Abstract
Introduction
Malnutrition is a frequent condition in the elderly especially in hospitals and in nursing homes, and even among the free-living elders the prevalence is not negligible (5-10%). Awareness towards malnutrition is still limited. The lack of time for nutritional assessment by the overcommitted healthcare personnel, including the general practitioners (GPs), may represent one possible explanation for limited recognition of malnutrition. Therefore, a self-administered instrument could be useful in raising alert on the GPs and allow early detection of malnutrition and early care provision. The aim of the present study was to analyze the validity of the Self-MNA that takes cue from the Mini Nutritional Assessment-Short Form (MNA-SF) and has been adapted to be self-administered by free-living elderly subjects.
Methods
Participants were recruited from patients referring to the GP offices in Italy. Nutritional evaluation was performed through the administration of Full-MNA, MNA-SF and Self-MNA. The comorbidity level was assessed through the Cumulative Illness Rating Scale (CIRS). The level of difficulty in filling out the test was reported by the participants, and the time spent to complete the Self-MNA was also registered.
Results
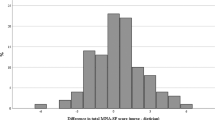
A total of 226 subjects, 125 women and 101 men (75.1 ± 8 and 75.3 ± 8 years old, respectively; p=0.89) were enrolled, and 214 (94.7%) of them completed the Self-MNA. According with the Full-MNA test score, 8.4% of women and 3.5% of men were classified as malnourished, whereas 32.7% of women and 31.4% of men were at risk of malnutrition. Agreement between Self-MNA and Full-MNA, and Self-MNA vs. MNA-SF was classified as “moderate” (k = 0.476 and 0.496 respectively; p < 0.001). Self-MNA showed a fair predictive value compared to the Full-MNA and MNA-SF tests (76.6 and 79.9%, respectively) with a barely adequate sensitivity (70.9 and 75.4%, respectively). The analysis of the characteristics of FN (false negative: subjects who were considered at risk of malnutrition or malnourished at Full-MNA but not at Self-MNA) showed that the clinical and functional aspects of these subjects (age, comorbidity and severity, time necessary to complete the Self-MNA, decrease in food intake, severe illness in the past 3 months, dementia and depression, fluid intake, need for feeding assistance, arm and calf circumferences) were very similar to the characteristics of true positive subjects. Patients required 6.7 ± 4.5 minutes to complete the test and 25 subjects (11.7%) needed more than 10 minutes, up to a maximum of 30 minutes. Patients who stated a greater difficulty were older (79.8 ± 7 vs. 73.5 ± 7 years; p< 0.001), they were more «malnourished» at Full-MNA (10.7 vs. 1,7%; p= 0.006) and clinical status was characterized by a higher severity index (1.72 ± 0.6 vs. 1.41 ± 0.4; p= 0.008).
Conclusion
In the present study we investigated the validity of the Self-MNA in a sample of free-living elderly subjects. The results obtained confirm the validity of the test that may represent a useful tool for the GPs, although some important limitations need to be considered, limiting its use in clinical practice.



Similar content being viewed by others
References
Cereda E, Pedrolli C, Klersy C, Bonardi C, Quarleri L, Cappello S, Turri A, Rondanelli M, Caccialanza R. Nutritional status in older persons according to healthcare setting: A systematic review and meta-analysis of prevalence data using MNA(®). Clin Nutr. 2016 Apr 6. pii: S0261-5614(16)00099-6.
Schrader E, Grosch E, Bertsch T, Sieber CC, Volkert D. Nutritional and Functional Status in Geriatric Day Hospital Patients-MNA Short Form Versus Full MNA. J Nutr Health Aging. 2016;20: 918–926
Vellas B, Lauque S, Andrieu S, Nourhashemi F, Rolland Y, Baumgartner R, Garry P. Nutrition assessment in the elderly. Curr Opin Clin Nutr Metab Care. 2001 Jan;4(1):5–8.
de van der Schueren MA, Wijnhoven HA, Kruizenga HM, Visser M. A critical appraisal of nutritional intervention studies in malnourished, community dwelling older persons. Clin Nutr. 2015 Dec 29. pii: S0261–5614(15)00351-9.
Kaiser MJ, Bauer JM, Ramsch C, et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010;58: 1734–1738.
Donini LM, Poggiogalle E, Piredda M, Pinto A, Barbagallo M, Cucinotta D, Sergi G. Anorexia and eating patterns in the elderly. PLoS One. 2013; 8: e63539.
Lattanzio F, Laino I, Pedone C, Corica F, Maltese G, Salerno G, Garasto S, Corsonello A, Incalzi RA; on behalf of the Pharmaco surVeillance in the elderly Care (PVC) Study Group. Geriatric Conditions and Adverse Drug Reactions in Elderly Hospitalized Patients. J Am Med Dir Assoc. 2012;13: 96–9.
Torheim LE, Ferguson EL, Penrose K, Arimond M. Women in resource-poor settings are at risk of inadequate intakes of multiple micronutrients. J Nutr. 2010;140:2051S–8S.
Hassen TA, Pearson S, Cowled PA, Fitridge RA. Preoperative nutritional status predicts the severity of the Systemic Inflammatory Response Syndrome (SIRS) following major vascular surgery. Eur J Vasc Endovasc Surg 2007;33: 696–702.
Schneider SM, Veyres P, Pivot X, Soummer AM, Jambou P. Malnutrition is an independent factor associated with nosocomial infections. Br J Nutr 2004;92: 105–111.
Donini LM, De Felice MR, Tagliaccica A, De Bernardini L, C Cannella. Nutritional status and evolution of pressure sores in geriatric patients. J Nutr Health Aging 2005; 9 (6): 446–454
Donini LM, De Felice MR, Cannella C. Nutritional status determinants and cognition in the elderly. Arch Gerontol Geriatr 2007; Suppl 1:143–153.
Grieger JA, Nowson CA, Ackland LM. Nutritional and functional status indicators in residents of a long-term care facility. J Nutr Elder 2009;28: 47–60.
Friedmann JM, Jensen GM, Smicklas-Wright J, McCamish MA. Initial malnutrition predicting early non-elective hospital readmission in nutritionally compromised older adults. Am J Clin Nutr 1997;65: 1714–20.
Muscaritoli M, Molfino A. Malnutrition: the hidden killer in healthcare systems. BMJ. 2013; 346:f1547.
van Wissen J, van Stijn MF, Doodeman HJ, Houdijk AP. Mini Nutritional Assessment and Mortality after Hip Fracture Surgery in the Elderly. J Nutr Health Aging. 2016;20(9):964–968
Elia M, Stratton RJ. Considerations for screening tool selection and role of predictive and concurrent validity. Curr Opin Clin Nutr Metab Care 2011; 14: 425–433.
Donini LM, De Bernardini L, De Felice MR, Savina C, Coletti C. Effect of nutritional status on clinical outcome in a population of geriatric rehabilitation patients. Aging Clin Exper Res 2004;16: 132–8
Pirlich M, Schutz T, Norman K, Gastell S, Lubke HJ. The German hospital malnutrition study. Clin Nutr 2006;25: 563–572.
Stratton RJ, Elia M. Deprivation linked to malnutrition risk and mortality in hospital. Br J Nutr 2006; 96(5): 870–6
Kubrak C, Jensen L. Malnutrition in acute care patients: a narrative review. Int J Nurs Studies 2007;44: 1036–1054.
Hassan A, Ramadan M, Abdel-Rahman MO, Kerkadi A. Prevalence of undernutrition in a long-term care facility in Qatar. J Nutr Elder 2009; 28(3): 313–22.
Cereda E, Pedrolli C, Zagami A, Vanotti A, Piffer S. Body mass index and mortality in institutionalized elderly. J Am Med Dir Assoc 2001; 12(3): 174–8.
Guigoz Y, Vellas B, Garry PJ. Mini nutritional assessment: a practical assessment tool for grading the nutritional status of elderly patients. Facts Res Gerontol 1994; Suppl 2:15–59.
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, van Gossum A, Klek S, Muscaritoli M, Nyulasi I, Ockenga J, Schneider SM, de van der Schueren MA, Singer P. Diagnostic criteria for malnutrition -An ESPEN Consensus Statement. Clin Nutr. 2015;34: 335–40.
Schönherr S, Halfens RJG, Meijers JMM, Schols JMGA, Lohrmann C: Structural and process indicators of nutritional care: A comparison between Austrian hospitals and nursing homes. Nutrition 2012; 28: 868–873.
Söderhamn, U., Dale, B., Sundsli, K., & Söderhamn, O. (2012). Nutritional screening of older home-dwelling Norwegians: a comparison between two instruments. Clin Interv Aging. 2012;7: 383–91.
Hamirudin AH, Charlton K, Walton K, Bonney A, Potter J, Milosavljevic M, Hodgkins A, Albert G, Ghosh A, Dalley A. Feasibility of implementing routine nutritional screening for older adults in Australian general practices: a mixed-methods study. BMC Fam Pract. 2014 Nov 25;15:186.
Huhmann MB, Perez V, Alexander DD, Thomas DR. A self-completed nutrition screening tool for community-dwelling older adults with high reliability: a comparison study. J Nutr Health Aging. 2013;17: 339–44.
Rubenstein LZ, Harker JO, Salva A et al. Screening for undernutrition in geriatric practice: Developing the short-form Mini-Nutritional Assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 2001; 56A: M366–372.
Kaiser MJ, Bauer JM, Uter W, Donini LM, Stange I, Volkert D, Diekmann R, Drey M, Bollwein J, Tempera S, Guerra A, Ricciardi LM, Sieber CC. Prospective validation of the modified mini nutritional assessment short-forms in the community, nursing home, and rehabilitation setting. J Am Geriatr Soc. 2011;59: 2124–8
Parmelee PA, Thuras PD, Katz IR, Lawton MP. Validation of the Cumulative Illness Rating Scale in a geriatric residential population. J Am Geriatr Soc 1995;43: 130–137.
Galen R, Gambino S. The Predictive Value and Efficiency of Medical Diagnosis. John Wiley: New York (USA), 1975.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–74.
Moore BE, Friedman BJ, Crixell SH: Usability of the Self-Mini Nutritional Assessment among Older Adults Receiving Home-delivered Meals in Texas. Family & Consumer Sci Res J 2015;44: 159–171.
Pfrimer K, Vilela M, Resende CM, Scagliusi FB, Marchini JS, Lima NK, Moriguti JC, Ferriolli E. Under-reporting of food intake and body fatness in independent older people: a doubly labelled water study. Age Ageing. 2015;44: 103–8.
Gemming L, Jiang Y, Swinburn B, Utter J, Mhurchu CN. Under-reporting remains a key limitation of self-reported dietary intake: an analysis of the 2008/09 New Zealand Adult Nutrition Survey. Eur J Clin Nutr. 2014;68: 259–64.
Törmä J, Winblad U, Cederholm T, Saletti A. Does undernutrition still prevail among nursing home residents? Clin Nutr 2013; 32: 562–8.
Donini LM, Savina C, Rosano A, Cannella C. Systematic review of nutritional status evaluation and screening tools in the elderly. J Nutr Health Aging. 2007;11: 421–32.
Beck AM, Gøgsig Christensen A, Stenbæk Hansen B, Damsbo-Svendsen S, Kreinfeldt Skovgaard Møller T, Boll Hansen E, Keiding H. Study protocol: costeffectiveness of multidisciplinary nutritional support for undernutrition in older adults in nursing home and home-care: cluster randomized controlled trial. Nutr J. 2014; 13: 86.
Stratton RJ, Hackston A, Longmore D, Dixon R, Price S, Stroud M, King C, Elia M. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘Malnutrition Universal Screening Tool (‘MUST’) for adults. Br J Nutr 2004;92: 799–808.
Raslan M, Gonzalez MC, Gonçalves Dias MC, Nascimento M, Castro M, Marques P, Segatto S, Torrinhas RS, Cecconello I, Linetzky Waitzberg D: Comparison of nutritional risk screening tools for predicting clinical outcomes in hospitalized patients. Nutrition 2010; 26: 721–726.
Donini LM, Poggiogalle E, Molfino A, Rosano A, Lenzi A, Rossi Fanelli F, Muscaritoli M. Mini-Nutritional Assessment, Malnutrition Universal Screening Tool, and Nutrition Risk Screening Tool for the Nutritional Evaluation of Older Nursing Home Residents. J Am Med Dir Assoc. 2016 Aug 12. pii: S1525-8610(16)30246-8.
Donini LM, Savina C, Gennaro E, De Felice MR, Rosano A, Pandolfo MM, Del Balzo V, Cannella C, Ritz P, Chumlea WC.: A Systematic Review of the Literature Concerning the Relationship between Obesity and Mortality in the Elderly. J Nutr Health Aging. 2012;16: 89–98.
Donini LM, Ricciardi LM, Neri B, Lenzi A, Marchesini G.: Risk of malnutrition (over and under-nutrition): Validation of the JaNuS screening tool. Clin Nutr 2014;33: 1087–1094.
Donini LM, Poggiogalle E, Migliaccio S, Pinto A, Lubrano C, Lenzi A: Sarcopenic Obesity: Correlation with Clinical, Functional, and Psychological Status in a Rehabilitation Setting. Food & Nutr Sci, 2014;5: 2020–2031.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
WM and LMD designed the study and wrote the manuscript; the members of the Research Group of the SIMPeSV collected the data; CM and LMD analyzed the data; AL contributed to the critical revision of the manuscript
Vito Albano, Lucia Auriemma, Giuseppe Bariletto, Francesco Bellani, Giuseppe Nicodemo Bombardiere, Carla Bruschelli, Maria Grazia Rita Cadeddu, Barbara Cogorno, Rosario Salvatore Di Modica, Fernando Gori, Daniela Livadiotti, Giulia Marini, Matteo Marolla, Serafina Mastroianni, Maria Felicia Mocerino, Antonella Monaco, Francesco Filippo Morbiato, Sauro Omenetti, Tiziana Panzera, Elisabetta Pelini, Sara Petruzzi, Maurizio Pirro, Italo Guido Ricagni, Franco Roscilli, Pietro Scalera, Guido Alberto Siviero, Francesco Vaccaro.
Rights and permissions
About this article
Cite this article
Donini, L.M., Marrocco, W., Marocco, C. et al. Validity of the Self-Mini Nutritional Assessment (Self-MNA) for the Evaluation of Nutritional Risk. A Cross-Sectional Study Conducted in General Practice. J Nutr Health Aging 22, 44–52 (2018). https://doi.org/10.1007/s12603-017-0919-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-017-0919-y