves the capacity to identify sarcopenic subjects.


Similar content being viewed by others
References
Crutz-Jentoft AJ, Baeyens JP, Bauer JM, Boire Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkovà E, Vandewoude M, Zamboni M. Sarcopenia: European consensus on definition and diagnosis. Report of the European Working Group on Sarcopenia in Older People. Age and Aging. 2010;39: 412–23.
Janssen I, Shepard DS, Katzmarzyc PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatrc Soc 2004;52: 80–85.
Rolland Y, Czerwinski S, Abellan van Kan G, Morley JE, Cesari M, Onder G, Woo J, Baumgartner R, Pillard F, Boirie Y, Chumlea WMC, Vellas B. Sarcopenia: Its assessment, etiology, pathogenesis, consequences and future perspectives. J Nutr Health Aging. 2008 Aug-Sep; 12: 433–450.
Rossi AP, Fantin F, Micciolo R, Bertocchi M, Bertassello P, Zanandrea V, Zivelonghi A, Bissoli L, Zamboni M. Identifying sarcopenia in acute care setting patients. J Am Med Dir Assoc 2014; 15: 303.e7–12.
Landi F, Liperoti R, Fusco D, Mastropaolo S, Quattrociocchi D, Proia A, Russo A, Bernabei R, Onder G. Prevalence and risk factors of sarcopenia among nursing home older residents. J Gerontol A Biol Sci Med Sci. 2012;67: 48–55.
Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. 2013;14: 531–2.
Woo J, Leung J, Morley JE. Validating the SARC-F: a suitable community screening tool for sarcopenia? J Am Med Dir Assoc. 2014;15: 630–4.
Zamboni M, Turcato E, Santana H, Maggi S, Harris TB, Pietrobelli A, Heymsfield SB, Micciolo R, Bosello O. The relationship between body composition and physical performance in older women. J Am Geriatr Soc 1999;47: 1403–8.
Rossi AP, Fantin F, Caliari C, Zoico E, Mazzali G, Zanardo M, Bertassello P, Zanandrea V, Micciolo R, Zamboni M. Dynapenic abdominal obesity as predictor of mortality and disability worsening in older adults: A 10-year prospective study. Clin Nutr. 2016; 35: 199–204.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 1998;147: 755–763.
Istituto Nazionale della Nutrizione. Tabelle di composizione degli alimenti. (National Institute of Nutrition: tables of nutritional composition). Litho Delta: Milano, 1989 (in Italian)
Budui SL, Rossi AP, Zamboni M. The pathogenetic bases of sarcopenia. Clin Cases Miner Bone Metab. 2015;12: 22–6.
Kortebein P, Ferrando A, Lombeida J, Wolfe R, Evans WJ. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA 2007;297: 1769–1774.
Evans WJ. Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr 2010, 91(suppl): 1123–75.
Renoud A, Ecochard R, Marchand F, Chapulart R, Szulc P. Predictive parameters of accelerated muscle loss in men-MINOS Study. The American Journal of Medicine 2014;127: 554–61.
Alley D, Koster A, Mackey D, Cawthon P, Ferrucci L, Simonsick EM, Yu B, Hardy S, Goodpaster B, Sarkisian C, Houston DK, Kritchevsky SB, Cummings S, Lee JS, Tylavsky FA, Newman A, Harris T. Hospitalization and change in body composition and strength in a population-based cohort of older persons. J Am Geriatr Soc. 2010;58: 2085–91.
Abellan van Kan. G. Epidemiology and consequences of sarcopenia. J Nutr Health Aging 2009;13: 708–712.
Houston DK, Nicklas BJ, Ding J, Harris TB, Tylavsky FA, Newman AB, Sun Lee J, Sahyoun NR, Visser M, Kritchevsky SB. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: The Health Aging and Body Composition Study. Am J Clin Nutr 2008;87: 150–5.
Filion ME, Barbat-Artigas S, Dupontgand S, Fex A, Karelis AD, Aubertin-Leheudre M. Relationship between protein intake and dynapenia in postmenopausal women. J Nutr Health Aging 2012;16: 616–619.
Molino S, Dossena M, Buonocore D, Verri M. Sarcopenic Obesity: An Appraisal of the Current Status of Knowledge and Management in Elderly People. J Nutr Health Aging. 2016;20: 780–8.
Fawcett T. An introduction to ROC analysis. Pattern Recogn Lett. 2006, 27:861–874.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44: 837–845.
Zhou X.H, Obuchowski N.A., McClish D.K. (2011) Statistical Methods in Diagnostic Medicine. 2nd edition. John Wiley & Sons, New York.
Zweig MH, Campbell G. Receiver-Operating Characteristic (ROC) Plots: A Fundamental Evaluation Tool in Clinical Medicine. Clin Chem 1993;39: 561–577.
Mijnarends DM, Schols JMGA, Halfens RJG, Meijers JMM, Luiking, YC, Verlaane S, Evers SMAA. Burden-of-illness of Dutch community-dwelling older adults with sarcopenia: Health related outcomes and costs. Eur J Geriatr 2016;7: 276–284.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing 2014, Vienna, Austria.
Robin, N. Turck, A. Hainard, N. Tiberti, F. Lisacek, J.C. Sanchez, M. Müller, pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 2011; 12:77.
Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Muscle Wasting 2016;7: 28–36.
Barbosa-Silva TG, Menezes AM Bielemann RM, Malmstrom TK, Gonzalez MC. Enhancing the SARC-F: improving sarcopenia screening in the clinical practice. J Am Med Dir Assoc 2016; S1525-8610, 30314–0.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rossi, A.P., Micciolo, R., Rubele, S. et al. Assessing the risk of sarcopenia in the elderly: The Mini Sarcopenia Risk Assessment (MSRA) questionnaire. J Nutr Health Aging 21, 743–749 (2017). https://doi.org/10.1007/s12603-017-0921-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-017-0921-4